Optimize Briefings and Debriefings: Slide Presentation
AHRQ Safety Program for Surgery
Slide 1: AHRQ Safety Program for Surgery—Implementation
Optimize Briefings and Debriefings
Slide 2: Learning Objectives
- Describe characteristics of effective briefings and debriefings.
- Present the evidence base for briefings and debriefings to your surgeons and surgical staff during a staff meeting.
- Prioritize and investigate defects identified by the team during operating room debriefings.
Slide 3: Safety Program for Surgery Approach
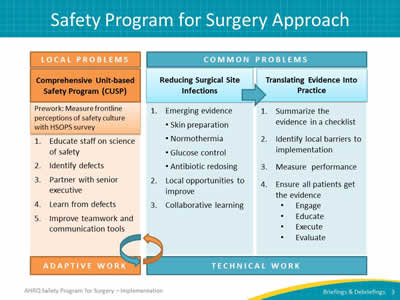
Image: Three columns presenting CUSP, Reducing SSIs, and TRIP:
ADAPTIVE WORK:
Comprehensive Unit-based Safety Program (CUSP):
Prework: Measure frontline perceptions of safety culture with HSOPS survey.
- Educate staff on science of safety.
- Identify defects.
- Partner with a senior executive.
- Learn from defects.
- Improve teamwork and communication.
TECHNICAL WORK:
Reducing Surgical Site Infections:
- Emerging evidence [Skin preparation, Normothermia, Glucose control, Antibiotic redosing].
- Local opportunities to improve.
- Collaborative learning.
Translating Research into Practice (TRiP):
- Summarize the evidence in a checklist.
- Identify local barriers to implementation.
- Measure performance.
- Ensure all patients get the evidence (Engage, Educate, Execute, Evaluate).
Slide 4: Comprehensive Unit-based Safety Program1
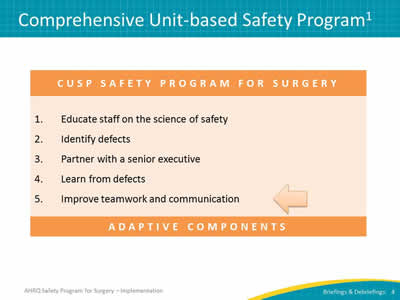
Image: Box with heading CUSP Safety Program for Surgery:
- Educate staff on the science of safety.
- Identify defects.
- Partner with a Senior Executive.
- Learn from defects.
- Improve teamwork and communication.
Adaptive components
An arrow points to Step 5: Improve teamwork and communication.
Slide 5: AHRQ Safety Program for Surgery—Implementation
Basics of Briefing and Debriefing
Slide 6: Overview of Critical Team Interactions
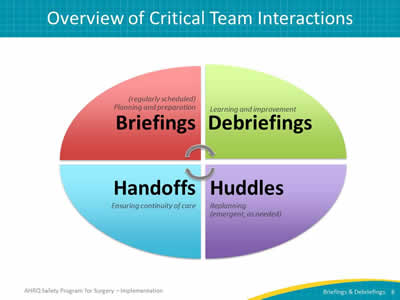
Image: Oval broken into four quadrants with central arrows indicating cyclical proces. Quadrants are captioned:
- Briefings: Planning and preparation (regularly scheduled).
- Debriefings: Learning and improvement.
- Huddles: Replanning (emergent, as needed).
- Handoffs: Ensuring continuity of care.
Slide 7: What Is a Briefing?

A briefing is a discussion between two or more people, often a team, using succinct information pertinent to an event.
Image: Photograph of medical providers gathered around a laptop.
Slide 8: Purpose of a Briefing
- Maps out the plan of care.
- Identifies roles and responsibilities for each team member.
- Heightens awareness of the situation.
- Allows the team to plan for the unexpected.
- Anticipates team members’ needs and expectations.
Slide 9: Effective Briefings
- Set the tone for the day:
- Chaotic and harried
OR - Organized and efficient.
- Chaotic and harried
- Encourage participation and ownership by all team members:
- Organize based on procedure.
