Module 4: How To Implement the Fall Prevention Program in Your Organization—Training Guide
Module Aim
The aim of this module is to support your efforts in implementing the new prevention practices at the patient care level.
Module Goals
The goals of Module 4 are to have the Implementation Team determine how to successfully implement changes to your program by answering the following questions:
- What roles and responsibilities will staff have in preventing falls?
- What fall prevention practices go beyond the unit (e.g., when patients are transferred for tests)?
- How do you put the new practices into operation?
- How can you help staff learn new practices?
Timing
This module will take 55 minutes to present.
Allow approximately 25 minutes to present slides 1–27. That leaves approximately 30 minutes for assessment of current staff education and training (Slide 28).
Learning Methodology Checklist
- Large group discussion.
- PowerPoint slide presentation.
- Group planning activities.
Additional Related Training Resources
- Staff Roles and Training for Your Fall Prevention Program—AHRQ Fall Prevention Program Training Webinar.
- Critical Thinking for Fall Injury Prevention—AHRQ Fall Prevention Program Implementation Sharing Webinar.
- DMAIC: A Deep Dive into Reducing Patient Falls—AHRQ Fall Prevention Program Implementation Sharing Webinar.
Materials Checklist
- LCD projector and laptop.
- “Parking Lot” flip chart page (with tape or sticky band and markers).
- Flip chart “Best Practices” page completed by the Implementation Team during Module 3. Keep this page on the tripod or taped to the wall in clear view of the participants.
Instructor Preparation
- Add the specific hospital name to the first slide.
- Have the PowerPoint file Module 4 cued on the computer and minimized.
- Participants should have Tool 2F: Action Plan available, as they will continually add to it in each module.
- Ask the Implementation Team Leader to work with the manager of the pilot unit(s) prior to this training to identify Unit Champions for each shift on each pilot unit. (Refer to page 56 in the Toolkit for characteristics of a good Unit Champion.)
- Ask the Implementation Team Leader to assign a Task Force Leader to think about which staff roles will be responsible for performing the best practices tasks using Tool 4B: Staff Roles. (See Slide 10, where the Implementation Team Leader will be asked to assign a Task Force Leader and then ask for volunteers to be on the small Task Force.)
- Alert the Implementation Team Leader(s) or designee(s) to be ready to present findings from Tool 4C: Assessing Staff Education and Training and to lead a group planning discussion of an Action Plan for this education.
- Alert the information technology (IT) representative on the Implementation Team to be ready to talk about the following topics during this module:
- The electronic health record (EHR) and the possibility of building fall prevention into the electronic documentation system.
- How to use electronic communication modalities to communicate the program’s progress and success to the rest of the hospital staff.
- Have a copy of the following materials for all participants:
- Tool 4A: Assigning Responsibilities for Using Best Practices.
- Tool 4B: Staff Roles.
- Tool 4C: Assessing Staff Education and Training (completed by the Implementation Team Leader or designee).
- Tool 4D: Implementing Best Practices Checklist.
