This section of the toolkit describes key factors that promote success in quality improvement (QI) initiatives and provides supportive resources. It describes the settings and the multiple factors that impact the asthma ED measure. You can navigate directly to the Approaches to Quality Improvement in Asthma Care section.
The toolkit also provides more detailed guidance on implementing primary care learning collaboratives based on the experiences from two initiatives that aimed at reducing ED use among pediatric asthma patients and examining the asthma ED use measure. Navigate directly to the Quality Improvement with a Focus on Primary Care Delivery section.
Within that section, the toolkit presents a “phased” approach to QI so that users can tailor their goals and strategies based on their prior experience in implementing QI activities. Practices with limited or no prior QI experience are encouraged to start with Phase 1, initiating a learning collaborative to assess and improve NHLBI guideline adherence in primary care. For practices with prior experience implementing NHLBI guidelines and using QI strategies, this toolkit describes a “deep dive” approach to improve existing processes, designated Phase 2.
Key Success Factors for Quality Improvement
The PQMP measure, Pediatric Asthma Emergency Department (ED) Use, is an outcome measure based on administrative data. In that context, the toolkit user entity (state agency, health plan, healthcare organization, improvement partnership, provider group) will need to partner with practices and quality improvement (QI) coaches to evaluate systems and develop process measures to guide improvement efforts that will impact the measure. Process measures can be developed from clinical guidelines such as the National Heart Lung and Blood Institute (NHLBI) Guidelines for the Diagnosis and Management of Asthma (PDF, 3.64 MB)
It is important to recognize that most process measures will be contained in a practice’s electronic health record (EHR) or a data source separate from claims data. Additionally, effective process measures should be evaluated longitudinally to assess performance over time and allow for identification of variation, either intended or unintended.
Successful improvement requires sound QI science methodology, appropriate resources and ready access to reliable data. Without these components (appropriate training, infrastructure and data access), application of QI may lead to unintended consequences, such as provider frustration or QI ‘fatigue’.
The table below summarizes the strategies and complementary toolkit resources available to support implementing quality measurement and improvement strategies in primary care settings to reduce asthma-related ED visits from the perspective of a health plan.
Summary of Strategies and Complementary Toolkit Resources
| Goal | Resources Required | Resources in Toolkit | Health Plan Contributions |
|---|---|---|---|
| Strategy: Improvement Science Approach | |||
| Appreciate the system of care for children with asthma | Understand the population and the system resources in your care delivery area | Refer to PQMP National Asthma Quality Metric Key Driver Diagram (PDF, 180 KB) | Foster partnerships and determine strategic alignment(s) |
| Strategy: Collaborative | |||
| Partner with practices in Health Plan network | Practice network | Engage practices in collaborative | |
| Engage practice leadership | Practice champion | Financial alignment for clinical champion(s) | |
| Develop improvement science expertise | QI Coaching | Refer to QI Knowledge Survey (PDF, 208 KB) | Offer financial support for QI infrastructure |
| Determine baseline performance on NHLBI measures | Process measures from EHR | Refer to Baseline Chart Review Tool (PDF, 333.5 KB) | Support practices to engage EHR vendor/ practice support to obtain data |
| Assess periodic performance/ improvement over time | Refer to measures monitored by the SF Collaborative (PDF, 259 KB) | Develop practice-based incentives for improvement | |
| Understand variation in performance and guide improvement efforts | Practice level strategies | Refer to OSI tool (PDF, 237 KB) | |
| Strategy: Continuous Improvement | |||
| Systems learning | Practice data of children who went to ED | Refer to Practice Participation Flow Chart (PDF, 150 KB) | Health plan provides practice reports |
| Systems learning | Practice-based clinician(s)/ chart auditor | Refer to Practice Data Collection Form (PDF, 323 KB) | |
Approaches to Quality Improvement in Asthma Care
This section introduces the range of approaches aimed at decreasing pediatric asthma ED visits and important factors for determining which approach may be most appropriate to take. Specific guidance on implementing a primary care learning collaborative is provided in the next few sections.