- Establish competencies.
- Anticipate events and plan for the unexpected:
- Equipment, medications, consultations.
- Intensive care unit bed.
Slide 10: Briefing Checklist
Topic:
- Who is on core team?
- All members understand and agree upon goals?
- Roles and responsibilities understood?
- Plan of care?
- Staff availability?
- Workload?
- Available resources?
Image: Photograph of medical staff examining a list posted on a wall. Sample checklist has seven items with a check box next to each one.
Slide 11: Team Debrief
What can we do better next time?
- Brief, informal information exchange and feedback sessions.
- Occur after an event or shift.
- Stress learning and improvement.
- Designed to improve teamwork skills.
- Designed to improve outcomes:
- Accurate reconstruction of key events.
- Analysis of why the event occurred.
- Focus on what should be done differently next time.
Slide 12: Root Causes of Sentinel Events in 20132
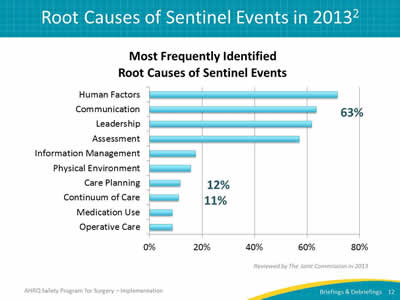
Image: Bar chart of the most frequently identified root causes of sentinel events as reviewed by the Joint Commission in 2013:
- Human Factors - 70%.
- Communication - 63%.
- Leadership - 61%.
- Assessment - 58%.
- Information Management - 18%.
- Physical Environment - 17%.
- Care Planning - 12%.
- Continuum of Care - 11%.
- Medication Use - 9%.
- Operative Care - 8%.
Communication, Care Planning, and Continuum of Care categories are stressed with values placed next to each bar.
Slide 13: Evidence Supports Briefings
- Reduce communication breakdowns and operating room delays.3
- Reduce procedure and miscommunication-related disruptions and nursing time spent in core.4
- Improve communication and teamwork, as feasible given current workload.5
- Reduce rate of complications, surgical site infections, and mortality.6
Slide 14: Evidence Supports Briefings
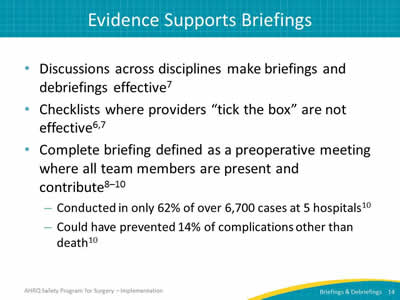
- Discussions across disciplines make briefings and debriefings effective.7
- Checklists where providers “tick the box” are not effective.6,7
- Complete briefing defined as a preoperative meeting where all team members are present and contribute.8–10
Slide 15: Evidence Supports Briefings
- Create shared mental model among team members.11
- Reduce task-related conflict in multi-disciplinary teams.12
- Clarify roles and responsibilities.8,9,12
- Anticipate changes and plan for emergent patient needs.11
Slide 16: Briefing and Debrief Checklist
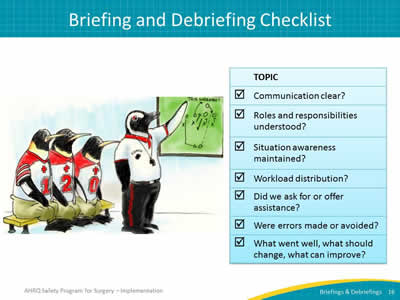
Topic:
- Communication clear?
- Roles and responsibilities understood?
- Situation awareness maintained?
- Workload distribution?
- Did we ask for or offer assistance?
- Were errors made or avoided?
- What went well, what should change, what can improve?
Image: Cartoon of penguin dressed in coach shirt with whistle, pointing to game plan on chalkboard while three penguin players watch from a bench.
Slide 17: Why Briefings and Debriefings?
Teams perform better when they…
- Have a high quality plan.
- Share that plan.
- Learn and improve over time.
