Measure Descriptions for Daily Early Mobility: Slide Presentation
AHRQ Safety Program for Mechanically Ventilated Patients
Slide 1: AHRQ Safety Program for Mechanically Ventilated Patients
Measure Descriptions for Daily Early Mobility
Slide 2: Learning Objectives
After this session, you will be able to—
- Collect and enter daily early mobility data using the Daily Early Mobility Data Collection Tool.
- Understand the definitions of the data elements.
- Locate the necessary data elements.
Slide 3: Daily Early Mobility: Key Interventions
- Use multidisciplinary and coordinated approach.
- Interrupt sedation daily and minimize sedative use.
- Assess sedation and delirium with structured scales.
- Screen for highest level of mobilization.
- Employ a nurse-driven protocol to achieve highest level of mobility.
Slide 4: Data Collection

- Drives quality improvement efforts.
- Can be used for quality improvement processes or for research.
- Provides quantifiable measures of care practices.
- Guides patient safety conversations.
- Justifies resource allocations:
- Human resources (time).
- Financial resources (money).
- Supplies and equipment (stuff).
Slide 5: Daily Early Mobility Data Collection Tool
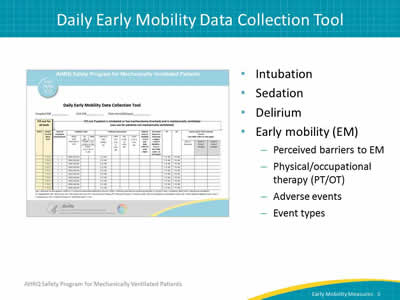
Image: The Daily Early Mobility Data Collection Tool.
- Intubation.
- Sedation.
- Delirium.
- Early mobility (EM):
- Perceived barriers to EM.
- Physical/occupational therapy (PT/OT).
- Adverse events.
- Event types.
Slide 6: Data Collection: Intubation, Sedation, and Delirium
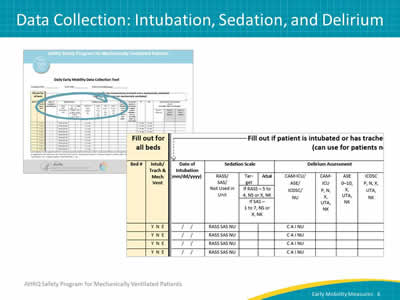
Images: The Daily Early Mobility Data Collection Tool. Detail view of the intubation, sedation, and delirium columns of the data collection tool.
Slide 7: Let’s Begin
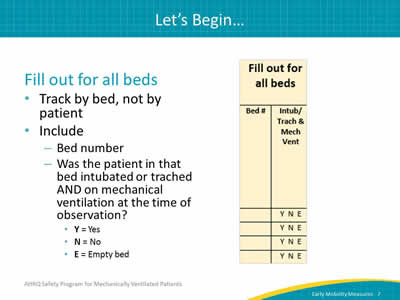
Image: Detail of bed number and intubation columns of data collection tool.
Fill out for all beds:
- Track by bed, not by patient.
- Include:
- Bed number.
- Was the patient in that bed intubated or trached AND on mechanical ventilation at the time of observation?
- Y = Yes.
- N = No.
- E = Empty bed.
Slide 8: Date of Intubation
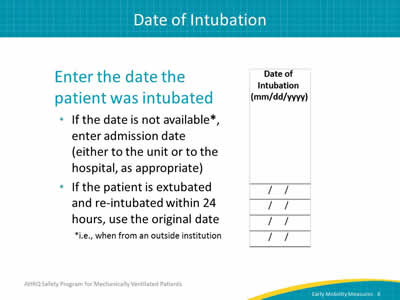
Image: Detail of date of intubation column from data collection tool.
Enter the date the patient was intubated:
- If the date is not available*, enter admission date (either to the unit or to the hospital, as appropriate).
- If the patient is extubated and re-intubated within 24 hours, use the original date.
