Sustainability: Learning From Defects: Slide Presentation
AHRQ Safety Program for Surgery
Slide 1: AHRQ Safety Program for Surgery—Sustainability
Sustainability: Learning From Defects
Slide 2: Learning Objectives
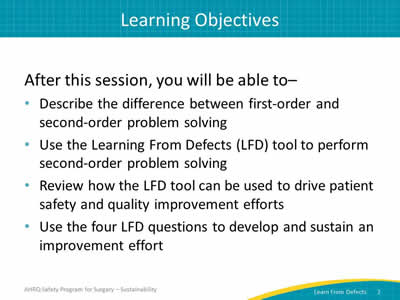
After this session, you will be able to–
- Describe the difference between first-order and second-order problem solving.
- Use the Learning From Defects (LFD) tool to perform second-order problem solving.
- Review how the LFD tool can be used to drive patient safety and quality improvement efforts.
- Use the four LFD questions to develop and sustain an improvement effort.
Slide 3: AHRQ Safety Program for Surgery
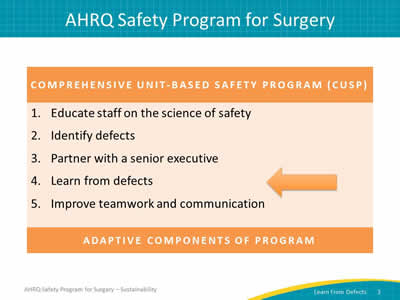
Comprehensive Unit-based Safety Program
- Educate staff on the science of safety.
- Identify defects.
- Partner with a senior executive.
- Learn from defects.
- Improve teamwork and communication.
Adaptive Components of Program
Image: An arrow indicates Step 4: Learn from defects.
Slide 4: Problem-Solving Hierarchy
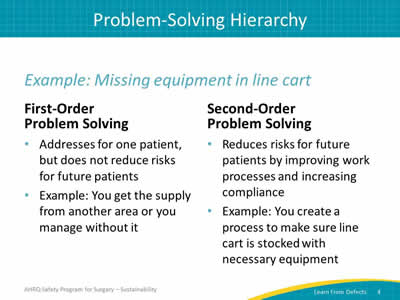
Example: Missing equipment in line cart
First-order problem solving
- Addresses for one patient, but does not reduce risks for future patients.
- Example: You get the supply from another area or you manage without it.
Second-order problem solving
- Reduces risks for future patients by improving work processes and increasing compliance.
- Example: You create a process to make sure line cart is stocked with necessary equipment.
Slide 5: Problem Solving Goal: Long-Term Solution
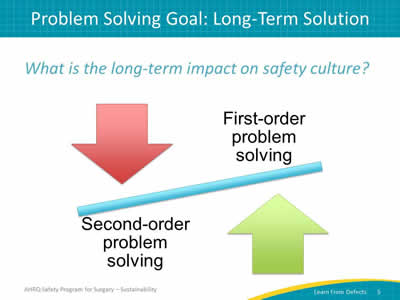
What is the long-term impact on patient safety culture?
Image: See-saw presentation of arrows pointing towards the balancing line. Red arrow pointing down is captioned "First-order problem-solving." Green arrow pointing up is captioned "Second-order problem-solving."
Slide 6: What Is a Defect
Anything you do not want to happen again.
Image: Man wearing jeans and orange/black striped t-shirt sitting with hands raised to chin height with fingers outstretched in a questioning manner.
Slide 7: Individual Mistake or System Failing?
“Rather than being the main instigators of an accident, operators tend to be the inheritors of SYSTEM defects. . . . Their part is that of adding the final garnish to a lethal brew that has been long in the cooking.”
— James Reason, Human Error, 19901
Slide 8: AHRQ Safety Program for Surgery—Sustainability
Sustaining your patient safety initiatives
Learning From Defects
Slide 9: Learning From Defects2,3,4
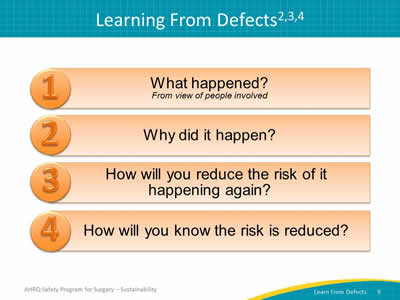
Image: Four numbered blue boxes list the Learning From Defects questions:
- What happened? (From view of person involved)
- Why did it happen?
- How will you reduce the risk of it happening again?
- How will you know the risk is reduced?
Slide 10: What Happened?

Walk the process.
- Reconstruct the timeline and reenact what happened.
- Dig down to the reasoning and emotions behind actions and decisions.