Briefings and debriefings can help, but they do not guarantee good planning.
Checking the box ≠ Mindful engagement
Slide 18: Why Briefings and Debriefings?
- Surgical safety checklists associated with significant reductions in mortality.6
- Later, 50% of reductions associated with preexisting safety culture rather than checklist alone.13
- Surgical units with strong safety culture yielded significant benefit with briefing checklist.
- Units with weaker safety culture saw minimal improvement.
- Staff that value teammates and tools are mindful of process and achieve results.
Slide 19: How Do You Create a Mindful Process?

- Coaching, role modeling, and feedback:
- Show that the organization values this process.
- Build effective communication behaviors.
- Briefing and debriefing process closes the loop with outcomes:
- Identifies defects and encourages correction.
- Validates the process.
Slide 20: AHRQ Safety Program for Surgery—Implementation
Operating Room Briefings and Debriefings
Slide 21: Timeout: The Universal Protocol
- Right patient.
- Right procedure.
- Right site.
Image: Check mark in a box.
Slide 22: Briefings: Expanding the Timeout
- Introduce all team members by first and last names.
- Write names and roles on white board.
- Facilitate timeouts.
- Share goal of the operation (surgeon).
- Identify all issues or concerns (entire team).
Slide 23: What Is Most Likely To Go Wrong?
Safety concerns
- Identify critical steps of the procedure?
- Is required equipment available?
- Is someone trained on the equipment available?
- Is instrumentation available?
- Need implants?
- Has attending physician reviewed latest test results from lab and radiology?
Slide 24: What Is Most Likely To Go Wrong?
Operating room best practices
- Antibiotic type, dosage, and redosing.
- Beta blockers.
- Glucose control.
- Positioning.
- Blood loss and blood availability.
- Deep vein thrombosis prophylaxis.
- Normothermia warmers usage and availability.
Slide 25: What Is Most Likely To Go Wrong?
Other concerns
- Special precautions.
- Bed availability.
- Intensive care bed requirement.
- Staffing and shift changes.
- Time allotted for procedure.
Slide 26: Briefings: Best Practices
- All team members should be present and participating, including the surgical attending.
- May include the patient in the discussion.
- Assign a point person to own the process.
- Initiate the tool or checklist.
- Write names of providers on white board.
- Modify checklist to local context.
Slide 27: Timeout: Prior to Incision
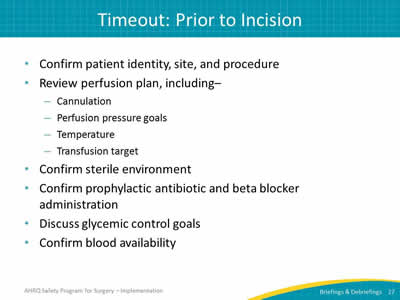
- Confirm patient identity, site, and procedure.
- Review perfusion plan, including–
- Cannulation.
- Perfusion pressure goals.
- Temperature.
- Transfusion target.
- Confirm sterile environment.
- Confirm prophylactic antibiotic and beta blocker administration.
- Discuss glycemic control goals.
- Confirm blood availability.
Slide 28: Timeout: Best Practices
- All team members present.
- Use a checklist to serve as reminder.
- Encourage 100% participation.
Slide 29: Briefings in the Operating Room
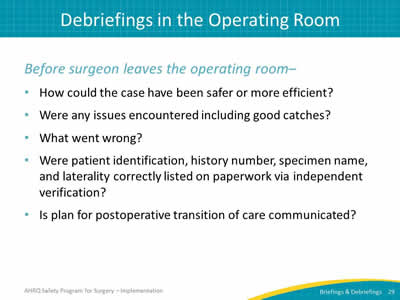
Before surgeon leaves the operating room–
- How could the case have been safer or more efficient?
- Were any issues encountered including good catches?
- What went wrong?
- Were patient identification, history number, specimen name, and laterality correctly listed on paperwork via independent verification?
- Is plan for postoperative transition of care communicated?
