Performing SSI Investigations: Slide Presentation
AHRQ Safety Program for Surgery
Slide 1: AHRQ Safety Program for Surgery—Onboarding
Performing an SSI Investigation
Slide 2: Learning Objectives
After this session, you will be able to–
- Explain the difference between process and outcome data.
- Describe how the Surgical Site Infection (SSI) Investigation Tool can guide improvement work even when SSI rates are low.
- Adapt an SSI Investigation Tool to reflect the care processes in your local SSI prevention bundle.
Slide 3: Readiness Bridge
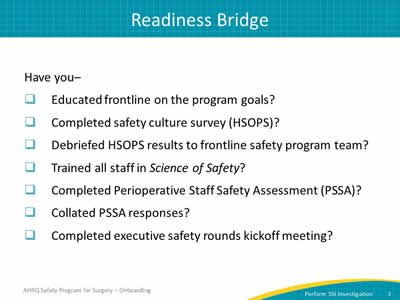
Have you–
- Educated frontline on the program goals?
- Completed safety culture survey (HSOPS)?
- Debriefed HSOPS results to frontline safety program team?
- Trained all staff in Science of Safety?
- Completed Perioperative Staff Safety Assessment (PSSA)?
- Collated PSSA responses?
- Completed executive safety rounds kickoff meeting?
Slide 4: Assess Your Performance
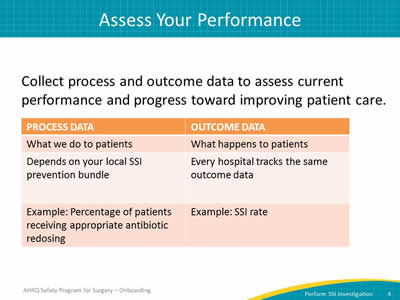
Collect process and outcome data to assess current performance and progress toward improving patient care.
Image: Table with two columns, process data and outcome data:
Process Data
- What we do to patients.
- Depends on your local SSI prevention bundle.
- Example: percentage of patients receiving appropriate antibiotic redosing.
Outcome Data
- What happens to patients.
- Every hospital in AHRQ safety program for surgery is tracking the same outcome data.
- Example: SSI Rate.
Slide 5: Donabedian Process
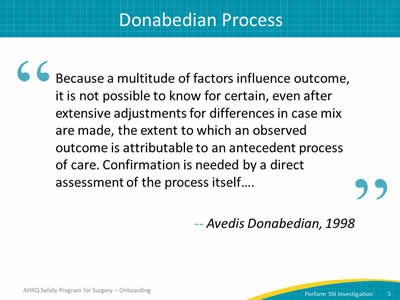
"Because a multitude of factors influence outcome, it is not possible to know for certain, even after extensive adjustments for differences in case mix are made, the extent to which an observed outcome is attributable to an antecedent process of care. Confirmation is needed by a direct assessment of the process itself…."
—Avedis Donabedian, 1998
Slide 6: Identify Defects With SSI Investigation Tool
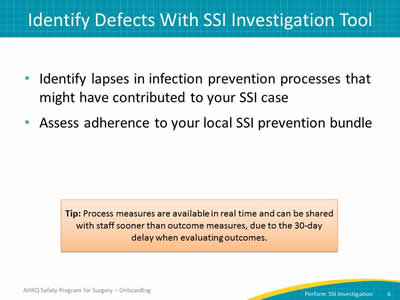
- Identify lapses in infection prevention processes that may have contributed to your SSI case.
- Assess adherence to your local SSI prevention bundle.
Tip: Process measures are available in real time and can be shared with staff sooner than outcome measures, due to the 30-day delay when evaluating outcomes.
Slide 7: Identify Defects With SSI Investigation Tool
Image: Four thumbnails of SSI investigation tool.
Slide 8: Patient or Provider Factors
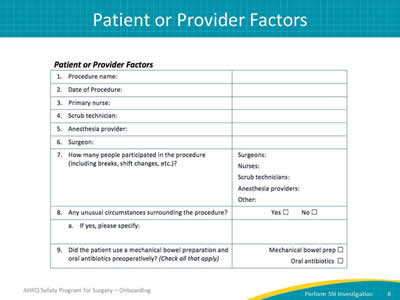
Image: Sample form covering patient or provider factors:
- Procedure name.
- Data of procedure.
- Primary nurse.
- Scrub technician.
- Anesthesia provider.
- Surgeon.
- How many people participated in the procedure (including breaks, shift changes, etc.?
Indicate if Nurses, Scrub techs, Anesthesia provider
- Any unusual circumstances surrounding the procedure?
Indicate Yes or No
If yes, please specify:
- Did the patient use a mechanical bowel preparation and oral antibiotics preoperatively?
Indicate if mechanical bowel preparation or oral antibiotics (Check all that apply)
Slide 9: Normothermia Maintenance
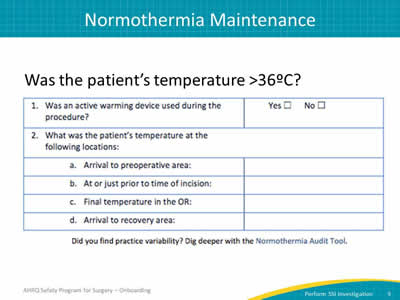
Image: Sample form covering normothermia maintenance:
Was the patient’s temperature greater than 36 ºC?