Module 4: How To Implement the Fall Prevention Program in Your Organization
| Slide | Script |
|---|---|
|
Slide 1
|
Say: In this module, we begin planning for implementation of your hospital’s Fall Prevention Plan and best practices. |
|
Slide 2
|
Say: Up to this point, you have:
|
|
Slide 3
|
Say: Our work in this module centers around the Implementation Team interacting with the Unit Teams to implement new prevention practices at the patient care level. This is where the rubber meets the road. For any prevention program to succeed, the staff must understand and use the best practices you have outlined. |
|
Slide 4
|
Say: There are many goals when planning for implementation, such as determining the roles and responsibilities of staff in preventing falls. You need to answer:
This last point is crucial, because once patients are off the unit floor, other hospital Team members in those testing areas are now responsible for the patients’ care and need to know they are at risk for falls. |
|
Slide 5
|
Say: Another implementation planning goal is to put new evidence-based practices into operation. The questions to ask your Team are:
As suggested in Module 2, the change process of rolling out new practices tends to be most successful when teams follow a systematic approach to analysis and implementation, such as in the Plan, Do, Study, Act improvement process. (This is discussed on page 21 of the Toolkit.) Consider implementing small tests of change, whereby one staff nurse tries out the new practice for 1 day, and then two or more nurses implement the new practice for 1 or 2 days. This systematic approach helps to work out any problems and perfect a new practice before rolling it out to the whole unit. We can’t answer all these questions today, but they are points to ponder as you plan to implement a Fall Prevention Program. |
|
Slide 6
|
Say: Think about who will perform each specific task identified for your set of best practices. Assign responsibilities based on the formal training and informal work experience of each individual. |
|
Slide 7
|
Say: In some cases, a group will perform a task based on their specific role or title, such as certified nursing assistants (CNAs). Other tasks may be assigned to a specific individual. In that case, always ensure you have a backup and that everyone knows who the backup is. |
|
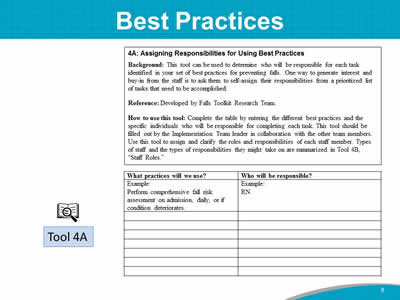
Slide 8
|
Do: Ask participants to take out Tool 4A: Assigning Responsibilities for Using Best Practices. Say: The Implementation Team decided on a preliminary list of best practices this morning in Module 3. The best practices to be incorporated at your hospital are (best practices selected by the group). Do: Refer to the flip chart “Best Practices” page completed by the Implementation Team during Module 3. Read the best practices listed on the flip chart page and ask the participants to write the preliminary list of best practices on Tool 4A. If you haven’t prioritized the list of opportunities for change or decisions on best practices, tell the group that this activity using Tool 4A will be done at a later meeting of the Implementation Team. |
|
Slide 9
|
Say: The next step is to decide who will be responsible for carrying out the tasks necessary to implement best practices at the unit level. |
|
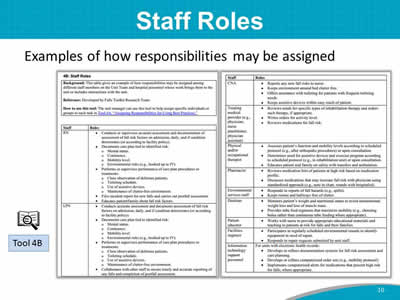
Slide 10
|
Say: Look at Tool 4B. Think about who will be responsible for performing the best practice tasks. Tool 4B includes examples of how responsibilities may be assigned among different staff members on the Unit Team and among hospital personnel whose work brings them to the unit or includes interactions with the unit. The task of assigning staff roles for performing the identified best practices using Tools 4A and 4B is best assigned to a small Task Force of the Implementation Team. Because of time constraints, this activity is one we can’t accomplish during this training today. What we can do is assign or ask for volunteers to be on this Task Force. This topic may be an agenda item for one of the first Team meetings. Do: Ask the Implementation Team Leader to appoint the Task Force Leader and then ask for volunteers to serve on the Task Force. |
|
Slide 11
|
Say: The staff who will be assigned these best practice responsibilities are considered the Unit Team. The Unit Team comprises staff members who provide daily direct patient care by:
|
|
Slide 12
|
Say: The Unit Team includes everyone on the unit, such as:
The patient and family are also members of the Team. (See page 55 of the Toolkit for more information on the Unit Team.) |
|
Slide 13
|