Slide 30: Debriefings: Best Practices
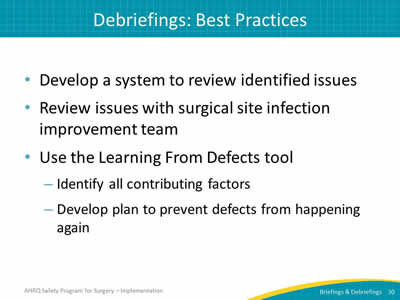
- Develop a system to review identified issues.
- Review issues with surgical site infection improvement team.
- Use the Learning From Defects tool:
- Identify all contributing factors.
- Develop plan to prevent defects from happening again.
Slide 31: Real-Time Identification of Defects
- Customize form based on needs in your surgical unit.
- Initiate candid discussions with surgeons about effective strategies for briefing and debriefing.
- Provide protected time for nurse to address defects and communicate solutions.
- Maintain logbook of defects.
Slide 32: World Health Organization Checklist
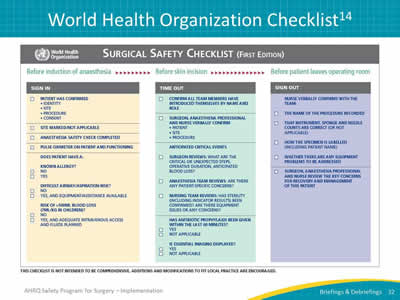
Image: Three-phase checklist for the surgical setting. It covers Sign In (before induction of anesthesia), Time Out (before skin incision), and Sign Out (before patient leaves operating room).
Slide 33: Colorectal Surgical Safety Checklist
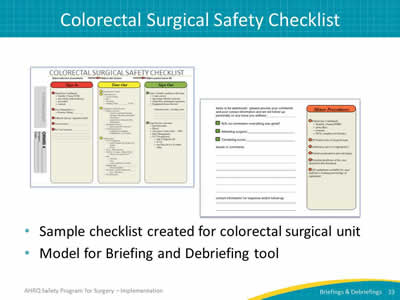
- Sample checklist created for colorectal surgical unit.
- Model for Briefing and Debriefing tool.
Image: Johns Hopkins Medicine local adaptation of a surgical safety checklist.
Slide 34: Debriefing Defect Logbook
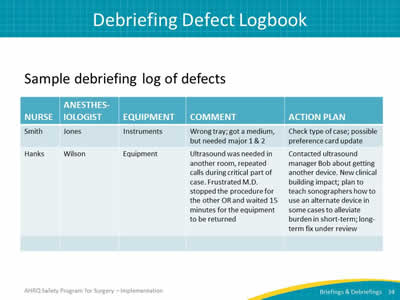
Sample debriefing log of defects.
Image: Two examples shared with the following column headings: Nurse, Anesthesiologist, Equipment, Comment, and Action Plan:
First example of an instrument defect: Wrong tray; got a medium, but needed major 1 & 2. Action: Check type of case; possible preference card update.
Second example of an equipment defect: Ultrasound was needed in another room, repeated calls during critical part of case. Frustrated MD stopped the procedure for the other OR and waited 15 minutes for the equipment to be returned. Action: Contacted ultrasound manager Bob about getting another device. New clinical building impact; plan to teach sonographers how to use an alternate device in some cases to alleviate burden in short-term; long-term fix under review.
Slide 35: Example of Defects Addressed: Instruments
Problem
Conflict with colorectal surgical instrument set.
Solution
Increased fleet from two to four.
Reorganized set contents so it is only pulled for cases when needed.
Impact
Instruments available when needed.
Image: Photograph of colorectal surgery set of tools.
Slide 36: Case Study: Laparoscopic Surgery Trays
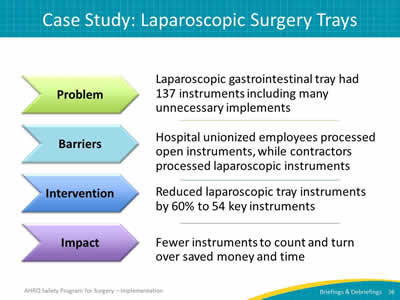
Problem
Laparoscopic gastrointestinal tray had 137 instruments including many unnecessary implements.