*i.e., when from an outside institution.
Slide 9: Sedation Scale
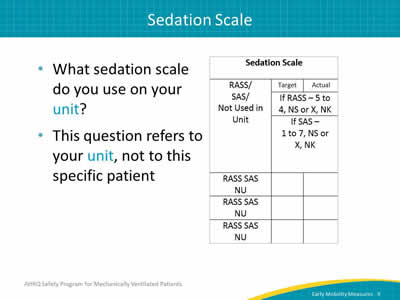
Image: Detail of the sedation scale columns.
- What sedation scale do you use on your unit?
- This question refers to your unit, not to this specific patient.
Slide 10: Sedation Scale
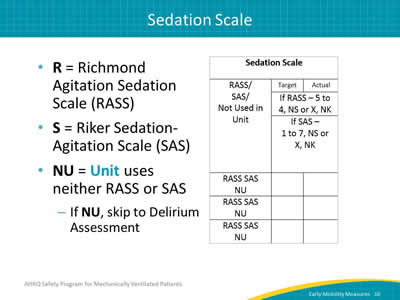
Image: Detail of the sedation scale columns.
- R = Richmond Agitation Sedation Scale (RASS).
- S = Riker Sedation-Agitation Scale (SAS).
- NU = Unit uses neither RASS or SAS:
- If NU, skip to Delirium Assessment.
Slide 11: Sedation Scale
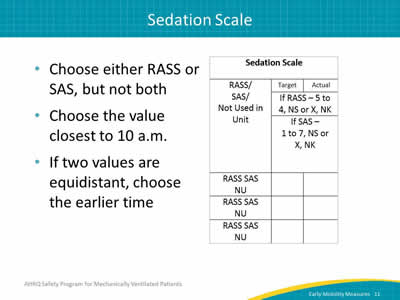
Image: Detail of the sedation scale columns.
- Choose either RASS or SAS, but not both.
- Choose the value closest to 10 a.m.
- If two values are equidistant, choose the earlier time.
Slide 12: Sedation Scale: Target RASS or SAS
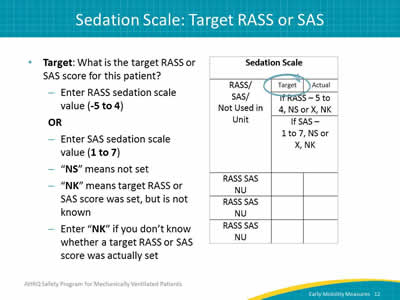
Image: Detail of the sedation scale columns, with "target" column head circled.
- Target: What is the target RASS or SAS score for this patient?
- Enter RASS sedation scale value (-5 to 4).
OR
- Enter SAS sedation scale value (1 to 7).
- "NS" means not set.
- "NK" means target RASS or SAS score was set, but is not known.
- Enter "NK" if you don’t know whether a target RASS or SAS score was actually set.
- Enter RASS sedation scale value (-5 to 4).
Slide 13: Sedation Scale: Actual RASS or SAS
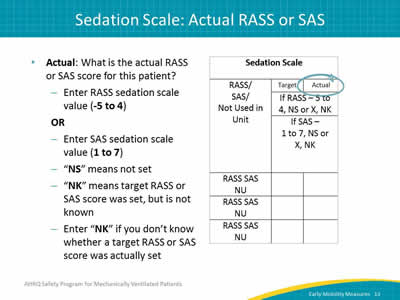
Image: Detail of the sedation scale columns with "actual" column head circled.
- Actual: What is the actual RASS or SAS score for this patient?
- Enter RASS sedation scale value (-5 to 4).
OR
- Enter SAS sedation scale value (1 to 7).
- "NS" means not set.
- "NK" means target RASS or SAS score was set, but is not known.
- Enter "NK" if you don’t know whether a target RASS or SAS score was actually set.
- Enter RASS sedation scale value (-5 to 4).
