The Science of Improving Patient Safety and Identifying Defects: Slide Presentation
AHRQ Safety Program for Surgery
Slide 1: AHRQ Safety Program for Surgery—Onboarding
The Science of Improving Patient Safety and Identifying Defects
Slide 2: Learning Objectives
After this session, you will be able to—
- Educate your team and executive partners on the Science of Safety.
- Identify defects within your operating room by administering the Perioperative Safety Staff Assessment (PSSA).
- Distribute and share PSSA results with your team.
- Locate resources on the program Web site to help complete the above tasks.
- Apply Science of Safety principles to your work.
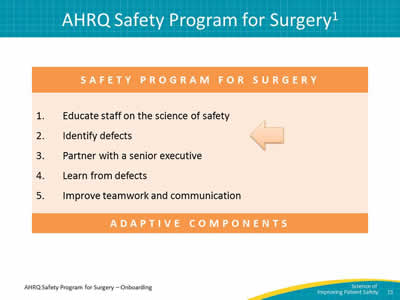
Slide 3: AHRQ Safety Program for Surgery1
Safety Program for Surgery
- Educate staff on the science of safety.
- Identify defects.
- Partner with a senior executive.
- Learn from defects.
- Improve teamwork and communication.
Adaptive Components
Image: Arrow indicates Step 1: Educate staff on the science of safety.
Slide 4: Advances in Medicine: Lingering Contradictions
Advances in medicine have led to positive outcomes:
- Most childhood cancers are curable.
- AIDS is now a chronic disease.
- Life expectancy has increased 10 years since the 1950s.
However, sponges are still found inside patients’ bodies after operations.
Slide 5: Why is This Work Important?2
- 1 in 25 people will undergo surgery worldwide.
- 7 million complications follow inpatient surgeries.
- Complications impact 25% of inpatient surgeries.
- 1 million deaths follow surgery.
- Between 0.5 and 5% of surgical patients do not survive.
- Surgery is linked to 50% of all hospital adverse events.
- Most hospital adverse events are AVOIDABLE.
Slide 6: How Do These Errors Happen?
- Medicine is still treated as an art, not a science.
- People are fallible.
- Every system is perfectly designed to achieve its results.
- Need to view the delivery of health care as a science.
- Reengineer systems to catch mistakes.
Slide 7: Educate Staff on the Science of Safety3,4
Three primary concepts of science of safety:
- Understand that the system determines performance, and safety is the property of the system.
- Use strategies to improve system performance.
- Recognize that teams with diverse and independent input make wise decisions.
Slide 8: Who Is Making Mistakes?
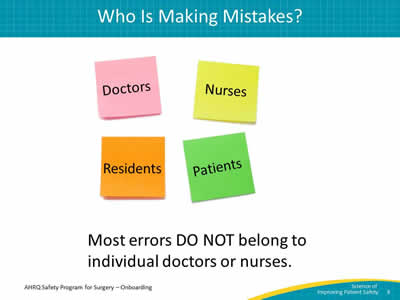
Most errors DO NOT belong to individual doctors or nurses.
Images: Four post-it notes labeled Doctors, Nurses, Residents, and Patients.
Slide 9: System Factors Impact Safety5
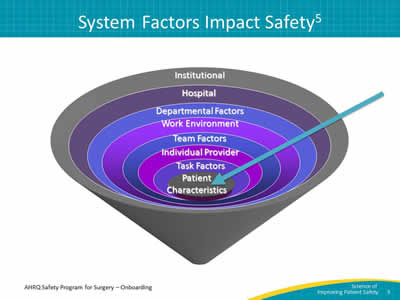
Image: Funnel depicting the factors that come together to impact patient safety. From the top of the funnel to the bottom, these factors include: institutional, hospital, departmental factors, the work environment, team factors, individual provider, task factors, and patient characteristics. An arrow points through the system factors into the funnel.