Barriers
Hospital unionized employees processed open instruments, while contractors processed laparoscopic instruments.
Intervention
Reduced laparoscopic tray instruments by 60% to 54 key instruments.
Impact
Fewer instruments to count and turn over saved money and time.
Image: Problem, barriers, intervention, and impact are located within arrows pointing to descriptions of each.
Slide 37: Case Study: Laparoscopic Surgery Trays

Images: "Before" photograph of laparoscopic GI Surgery Tray with 137 instruments and "After" photograph of laparoscopic GI Surgery Tray with 54 instruments.
Slide 38: Examples of Defects Addressed
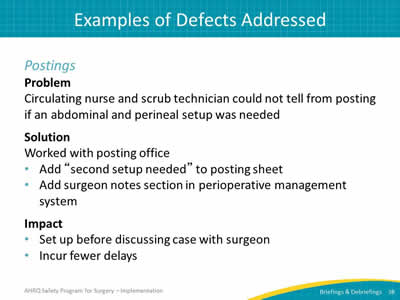
Postings
Problem
Circulating nurse and scrub technician could not tell from posting if an abdominal and perineal setup was needed.
Solution
Worked with posting office:
- Add “second setup needed” to posting sheet.
- Add surgeon notes section in perioperative management system.
Impact
- Set up before discussing case with surgeon.
- Incur fewer delays.
Slide 39: Examples of Defects Addressed
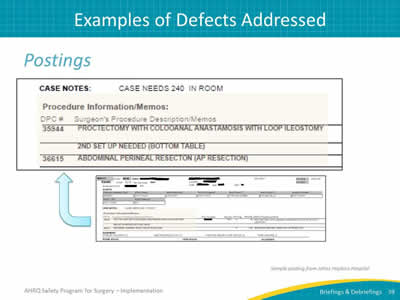
Postings
Image: Sample of a Hopkins posting. Highlights second setup requirement in the Procedure section.
Slide 40: Examples of Defects Addressed
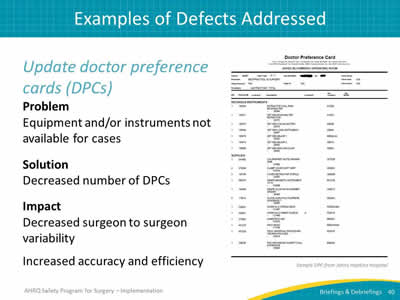
Update doctor preference cards (DPCs)
Problem
Equipment and/or instruments not available for cases.
Solution
Decreased number of DPCs.
Impact
Decreased surgeon to surgeon variability.
Increased accuracy and efficiency.
Image: Sample doctor preference card.
Slide 41: What Can We Catch?
- Wrong consents.
- Wrong patients.
- Incorrect equipment, implants, or instruments.
- Comorbidities that have a surgical impact.
- Incorrect specimen labels.
- Documentation issues.
- Unclear perioperative care instructions.
Slide 42: What Can We Accomplish?
- Create a shared mental model.
- Reduce missing equipment.
- Minimize team disruptions and reduce distractions.
- Contribute to more than 70% of sentinel events.5,6
- Reduce hazards.
Slide 43: Adapting to Local Context
- Make interventions relevant and meaningful to staff:
- Ineffective and inefficient to use the same checklist for all procedure types.
- Adapt tools to needs of your clinical area.
- Allow frontline staff to drive improvement efforts:
- Perioperative Staff Safety Assessment (2 questions).
- Surgical audits tools.
- Fixing local defects is a powerful (and visible) strategy to gain staff buy in and encourage participation.
Slide 44: Lessons Learned

Briefings and debriefings–
- Reshape safety culture with time and commitment.
- Foster safety culture growth.
- Practice and expect open communication.
- Flatten the hierarchy.
- Focus on the patient.
- Adapt to local context so are meaningful to staff.
- Identify defects proactively as they occur.
