Sustaining and Spreading Surgical Safety Improvements: Slide Presentation
AHRQ Safety Program for Surgery
Slide 1: AHRQ Safety Program for Surgery—Sustainability

Sustaining and Spreading Surgical Safety Improvements
Slide 2: Learning Objectives
After this session, you will be able to–
- Define sustainment and spread.
- Determine if you are ready to sustain.
- Plan key actions for sustainment.
- Prioritize needs for successful sustainment.
Slide 3: Sustainment Is…
- What you do to continue to build on your successes.
- How your efforts to change culture and improve safety persist.
- When you apply the process for improving surgical safety to new challenges.
Slide 4: Adaptive or Technical?
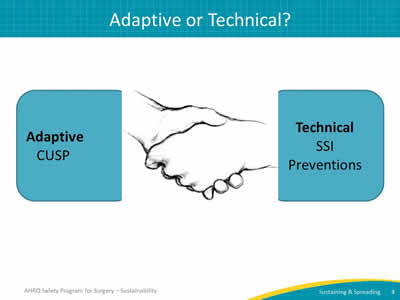
Image: The two sides of quality improvement work, Adaptive and Technical, are illustrated by two hands shaking flanked by the captions "Adaptive CUSP" and "Technical SSI Preventions".
Slide 5: Why Worry About Sustainment
- Avoid recidivism, or backsliding.
- Respect probability of failure over time.
- Recognize risks to sustaining progress:
- Staff turnover.
- Overlying priorities.
- Organizational changes.
Slide 6: Definition of Spread1
“Spreading takes the process from the narrow, segmented population(s) or group(s) and broadens it to include all the population(s) or group(s) that will use the process.”
“Formalizing a process provides a reference to others: those new to the organization and those in the organization needing clarity about the specifics of the process.”
Image: A team of providers steadily growing to include a range of providers, patients, and family members.
Slide 7: What Do Effective Teams Look Like?
Effective teams–
- Hold regular meetings.
- Include active surgical champions who partner with others.
- Have executive leadership support.
- Believe that progress is possible.
- Invent ways to create engagement (and then reinvent more ways).
- Maintain frequent communication.
Slide 8: What Sustainment Strategies Work?
- Stick to formal processes:
- Test changes on small scale first.
- Measure and make data-driven decisions.
- Maintain access to continuous feedback:
- Require current data to validate progress.
Slide 9: What Sustainment Strategies Work?
- Secure time and resources:
- Formalize job responsibilities for patient safety improvement work.
- Dedicate financial resources and personnel, including protected time.
- Make data support available.
- Take care of your team:
- Plan for team growth and turnover.
- Offer highly engaged team members professional development opportunities.
Slide 10: We Are Ready to Sustain: Now What?
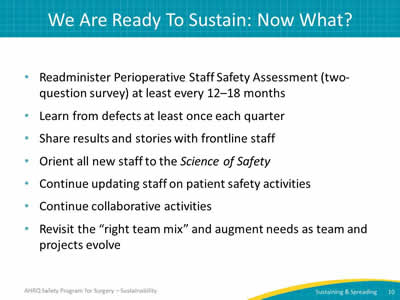
- Readminister Perioperative Staff Safety Assessment (two-question survey) at least every 12–18 months.
- Learn from defects at least once each quarter.
- Share results and stories with frontline staff.
- Orient all new staff to the Science of Safety.
- Continue updating staff on patient safety activities.
- Continue collaborative activities.
- Revisit the “right team mix” and augment needs as team and projects evolve.
Slide 11: Preview of Premortem2
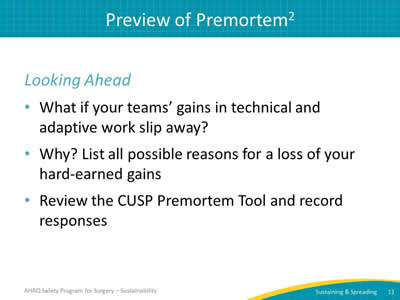
Looking ahead
- What if your teams’ gains in technical and adaptive work slip away?
- Why? List all possible reasons for a loss of your hard-earned gains.
- Review the CUSP Premortem Tool and record responses.
Slide 12: References
- North Carolina Center for Hospital Quality and Patient Safety. North Carolina Prevent Catheter-Associated Urinary Tract Infections Collaborative. North Carolina; 2010.
- Klein G. Performing a Project Premortem. Harvard Business Review. Sept 2007. https://hbr.org/2007/09/performing-a-project-premortem. Accessed Aug 22, 2015.