Image based on the work of Vincent C, Taylor-Adams S, Stanhope N., BMJ. Framework for analysing risk and safety in clinical medicine.1998; 316(7138):1154-7. PMID: 9552960. Developed at the Johns Hopkins Armstrong Institute for Patient Safety and Quality.
Slide 10: Safety Is a Property of the System

This video illustrates using system lenses in action.
Science of Safety videos are available at www.ahrq.gov/professionals/education/curriculum-tools/cusptoolkit/modules/understand/index.html
Slide 11: Educate Staff on the Science of Safety3,4
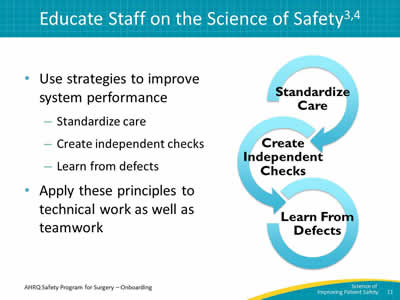
- Use strategies to improve system performance:
- Standardize care.
- Create independent checks.
- Learn from defects.
- Apply these principles to technical work as well as teamwork.
Image: Three interlocking circles labeled with the principles of the science of safety.
- Standardize care.
- Create independent checks.
- Learn from defects.
Slide 12: Standardize When You Can
In this video, we learn more from Dr. Peter Pronovost about the value of standardization.
Science of Safety videos are available at www.ahrq.gov/professionals/education/curriculum-tools/cusptoolkit/modules/understand/index.html
Slide 13: Create Independent Checks

This video illustrates the power of creating independent checks for key processes.
Science of Safety videos are available at www.ahrq.gov/professionals/education/curriculum-tools/cusptoolkit/modules/understand/index.html
Slide 14: Educate Staff on the Science of Safety3,4

- Recognize that teams with diverse and independent input make wise decisions.
- Encourage team members from different disciplines to contribute their expertise.
Slide 15: AHRQ Safety Program for Surgery1
Safety Program for Surgery
- Educate staff on the science of safety.
- Identify defects.
- Partner with a senior executive.
- Learn from defects.
- Improve teamwork and communication.
Adaptive Components
Image: Arrow indicates Step 2: Identify defects.
Slide 16: Communication Breakdowns6
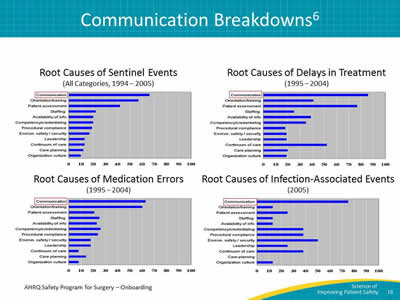
Images: Four bar graphs showing root causes of adverse events including sentinel events, medication errors, delays in treatment, and infection-associated events from 1995 to 2004. The Y-axis of each graph shows types of events. The X-axis shows percent in 10-percent intervals. In each graph, communication is the most common root cause of each event.
Graphic created by Joint Commission on Accreditation of Healthcare Organizations.
Slide 17: Basic Process of Communication7
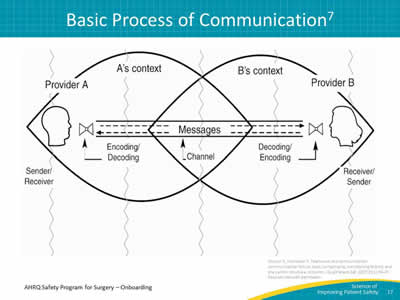
Image: An illustration of communication processes for two different providers (Provider A, shown at the left of the image as a male profile, and Provider B, shown at the right of the image as a female profile). The image shows that messages (illustrated by dashed arrows from one provider to the other) are encoded and decoded based on each provider's unique context. There's only partial overlap when it comes to shared perceptions of message content.
Source: Dayton E, Henrikson K. Teamwork and communication: communication failure: basic components, contributing factors, and the call for structure. Jt Comm J Qual Patient Saf 2007;31(1):34-47. Reproduced with permission.
Slide 18: What Is a Defect?

Anything that happens that you do not want to happen again.