Slide 45: Next Steps
- Evaluate how tools fit into your local context.
- Get input from all stakeholders.
- Modify the tool to fit your needs.
- Tailor to specific surgical procedure areas.
- Create followup mechanism to address defects identified during briefings.
- Identify a surgeon champion who will implement briefings and debriefings for surgical cases.
- Pilot, revise, and implement briefings.
Slide 46: References
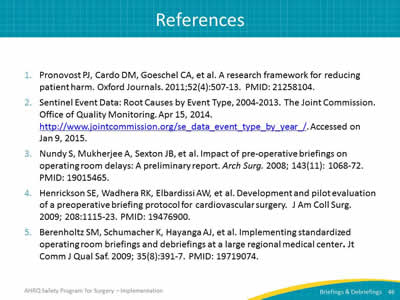
- Pronovost PJ, Cardo DM, Goeschel CA, et al. A research framework for reducing patient harm. Oxford Journals 2011;52(4):507-13. PMID: 21258104.
- Sentinel Event Data: Root Causes by Event Type, 2004-2013. The Joint Commission. Office of Quality Monitoring. Apr 15, 2014. http://www.jointcommission.org/se_data_event_type_by_year_/. Accessed on Jan 9, 2015.
- Nundy S, Mukherjee A, Sexton JB, et al. Impact of pre-operative briefings on operating room delays: A preliminary report. Arch Surg 2008; 143(11): 1068-72. PMID: 19015465.
- Henrickson SE, Wadhera RK, Elbardissi AW, et al. Development and pilot evaluation of a preoperative briefing protocol for cardiovascular surgery. J Am Coll Surg 2009; 208:1115-23. PMID: 19476900.
- Berenholtz SM, Schumacher K, Hayanga AJ, et al. Implementing standardized operating room briefings and debriefings at a large regional medical center. Jt Comm J Qual Saf 2009; 35(8):391-7. PMID: 19719074.
Slide 47: References
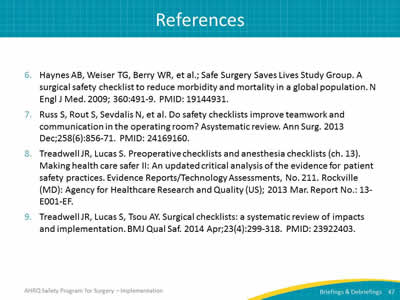
- Haynes AB, Weiser TG, Berry WR, et al.; Safe Surgery Saves Lives Study Group. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med 2009; 360:491-9. PMID: 19144931.
- Russ S, Rout S, Sevdalis N, et al. Do safety checklists improve teamwork and communication in the operating room? Asystematic review. Ann Surg 2013 Dec;258(6):856-71. PMID: 24169160.
- Treadwell JR, Lucas S. Preoperative checklists and anesthesia checklists (ch. 13). Making health care safer II: An updated critical analysis of the evidence for patient safety practices. Evidence Reports/Technology Assessments, No. 211. Rockville (MD): Agency for Healthcare Research and Quality (US); 2013 Mar. Report No.: 13-E001-EF.
- Treadwell JR, Lucas S, Tsou AY. Surgical checklists: a systematic review of impacts and implementation. BMJ Qual Saf 2014 Apr;23(4):299-318. PMID: 23922403.
Slide 48: References
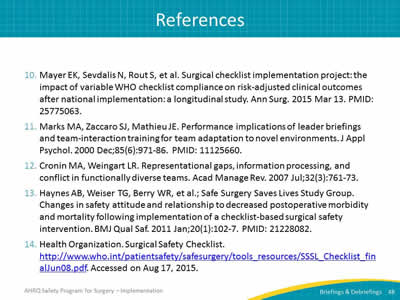
- Mayer EK, Sevdalis N, Rout S, et al. Surgical checklist implementation project: the impact of variable WHO checklist compliance on risk-adjusted clinical outcomes after national implementation: a longitudinal study. Ann Surg 2015 Mar 13. PMID: 25775063.