Slide 14: Delirium Assessment
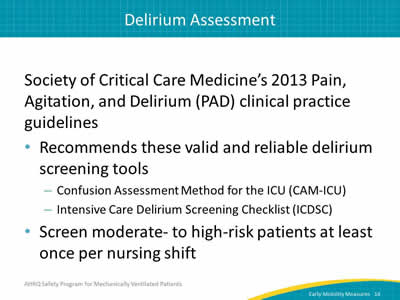
Society of Critical Care Medicine’s 2013 Pain, Agitation, and Delirium (PAD) clinical practice guidelines:
- Recommends these valid and reliable delirium screening tools:
- Confusion Assessment Method for the ICU (CAM-ICU).
- Intensive Care Delirium Screening Checklist (ICDSC).
- Screen moderate- to high-risk patients at least once per nursing shift.
Slide 15: Delirium Assessment
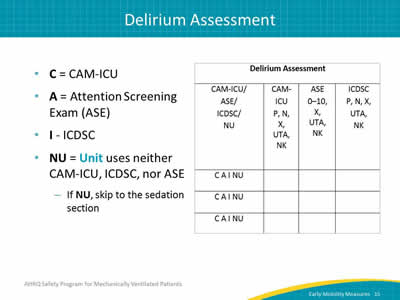
Image: Detail of delirium assessment columns of the data collection tool.
- C = CAM-ICU.
- A = Attention Screening Exam (ASE).
- I - ICDSC.
- NU = Unit uses neither CAM-ICU, ICDSC, nor ASE.
- If NU, skip to the sedation section.
Slide 16: Delirium Assessment
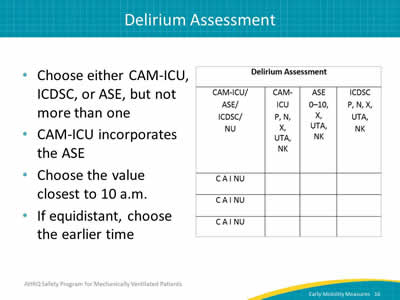
Image: Detail of delirium assessment columns of the data collection tool.
- Choose either CAM-ICU, ICDSC, or ASE, but not more than one.
- CAM-ICU incorporates the ASE.
- Choose the value closest to 10 a.m.
- If equidistant, choose the earlier time.
Slide 17: Delirium Assessment: CAM-ICU
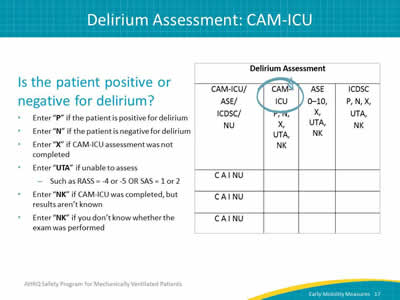
Image: Detail of delirium assessment columns of the data collection tool with "CAM-ICU" column head circled.
Is the patient positive or negative for delirium?
- Enter "P" if the patient is positive for delirium.
- Enter "N" if the patient is negative for delirium.
- Enter "X" if CAM-ICU assessment was not completed.
- Enter "UTA" if unable to assess:
- Such as RASS = -4 or -5 OR SAS = 1 or 2.
- Enter "NK" if CAM-ICU was completed, but results aren’t known.
- Enter "NK" if you don’t know whether the exam was performed.
Slide 18: Delirium Assessment: ICDSC
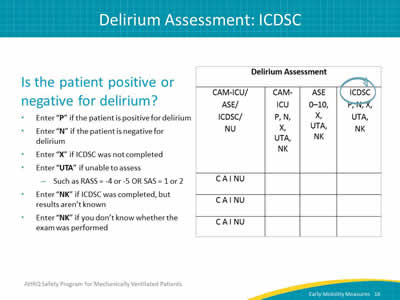
Image: Detail of delirium assessment columns of the data collection tool with "ICDSC" column head circled.