Slide 19: Defect Examples That Affect Patient Safety
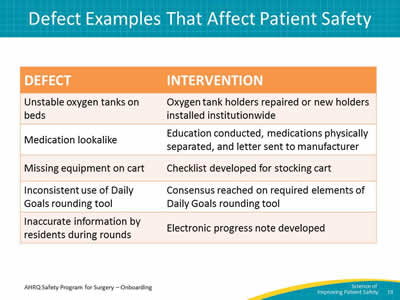
Image: The table presents a series of defects and their interventions:
- Unstable oxygen tanks on beds resulted in an intervention where oxygen tank holders were repaired or new holders were installed across the institution.
- A medication look-alike incident led to an intervention where education was conducted, medications were physically separated and a letter was sent to the manufacturer.
- Missing equipment on a cart resulted in the development of a checklist for stocking the cart.
- The inconsistent use of Daily Goals during rounding resulted in a group consensus on required elements of the Daily Goals rounding tools.
- Inaccurate information by residents during rounds resulted in the development of an electronic progress note.
Slide 20: How Can Your Team Identify Defects?
- Event reporting systems, liability claims, sentinel events, morbidity and mortality conferences.
- Perioperative Staff Safety Assessment (PSSA):
- Four-question survey.
- Completed by ALL staff members in the clinical area, not just medical staff.
Slide 21: PSSA Taps Wisdom of Frontline Providers
- Frontline providers–
- Understand the patient safety risks in their clinical areas.
- Have insight into potential solutions to these problems.
- Tap into this knowledge and use it to guide safety improvement efforts.
Slide 22: What Is the PSSA?
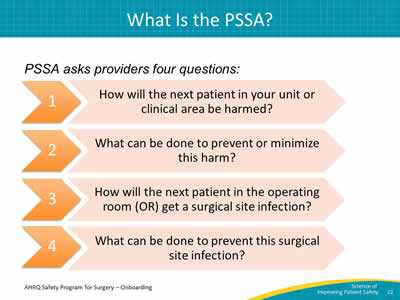
PSSA asks providers four questions:
- How will the next patient in your unit or clinical area be harmed?
- What can be done to prevent or minimize this harm?
- How will the next patient in the operating room get a surgical site infection?
- What can be done to prevent this surgical site infection?
Images: The questions are presented inside orange arrows for visual interest.
Slide 23: Who Administers the PSSA and When?
- Who: safety project lead or a designee.
- Recommendation: Administer PSSA to ALL staff following training on the Science of Safety – providers will have lenses to see system problems.
- To encourage staff to report safety concerns, establish a collection box in an accessible location where completed forms can be dropped off.
- Complete the PSSA at least every 6 months.
Slide 24: What’s Next? Interpreting PSSA Results
Prioritize identified defects using the following criteria:
- Likelihood of the defect harming the patient.
- Severity of harm the defect causes.
- Frequency of the defect occurrence.
- Likelihood of preventing defect in daily work.
Slide 25: How Will the Next Patient Be Harmed?
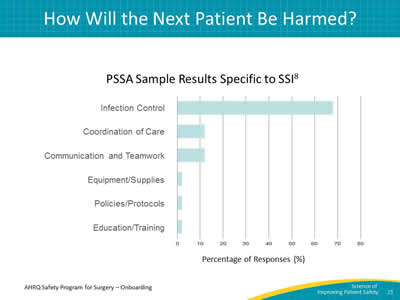
Image: Bar chart shows percentage of 95 SSI-specific responses8 from 36 staff members when asked, "How will the next patient be harmed?" Over 60 percent of staff members identified infection control as an important issue.
Reference: Wick EC, Hobson DB, Bennett JL, et al. Implementation of a surgical comprehensive unit-based safety program to reduce surgical site infections. J Am Coll Surg 2012;215(2):193-200.
Slide 26: PSSA Followup
- It is crucial that physician and nurse leaders respond to staff concerns about patient safety.
- Your quality team and other leaders must be ready to follow up on the defects identified from the PSSA.