- Was an active warming device used during the procedure?
Indicate Yes or No
- What was the patient’s temperature at the following locations:
- Arrival to preoperative area
- At or just prior to time of incision
- Final temperature in the OR
- Arrival to recovery area
Did you find practice variability? Dig deeper with Normothermia Audit Tool.
Slide 10: Glucose Control
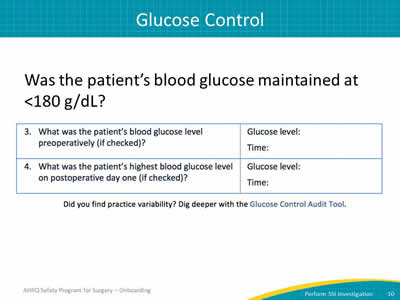
Image: Sample form covering glucose control:
Was the patient’s blood glucose maintained at less than 180 g/dL?
- What was the patient’s blood glucose level preoperatively (if checked)?
- Indicate Glucose level and Time.
- What was the patient’s highest blood glucose level on postoperative day one (if checked)?
- Indicate Glucose level and Time.
Did you find practice variability? Dig deeper with Glucose Control Audit Tool.
Slide 11: Skin Preparation
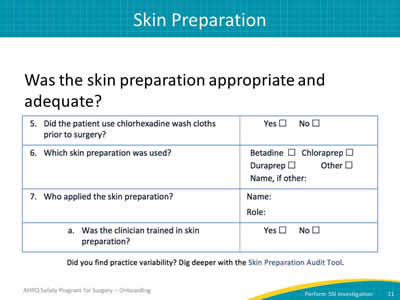
Image: Sample form covering skin preparation:
Was the skin preparation appropriate and adequate?
- Did the patient use chlorhexidine washcloths prior to surgery?
Indicate Yes or No
- Which skin preparation was used?
Indicate Betadine, Chloraprep, Duraprep, Other (Name, if Other)
- Who applied the skin preparation?
- Was the clinician trained in skin preparation?
Indicate Yes or No
- Was the clinician trained in skin preparation?
Did you find practice variability? Dig deeper with the Skin Preparation Audit Tool.
Slide 12: Prophylactic Antibiotics
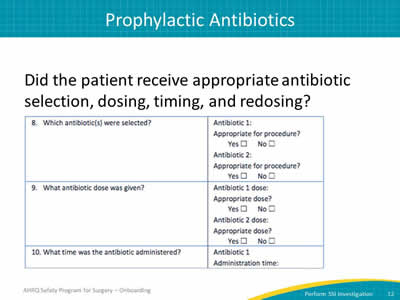
Image: Sample form covering prophylactic antibiotics:
Did the patient receive appropriate antibiotic selection, dosing, timing, and redosing?
- Which antibiotic(s) were selected?
Indicate name of antibiotic 1
Indicate if appropriate for procedure (Yes or No)
Indicate name of antibiotic 2
Indicate if appropriate for procedure (Yes or No)
- What antibiotic dose was given?
Indicate value for Antibiotic 1 dose
Indicate if appropriate dose? (Yes or No)
Indicate value for Antibiotic 1 dose
Indicate if appropriate dose? (Yes or No)
- What time was the antibiotic administered?
Indicate name of antibiotic 1
Indicate administration time for antibiotic 1
Indicate name of antibiotic 2
Indicate administration time for antibiotic 2
Slide 13: Prophylactic Antibiotics
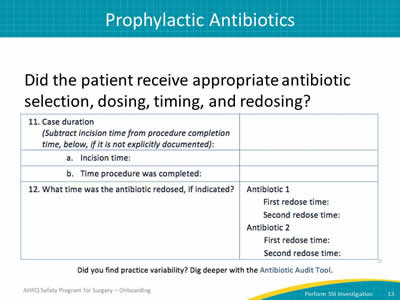
Did the patient receive appropriate antibiotic selection, dosing, timing, and redosing?
Image: Sample form covering prophylactic antibiotics:
- Case duration.
(Subtract incision time from procedure completion time, below, if it is not explicitly documented.)
- Indicate incision time.
- Indicate time procedure was completed.
- What time was the antibiotic redosed, if indicated?
- Indicate antibiotic 1 name.
- Indicate first redose time.
- Indicate second redose time.
- Indicate antibiotic 2 name.
- Indicate first redose time.
- Indicate second redose time.
Did you find practice variability? Dig deeper with the Antibiotic Audit Tool.
Slide 14: Adapt the SSI Investigation Tool
- Johns Hopkins Hospital clinicians designed this tool to assess adherence to their SSI prevention bundle.
- Your team may want to investigate care processes not included in this tool.
- This tool may include processes your team does not use.
- Use the example to get your team started.
Tip: Please modify the SSI Investigation Tool to best fit your team’s needs. The tool provides a starting point for your efforts.
Slide 15: What Your Team Can Do
- Pull this information from the patient’s chart.
- Use SSI audit tools to dig deeper into your care delivery system.
- Present process data to the team at a routine safety program for surgery meeting.
- Share investigation results with your operating room leadership and frontline staff.
Slide 16: Next Steps
- Complete an investigation of your most recent SSIs.
- Share your findings.