Is the patient positive or negative for delirium?
- Enter "P" if the patient is positive for delirium.
- Enter "N" if the patient is negative for delirium.
- Enter "X" if ICDSC was not completed.
- Enter "UTA" if unable to assess:
- Such as RASS = -4 or -5 OR SAS = 1 or 2.
- Enter "NK" if ICDSC was completed, but results aren’t known.
- Enter "NK" if you don’t know whether the exam was performed.
Slide 19: Delirium Assessment: Attention Screening Exam
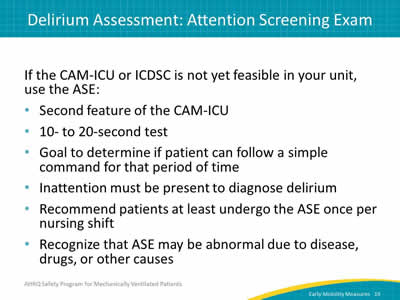
If the CAM-ICU or ICDSC is not yet feasible in your unit, use the ASE:
- Second feature of the CAM-ICU.
- 10- to 20-second test.
- Goal to determine if patient can follow a simple command for that period of time.
- Inattention must be present to diagnose delirium.
- Recommend patients at least undergo the ASE once per nursing shift.
- Recognize that ASE may be abnormal due to disease, drugs or other causes.
Slide 20: Attention Screening Exam
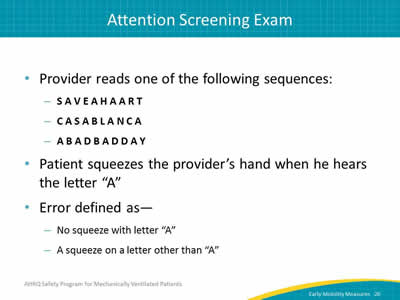
- Provider reads one of the following sequences:
- S A V E A H A A R T
- C A S A B L A N C A
- A B A D B A D D A Y
- Patient squeezes the provider’s hand when he hears the letter "A".
- Error defined as—
- No squeeze with letter "A".
- A squeeze on a letter other than "A".
Slide 21: Attention Screening Exam
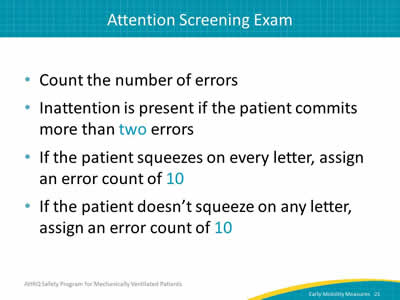
- Count the number of errors.
- Inattention is present if the patient commits more than two errors.
- If the patient squeezes on every letter, assign an error count of 10.
- If the patient doesn’t squeeze on any letter, assign an error count of 10.
Slide 22: Attention Screening Exam
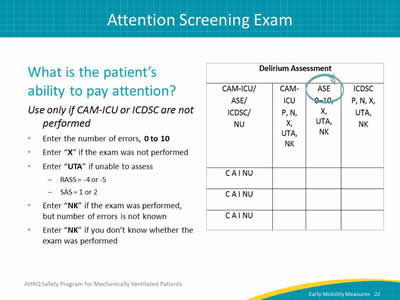
Image: Detail of delirium assessment columns of the data collection tool with "ASE" column head circled.
What is the patient’s ability to pay attention?
Use only if CAM-ICU or ICDSC are not performed
- Enter the number of errors, 0 to 10.
- Enter "X" if the exam was not performed.
- Enter "UTA" if unable to assess:
- RASS = -4 or -5.
- SAS = 1 or 2.
- Enter "NK" if the exam was performed, but number of errors is not known.
- Enter "NK" if you don’t know whether the exam was performed.