- You will use PSSA data to build your local surgical care improvement bundle.
Slide 27: Next Steps
Present the Science of Safety video and administer PSSA during these ideal times:
- Medical staff grand rounds.
- New staff orientation.
- Regularly scheduled staff meetings (for nurses, anesthesiologists, surgeons, etc.).
- Lunch & Learn sessions.
- Special educator sessions.
- Make video available in break room.
- Hang up Science of Safety factsheet in break room, restroom, etc.
- Annual recertification requirements.
- Hospital intranets.
- Others?
Slide 28: Engage Viewers of Science of Safety Videos
- What are safety events in the clinical area?
- What systems may have led to these events?
- How can the principles of safe design be applied to prevent future events?
- How can staff and others in the clinical area improve communication?
- How can these concepts be applied in this project?
Slide 29: Training Steps and Tools
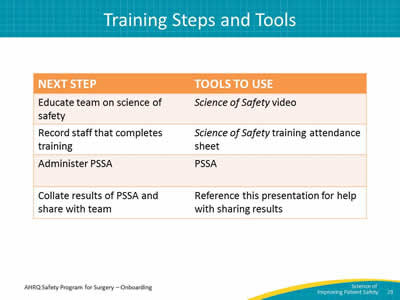
Image: Two-column table with following headings: Next step, Tools to use:
- Educate team with Science of Safety videos.
- Record staff that completes training with Science of Safety training attendance sheet.
- Administer PSSA.
- Collate results of PSSA and share with team and reference this presentation for help with sharing results.
Slide 30: Recap of Learning Objectives
- Apply Science of Safety principles in your work.
- Educate your team and executive partners on the Science of Safety.
- Administer the PSSA to identify defects in your OR.
- Share PSSA results with your team.
- Locate resources on the project Web site to help complete the above tasks.
Slide 31: Lessons Learned
- Every system is designed to achieve the results it gets.
- Recognize the principles of safe design:
- Standardize care.
- Create independent checks.
- Learn from defects.
- Teams make wise decisions when there is diverse input.
- PSSA helps teams identify defects that the team can address.
- Teams can design interventions that prevent defects from occurring in the future.
Slide 32: References
- Pronovost P, Cardo D, Goeschel C, Berenholtz SM, Saint S, Jernigan JA. A research framework for reducing patient harm. Oxford Journals 2011;52(4):507-513. PMID: 21258104.
- World Health Organization. New scientific evidence supports WHO findings: A surgical safety checklist could save hundreds of thousands of lives. http://www.who.int/patientsafety/topics/safe-surgery/checklist/en/. Accessed August 7, 2013.
- Baker DP, Day R, Salas E. Teamwork as an essential component of high-reliability organizations. Health Services Research 2006;41:1576–1598. PMID: 16898980.
- Pronovost P, Goeschel C, Marstellar J, Sexton JB, Pham JC, Berenholtz SM. Framework for patient safety research and improvement. Circulation Journal of the American Heart Association 2009;119:330-337. PMID: 19153284.
Slide 33: References
- Vincent C, Taylor-Adams S, Stanhope N. Framework for analysing risk and safety in clinical medicine. BMJ 1998;316:1154. PMID: 9552960.
- Joint Commission on Accreditation of Healthcare Organizations. Root Causes of Sentinel Events, 1995-2004. www.jointcommission.org/se_data_event_type_by_year_/. Accessed September 21, 2014.
- Dayton E, Henrikson K. Teamwork and communication: communication failure: basic components, contributing factors, and the call for structure. Jt Comm J Qual Patient Saf 2007;31(1):34-47. PMID: 17283940. Figure reproduced with permission of Elizabeth Dayton.
- Wick EC, Hobson DB, Bennett JL, Demski R, Maragakis L, Gearhart SL, Efron J, Berenholtz SM, Makary MA. Implementation of a surgical comprehensive unit-based safety program to reduce surgical site infections. J Am Coll Surg 2012;215(2):193-200. PMID: 22632912.