Say: All hospitals experience staff turnover. Staff turnover tends to make it difficult to keep staff adequately trained and up to speed on prevention efforts. Make sure that fall prevention is included in new staff or travel staff training. It is especially difficult when someone on the Implementation Team takes another position. It is helpful to have a plan or process in place to identify a replacement for each role on your Implementation Team. This plan for turnover on the Team should include specific training for that role. Ask: What are the challenges of staff turnover at your hospital? |
|
Slide 14
|
Say: Here’s how one hospital has addressed nursing turnover. It planned a 1-year residency program for new-graduate nurses to help retain new-hire graduate nurses (RNs). The goal is to provide specific orientation and on-the-job training to empower new RNs to learn and be confident in their skills. The new-graduate nurse program is usually a class of 30 RNs. The program consists of the following:
The outcome of this residency program is an 85 to 95% 2-year retention rate of new-graduate RNs. Recently, the main reasons for losing new graduate RNs early has been the travel nurse allure or wanting a nurse specialty that this hospital doesn’t have. While there are no simple solutions for addressing staff turnover, it will be critical for you to plan for it as you move forward with your Fall Prevention Program. |
|
Slide 15
|
Do: If Unit Champions have been identified before training, introduce them to the group if they are in the room. Otherwise, read the list of Unit Champion names. Say: Many successful improvement efforts rely on Unit Champions, especially during the implementation process. The Unit Champion is a staff member who serves as the liaison between the Implementation Team and the unit staff. The Unit Champion is familiar with the program goals, care processes, and outcome data that will be used. The Unit Champion will need to be oriented to the Fall Prevention Program prior to implementation. The Unit Champion is the go-to person when staff members have questions. Ideally, there should be one champion per shift to provide guidance to other staff. |
|
Slide 16
|
Say: Communication needs to occur among staff at all levels. It needs to occur:
|
|
Slide 17
|
Say: A communication process will need to be devised to share information about the effectiveness of implemented changes. The Unit Champions can present updates on the implementation of new changes at regularly scheduled meetings of the Implementation Team. The communication process should be regular and thorough with the least amount of time and effort. |
|
Slide 18
|
Say: Building new fall prevention practices into ongoing work processes is necessary for sustainability. Strategies for building prevention into ongoing processes include:
Ask: Does anyone have any ideas about who in your hospital may be able to help create visual cues? Perhaps a public relations or communications professional? (For examples of how change can be incorporated into routine care, see page 58 in the Toolkit.) The next slide addresses how to use the electronic health record to integrate best practices. |
|
Slide 19
|
Say: Electronic health records provide additional opportunities to integrate best practices into the daily routine. Questions to consider with electronic records include:
(Additional suggestions for building fall prevention into electronic documentation systems can be found on page 59 of the Toolkit.) Instructor’s Note: If a member of the IT Department is on the Implementation Team, he or she can discuss possible changes to the system. Ask: Can the IT representative, (name), speak to the possibility of building fall prevention processes into the electronic documentation system? |
|
Slide 20
|
Say: Incorporating a new set of practices involves changes in the way people work. To manage the change process more efficiently, consider doing the following:
|
|
Slide 21
|
Say: Identify and minimize practical barriers to using the new practices, such as inadequate access to supplies and equipment. For example, these items should be stored on or near the unit for easy availability:
At all levels, engage staff to gain their support and buy-in to the improvement effort, and help tailor the practices in fall prevention. Encourage staff to speak up if supplies and equipment are lacking, missing, or broken. |
|
Slide 22
|
Say: The Implementation Team and Unit Champions should develop a process for ongoing monitoring of implementation progress. It’s very important to collect baseline measurements of fall rates and current practices before implementing any changes. The monitoring process should include outcome measures, such as tracking changes in fall rates. Tracking the care processes to prevent falls is a measure of implementation success and should translate into better outcomes. Then, you will want to communicate the results from tracking to staff and the Implementation Team. We will discuss tracking fall rates in more depth in Module 5. |
|
Slide 23
|