Slide 23: Data Collection: Early Mobility Measures
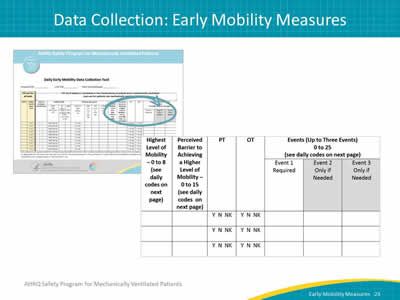
Images: The Daily Early Mobility Data Collection Tool. Detail of early mobility columns from the data collection tool.
Slide 24: Highest Level of Mobility
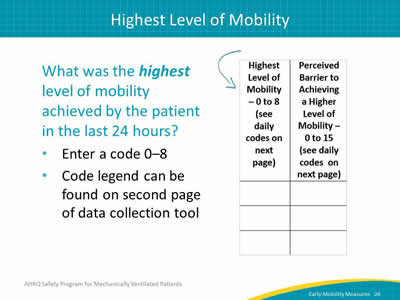
Image: Detail of early mobility columns from the data collection tool.
What was the highest level of mobility achieved by the patient in the last 24 hours?
- Enter a code 0–8.
- Code legend can be found on second page of data collection tool.
Slide 25: Highest Level of Mobility1
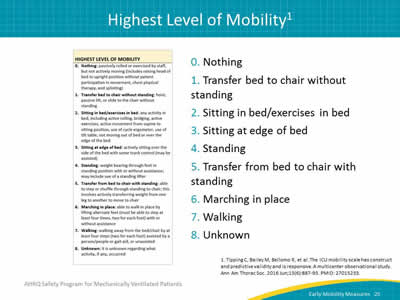
Image: The highest level of mobility code descriptions from the Early Mobility Data Collection Tool.
- Nothing.
- Transfer bed to chair without standing.
- Sitting in bed/exercises in bed.
- Sitting at edge of bed.
- Standing.
- Transfer from bed to chair with standing.
- Marching in place.
- Walking.
- Unknown.
1. Tipping C, Bailey M, Bellomo R, et al. The ICU mobility scale has construct and predictive validity and is responsive. A multicenter observational study. Ann Am Thorac Soc 2016 Jun;13(6):887-93. PMID: 27015233.
Slide 26: Perceived Barrier to Achieving Higher Mobility
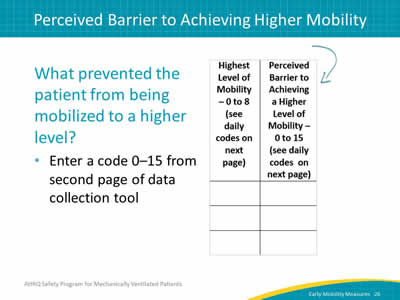
Image: Detail of early mobility columns from the data collection tool.
What prevented the patient from being mobilized to a higher level?
- Enter a code 0–15 from second page of data collection tool.
Slide 27: Perceived Barrier Code Examples
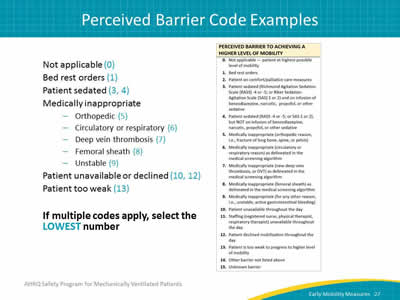
Image: Codes for perceived barriers to achieving a higher level of mobility.
- Not applicable (0).
- Bed rest orders (1).
- Patient sedated (3, 4).
- Medically inappropriate:
- Orthopedic (5).
- Circulatory or respiratory (6).
- Deep vein thrombosis (7).
- Femoral sheath (8).
- Unstable (9).
- Patient unavailable or declined (10, 12).
- Patient too weak (13).
If multiple codes apply, select the LOWEST number.