- Consider using visualization tools to break down complex defects and discover where steps go wrong.
- Process mapping.
- Diagrams.
- Sketches.
- Role playing.
Tip: Take time to listen. Seek to understand rather than to judge. Ask clarifying questions and followup questions.
Slide 11: What Happened?
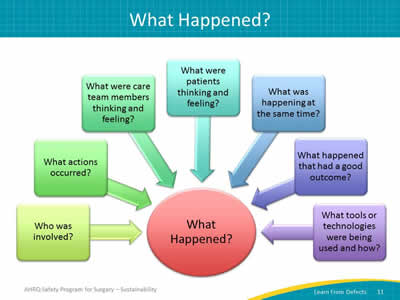
Image: Questions to ask to learn what happened. Questions are in color boxes with arrows pointing to a large circle in the center that reads, "What Happened?"
- Who was involved?
- What actions occurred?
- What were care team members thinking and feeling?
- What were patients thinking and feeling?
- What was happening at the same time?
- What happened that had a good outcome?
- What happened that had a bad outcome?
- What tools or technologies were used and how?
Slide 12: Why Did It Happen?
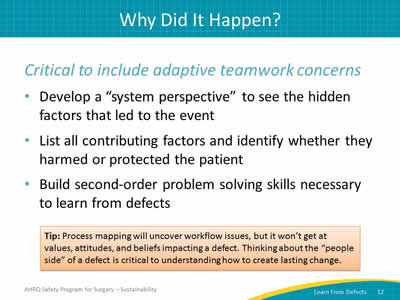
Critical to include adaptive teamwork concerns.
- Develop a “system perspective” to see the hidden factors that led to the event.
- List all contributing factors and identify whether they harmed or protected the patient.
- Build second-order problem solving skills necessary to learn from defects.
Tip: Process mapping will uncover workflow issues, but it won’t get at values, attitudes, and beliefs impacting a defect. Thinking about the “people side” of a defect is critical to understanding how to create lasting change.
Slide 13: How Will You Reduce Risk of Recurrence?
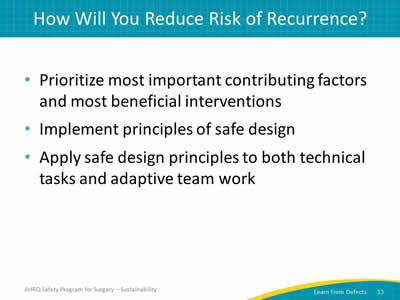
- Prioritize most important contributing factors and most beneficial interventions.
- Implement principles of safe design.
- Apply safe design principles to both technical tasks and adaptive team work.
Slide 14: How Will You Reduce Risk of Recurrence?
Take advantage of your diverse team.
- Leverage senior executive’s big-picture view of the organization and both knowledge of and access to resources.
- Defer to expertise of surgeon, nurses, and technicians.
- Use team members’ connections throughout organization.
- Tap into the wisdom of frontline staff with particular insight into the defect.
Slide 15: Prioritizing Interventions
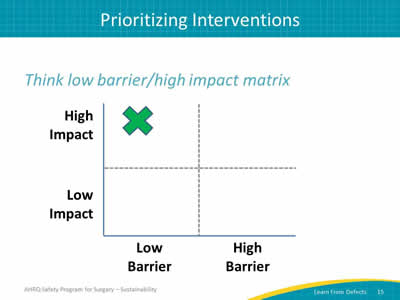
Think low barrier/high impact matrix.
Image: A grid matrix to prioritize interventions. X-axis is for barriers (low on left, growing to high barriers on the right). Y-axis is for impact (Low impact growing to high impact). An "X" marks the first quadrant, labeled High Impact and Low Barrier.
Slide 16: How Will You Reduce Risk of Recurrence?
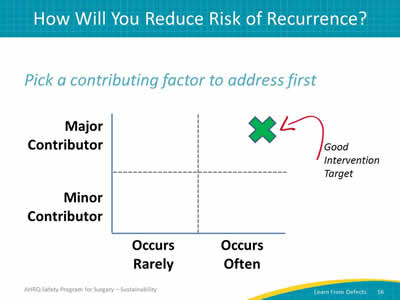
Pick a contributing factor to address first.
Image: A grid matrix to prioritize contributing factors. X-axis is for the frequency of the factor (occurs rarely on left growing to occurs often on the right). Y-axis is for the contribution the factor makes to the defect (minor contributor on the bottom growing to major contributor on the top). An "X" marks the second quadrant labeled Major Contributor and Occurs Often.