There are numerous factors and settings that impact the asthma ED measure (e.g., schools, ED, acute care, access to specialists, community, etc.), and these must be considered in trying to reduce inappropriate ED use for pediatric asthma. Many factors can lead to a child with asthma receiving care in the ED such as poor asthma control, severity of symptoms, decreased access to care, and ability to enact emergency care (such as use of a rescue inhaler) among many others. When thinking of these factors and where they occur, they generally can be attributed to the patient’s home and school environment, medical home, the ED, or a combination (Allen, 2019). Interventions engaging the ED should be considered if there is a high rate of patients with multiple visits to the ED. In this scenario, it is important to evaluate access to care, environmental factors, ED care, and the connection between the ED and the medical home.
Though there are several evidence-based QI strategies to decrease ED visits for pediatric asthma, there is insufficient evidence to recommend a single approach or set of interventions over another because there are many factors that influence what will be the most effective approach for a care system. Some systems with a high degree of integration and QI capacity have chosen multiple interventions to reduce ED visits (Allen, 2019). However, most care systems will likely be best served by selecting a single approach after evaluating their outcome and process measures while identifying the key drivers of performance. Assembling an interprofessional team to understand key stakeholder priorities and readiness coupled with a thorough and systematic approach to QI are essential to achieving success.
There are three general QI approaches to decrease pediatric ED visits for asthma that have a strong evidence base: Primary Care, Provider Continuing Medical Education, and Parental and School-Based. Following an overview of each approach, there is a brief introduction to the primary care learning collaboratives, one of which was formed as part of the PQMP grant, that examine the usability of the asthma ED measure. The work of these initiatives forms the basis of this toolkit, and is described in more detail in the next few sections.
Primary Care-Focused Approach
Most interventions that have been successful in improving asthma ED outcomes through provider-based activities have included intensive educational approaches or methods to develop improved systems of care within the primary care office setting. Harder et al. examined the effects of a one-year QI collaborative for primary care clinicians that focused on office systems strategies (e.g., asthma assessment, control and management, and patient education). Although there was no immediate effect noted, compared to control practices, the participating practices noted a substantial decrease of nearly 40 percent in asthma-related ED visit rates more than a year after the end of the collaborative (Harder, 2020). The development of a systematic primary care approach to asthma care can also improve asthma health care utilization. In a pragmatic, cluster randomized controlled trial, Yawn et al. demonstrated that the use of Asthma APGAR (Activities, Persistent, triGGers, Asthma medications, Response to therapy) tools improves rates of asthma control and reduces asthma-related ED and urgent care visits (Yawn, 2018).
Provider Continuing Medical Education Approach
Although traditional continuing medical education (CME) interventions have not been consistently effective in changing provider behavior; intensive, small group CME may make a difference. In a large national randomized control trial, a physician asthma education program, led by local opinion leaders, that focused on improving physician counseling skills and medication selection, along with resources for education, coding, and billing was effective in decreasing asthma ED use (Cabana, 2006). Timely feedback about patient symptoms may also help improve clinician management of asthma. For example, provider feedback about patient symptoms was shown to improve and change provider behavior and increase the frequency of asthma visits to adjust medications, but also reduce ED visits for asthma (Kattan, 2006).
Parental and School-based Education Approach
Parental understanding of asthma is an important component in helping children self-manage asthma. There have been mixed results in parent educational interventions (Nelson et al., 2011). Intensive parent education has also been shown to impact management and ED asthma visits (Chong, 2019), as well as asthma education and case management (Greineder, 1999). The use of home-based educational and environmental intervention delivered by lay health educators would improve asthma symptom control in inner-city children with asthma and has been shown to decrease ED visits (Bryant-Stephens, 2009). Finally, school-based interventions, “to help children improve management of their asthma by increasing knowledge, enhancing skills, or changing behaviour” have been associated with slightly decreased ED asthma visits (Harris, 2019).
PQMP Toolkit Approach: Primary Care Collaboratives
The PQMP asthma measure has the potential to improve asthma care, reduce ED utilization, and promote collaboration between health plans and primary care practices. Successful utilization of the measure will necessitate interpreting data from multiple sources and business entities. Because of this, there will be practical, ethical, and legal limitations relative to sharing data and how improvement efforts are implemented. While all of the approaches described above have merit, the PQMP grantees charged with testing how to use the pediatric ED use measure chose to focus on primary care, the intervention area with the most evidence of success. This toolkit outlines primary care-focused interventions using an intensive educational approach and methods to develop improved systems of care.