Slide 28: Physical and Occupational Therapy
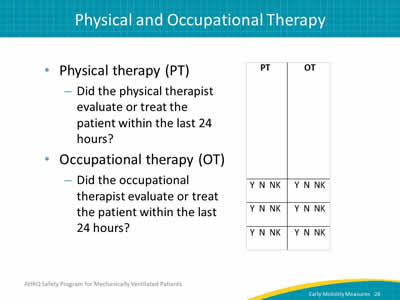
Image: Detail of PT and OT columns from data collection tool.
- Physical therapy (PT):
- Did the physical therapist evaluate or treat the patient within the last 24 hours?
- Occupational therapy (OT):
- Did the occupational therapist evaluate or treat the patient within the last 24 hours?
Slide 29: Events
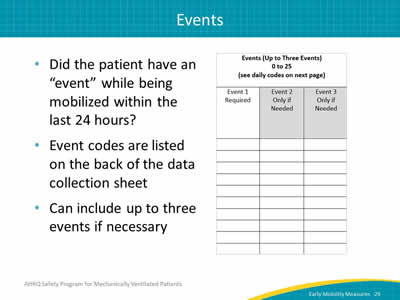
Image: Detail of the event reporting column from the data collection tool.
- Did the patient have an "event" while being mobilized within the last 24 hours?
- Event codes are listed on the back of the data collection sheet.
- Can include up to three events if necessary.
Slide 30: Event Codes
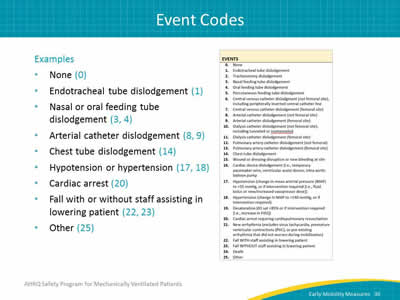
Image: Event codes for recording events that occur during mobilization.
Examples:
- None (0).
- Endotracheal tube dislodgement (1).
- Nasal or oral feeding tube dislodgement (3, 4).
- Arterial catheter dislodgement (8, 9).
- Chest tube dislodgement (14).
- Hypotension or hypertension (17, 18).
- Cardiac arrest (20).
- Fall with or without staff assisting in lowering patient (22, 23).
- Other (25).
Slide 31: Data Measures Guide
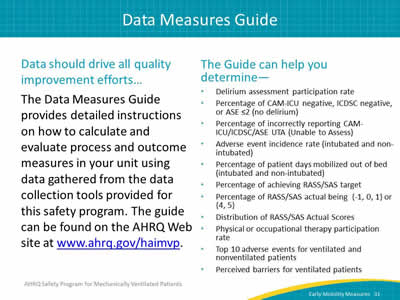
Data should drive all quality improvement efforts...
The Data Measures Guide provides detailed instructions on how to calculate and evaluate process and outcome measures in your unit using data gathered from the data collection tools provided for this safety program. The guide can be found on the AHRQ Web site at www.ahrq.gov/haimvp.
The Guide can help you determine—
- Delirium assessment participation rate.
- Percentage of CAM-ICU negative, ICDSC negative, or ASE ≤2 (no delirium).
- Percentage of incorrectly reporting CAM-ICU/ICDSC/ASE UTA (Unable to Assess).
- Adverse event incidence rate (intubated and non-intubated).
- Percentage of patient days mobilized out of bed (intubated and non-intubated).
- Percentage of achieving RASS/SAS target.
- Percentage of RASS/SAS actual being {-1, 0, 1} or {4, 5}.
- Distribution of RASS/SAS Actual Scores.
- Physical or occupational therapy participation rate.
- Top 10 adverse events for ventilated and nonventilated patients.
- Perceived barriers for ventilated patients.
Slide 32: Questions?
Image: A series of multi-colored hanging tags with question marks on them.
Slide 33: References
1. Tipping C, Bailey M, Bellomo R, et al. The ICU mobility scale has construct and predictive validity and is responsive. A multicenter observational study. Ann Am Thorac Soc 2016 Jun;13(6):887-93. PMID: 27015233.