Say: Tips for how to convey updates and information on successes from the prevention activities include using:
Ask: Does anyone have suggestions for how to convey program updates and successes to the hospital at large? How can IT professionals help communicate program successes? |
|
Slide 24
|
Say: To help sustain the Fall Prevention Program, ensure senior leaders and middle managers know about the results from tracking. Share this information on a regular basis. Leaders and managers can help remove barriers across departments and authorize resources for the prevention initiatives. Keeping senior administrative leadership in the know and involved in the Fall Prevention Program is key to sustaining the program long term. Engaging the buy-in and ongoing participation of staff members who are involved in hands-on care is important. Their engagement is crucial to achieve the improvement objectives. Communicate with clinical staff about the progress that has been made in fall prevention. Clinical staff need to hear the information. Let’s do a quick brainstorm of how to keep leadership and staff involved. Ask: What creative ideas would you suggest to best share tracking results or brief vignettes of success stories about the program? Is there a hospital staff member who does this kind of work? |
|
Slide 25
|
Say: Let’s turn now to staff education and training. How can you help staff learn new practices? You may want to craft an education plan to enhance staff knowledge on fall prevention. Adult learning theory suggests that adults learn best through methods that build on their own experiences. We also want to remember that we should provide prevention education to the patient and his or her family members and significant others. Tool 3L (Patient and Family Education) provides an example. Because individuals have different learning styles, and they are at different levels of practice proficiency, a variety of educational approaches is best, including didactic methods such as lectures, interactive presentations, online lessons, case-study analysis, listserv discussions, grand-rounds talks, and mentoring and coaching. |
|
Slide 26
|
Say: Let me provide you with an example of how to incorporate just-in-time coaching into your frontline staff training. This example comes from a hospital that implemented AHRQ’s Preventing Falls in Hospitals Toolkit. This hospital was working to have its patient care technicians, or PCTs, implement bedside handoffs of patients. During the early implementation of this intervention, unit leaders found that PCT bedside handoffs were not being implemented as planned. They learned that some staff believed it was rude to have conversations in front of the patients. To address this issue, leaders had conversations with and coached staff about why this intervention was being done and how to do it in a respectful and helpful way that includes the patient. They reinforced this practice during staff meetings and huddles. Leaders continue to talk with staff about the benefits of this practice: If they complete the handoffs as expected, their patients will be less likely to fall. They also continue personal coaching to support staff member growth. |
|
Slide 27
|
Say: You will also want to ensure staff members follow your hospital’s Fall Prevention Plan, so it is a good idea to have ongoing training to help remind staff of fall prevention strategies. Fall prevention should be included in four areas of training:
|
|
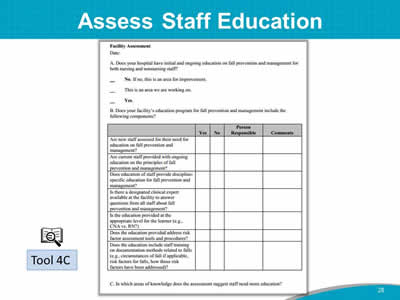
Slide 28
|
Say: The Implementation Team Leader or designee, (name of person who did the training assessment), in collaboration with other Team members, assessed current staff education practices on fall prevention using Tool 4C. Keep in mind, the purpose of assessing staff education is to identify where there may be room for improvement. Do: Distribute copies of completed Tool 4C. Say: I’d like to ask (name of Implementation Team Leader or designee) to review the current fall prevention staff education with you and lead a discussion about staff training needs. Do: Have Implementation Team Leader or designee review completed Tool 4C and lead a discussion about staff training needs. |
|
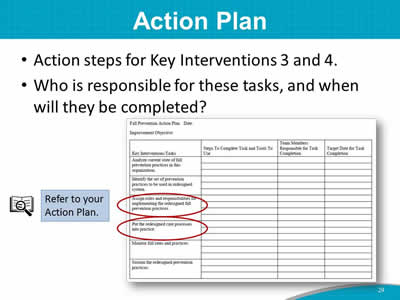
Slide 29
|
Say: Your staff roles Task Force will come up with a plan for assigning staff roles and responsibilities, which will become the information for Key Intervention 3. Key Intervention 4 includes steps to put the redesigned set of practices into operation, including staff education needs. |
|
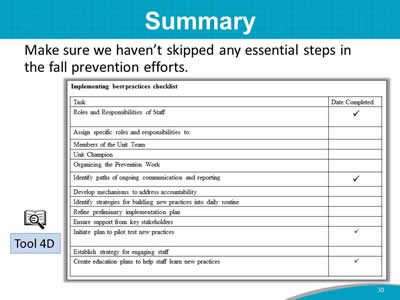
Slide 30
|
Say: Let’s end this module by looking at the checklist for implementing best practices. To summarize, we addressed the following points in this module:
Once again, you have accomplished a heroic amount of planning for your Fall Prevention Program. Let’s take a break and then move on to Module 5. |