Slide 17: Principles of Safe Design
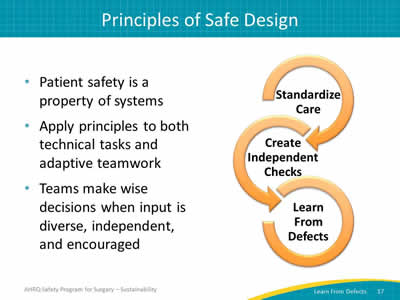
- Patient safety is a property of systems.
- Apply principles to both technical tasks and adaptive teamwork.
- Teams make wise decisions when input is diverse, independent, and encouraged.
Image: A series of interlocking circular arrows to connect three concepts:
- Standardize care.
- Create independent checks.
- Learn from defects.
Slide 18: Rank Order of Error Reduction Strategies5
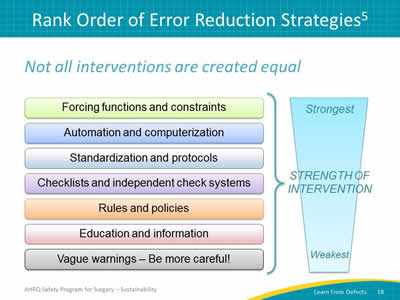
Image: Chart captioned "Strength of Interventions" showing ranked list of interventions with the strongest options at the top and the weakest interventions at the bottom:
- Forcing functions and constraints.
- Automation and computerization.
- Standardization and protocols.
- Checklists and independent check systems.
- Rules and policies.
- Education and information.
- Vague warnings—Be more careful!
Slide 19: How Will You Know Risks Were Reduced?
- Do staff members know about the interventions?
- Are staff members using the interventions as intended?
- Do staff members believe risks were reduced?
- Use data-driven metrics whenever possible.
Tip: Identify ways to measure success. Data is king, but subjective evaluations can provide valuable information. Ask your frontline staff about intervention compliance and effectiveness.
Slide 20: Share Success Stories
- Summarize findings and changes over time:
- Hospital Patient Safety Culture Survey (HSOPS).
- Safety Attitudes Questionnaire (SAQ).
- Share updates on initiatives and success stories to maintain engagement.
Tip: Some hospital units make staff safety assessments (refers to asking staff how the next patient will be harmed) available at all times. The team should review feedback on an ongoing basis.
Slide 21: What's Next?
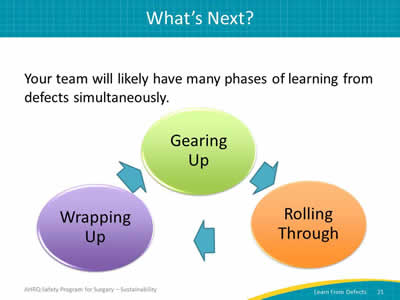
Your team will likely have many phases of learning from defects simultaneously.
Image: Circular process of varying stages of LFD life cycle. Three circles in a clockwise circle formation with interconnecting arrows.
- Gearing up.
- Rolling through.
- Wrapping up.
Slide 22: Turnover Happens
- Personnel turnover impacts all areas of organization:
- Frontline staff and clinicians.
- Executive officers.
- Patient safety team members.
- Invite new team members as defects evolve.
- Rotate existing team members as needed.
- Cultivate a depth of people with diverse experiences and exposures.
Slide 23: Key Takeaways
- Focus on systems, not people.
- Prioritize contributing factors and interventions.
- Use safe design principles.
- Go a mile deep and an inch wide rather than a mile wide and an inch deep.
- Learn from defects on a regular basis.
- Ask staff regularly what defects need attention.
Slide 24: Action Plan
- Review the Learning From Defects tool with your team.
- Review a defect in your operating rooms.
- Select one defect per month.
- Consider using in surgical morbidity and mortality conferences.
- Post the stories of reduced risks (with data!).
- Share with others.
Slide 25: References
- Reason J. Human Error: models and management. BMJ 2000;320:768-70. PMID: 10720363.
- Pronovost PJ, Holzmueller CG, Martinez E. A practical tool to learn from defects in patient care. Jt Comm J Qual Patient Saf 2006;32(2):102-8. PMID: 16568924.
- Pronovost P, Cardo D, Goeschel C, et al. A research framework for reducing patient harm. Oxford Journals 2011;52(4):507-13. PMID: 21258104.
- Wu AW, Lipshutz AKM, Pronovost PJ. The effectiveness and efficiency of root cause analysis. JAMA 2008;299:685-7. PMID: 18270357.
- Institute for Safe Medication Practices. Selecting the best error-prevention "tools" for the job. 2006. https://www.ismp.org/newsletters/ambulatory/archives/200602_4.asp. Accessed August 26, 2015.