- Marks MA, Zaccaro SJ, Mathieu JE. Performance implications of leader briefings and team-interaction training for team adaptation to novel environments. J Appl Psychol 2000 Dec;85(6):971-86. PMID: 11125660.
- Cronin MA, Weingart LR. Representational gaps, information processing, and conflict in functionally diverse teams. Acad Manage Rev 2007 Jul;32(3):761-73.
- Haynes AB, Weiser TG, Berry WR, et al.; Safe Surgery Saves Lives Study Group. Changes in safety attitude and relationship to decreased postoperative morbidity and mortality following implementation of a checklist-based surgical safety intervention. BMJ Qual Saf 2011 Jan;20(1):102-7. PMID: 21228082.
- Health Organization. Surgical Safety Checklist. http://www.who.int/patientsafety/safesurgery/tools_resources/SSSL_Checklist_finalJun08.pdf. Accessed on Aug 17, 2015.
Slide 49: AHRQ Safety Program for Surgery—Implementation
Hospital Team Experience: Briefings and Debriefings
Slide 50: Briefings and Debriefings
- Preoperative Verification.
- Briefing or Timeout.
- Debriefing.
Images: Photograph of hospital room setting; medical staff in scrubs performing preoperative verification. Photograph of medical staff in scrubs performing time out briefing. Photograph of operating room team debriefing after case.
Slide 51: Barriers to Debriefing
- Team needed approval from the administration.
- Staff hesitant to incorporate another form.
- Team questioned if staff would comply with new form and process.
Slide 52: Success with Debriefing
- Championed by our surgical quality improvement team.
- Provides process to document concerns and issues.
- Reviews and shares followup opportunities.
- Improves morale as staff and surgeons see issues addressed.
- Reduces number of less-urgent issues escalated to management.
Slide 53: Tips for Successful Debriefing
- Make process easy for staff to use:
- Place form in chart for every case.
- Provide a system to review issues:
- Review with operating room management, staff, and surgeons.
- Assign followup actions.
- Be transparent:
- Keep a log of all defects.
- Prioritize which (and when) defects will be addressed.
- List steps taken to address defects.
- Share the resolution of defects.
Image: Photographs of operating room team debriefing after case.
Slide 54: Intraoperative Debriefing
- Perform at case completion, usually after the first count and before surgeon leaves the operating room.
- Cover what went well, good catches, and room for improvement.
- Ask if instrument, sponge, and needle counts are correct.
- Record name of procedure and wound classification.
- If applicable, specify how specimen labeled or provide special instructions.
- Address equipment issues.
- Plan postoperative beta blockers, if applicable.
- Communicate key concerns for recovery and management of the patient.
Slide 55: Logging Debriefing Comments
- Record comments in a spreadsheet file.
- Use column headings applicable to local needs.
- Filter comments by subject, specialty, or procedure.
- Standing agenda item in the vascular meeting to review all vascular debriefing comments.
- Equipment issues reviewed in appropriate areas as well.
Image: Photograph of clerical staff member recording the debriefing comments in a spreadsheet.
Slide 56: Montly Debriefing Report
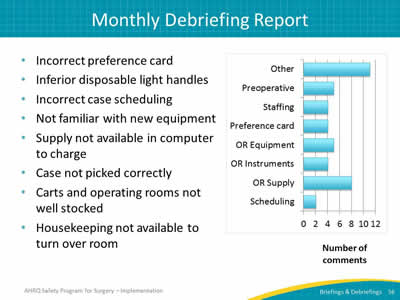
- Incorrect preference card.
- Inferior disposable light handles.
- Incorrect case scheduling.
- Not familiar with new equipment.
- Supply not available in computer to charge.
- Case not picked correctly.
- Carts and operating rooms not well stocked.
- Housekeeping not available to turn over room.
Image: Bar chart reporting number of comments by category:
- Other - 11.
- Preoperative - 5.
- Staffing - 4.
- Preference card - 4.
- OR Equipment - 5.
- OR Instruments - 4.
- OR Supply - 8.
- Scheduling - 2.