The IMPLEmenting MEasures NeTwork (IMPLEMENT) for Child Health initiative is the overall program that tested out the usability of the PQMP asthma ED measure by conducting QI initiatives in San Francisco, California (SF Collaborative) and in Burlington, Vermont (VT Collaborative). Both QI initiatives aimed to improve pediatric asthma care delivered in a primary care setting while examining the usability of the asthma measure. The strategies described in this toolkit reflect the learnings from the two QI initiatives. In the SF Collaborative, primary care practices participated in a 12-month learning collaborative. In the VT Collaborative, practices had participated in an earlier Vermont statewide asthma learning collaborative. Therefore, a more targeted approach was undertaken—performing a “deep dive” to examine factors that contributed to high ED rates.
Select for more information on the earlier Child Health Advances Measured in Practice (CHAMP) Learning Collaborative. Staff and faculty from the University of Vermont’s Vermont Child Health Improvement Program’s (VCHIP) provided the QI expertise for both initiatives.
Primary care learning collaboratives can be adapted based on the participants’ level of prior experience with QI activities. The support of practice leadership, clinicians, and operational staff are essential in successfully operating a primary care collaborative. Furthermore, partnerships with the clinicians from the practice, as well as commitment to looking into the complexity of the problems and processes involved, using QI methodologies, and communicating with and including members of the practice throughout the learning process are critical factors in any QI project’s success.
The next section of the toolkit describes a phased approach to implementing a learning collaborative in primary care aimed at reducing ED use among pediatric asthma patients based upon the experiences from the two initiatives with input from QI experts.
Quality Improvement with a Focus on Primary Care Delivery
Both the SF and VT Collaboratives used practice-level data to determine how and where to intervene using QI strategies based on the Institute for Health Improvement’s (IHI) Learning Collaborative model. Although the initiatives involved different strategies depending on the prior experience of the primary care practices with improving asthma care, all of the strategies were intended to contribute to a reduction in inappropriate ED use.
These collaborative initiatives can be sponsored by a managed care plan, health system large provider group, or Improvement Partnership as described in Shaw 2013, and are designed to support primary care practices focusing on ensuring provider adherence to NHLBI guidelines for managing pediatric asthma patients and implementing system-level changes to improve asthma care.
Practices are encouraged to assure they have a QI infrastructure that will promote rapid and sustainable improvement. Key components of a high-functioning QI team include clinical champions, leadership support, a quality coach and the ability to generate actionable data—including reporting. Additionally, a practice’s ability to be receptive to change and modify practices is essential to a learning organization. There are several tools that can help reinforce components of the QI team to promote success at the practice level, including the article entitled Modeling for Understanding Success in Quality (MUSIQ) (Kaplan, 2012).
Where to start
Primary care practices and the organizations supporting them with limited or no prior QI experience are encouraged to take the approach described below as Phase 1.
- The SF Collaborative provides an example of this approach. Adherence to the NHLBI guidelines, as determined through process measures, is a first step in ensuring that a primary care practice can best serve its pediatric asthma patients.
Primary care practices already experienced in implementing NHLBI guidelines and using QI strategies can take the approach described below as Phase 2.
- The VT Collaborative provides an example of working with primary care practices already adhering to NHLBI guidelines with prior experience in an asthma QI collaborative. These practices were ready to take a “deep dive” into their existing processes.
Phase 1—Learning Collaborative for NHLBI Guideline Adherence
For primary care practices with limited or no prior QI activity in improving asthma care, the learning collaborative should focus on ensuring adherence to NHLBI guidelines for pediatric asthma care.
The SF Collaborative focused on establishing consistent use of NHLBI guidelines among providers and ensuring key process measures were completed as part of every patient’s asthma care. Strategies included increasing asthma control assessment, developing an asthma action plan, performing spirometry and improving asthma education for patients and families. The learning collaborative follows the standard format as described by the IHI in the white paper titled, “The Breakthrough Series: IHI’s Collaborative Model for Achieving Breakthrough Improvement” (IHI, 2003).
Typical learning collaboratives include at least one face-to-face meeting, followed by monthly conference calls and are led by a group with experience in quality improvement. At the initial meeting, participants are educated on the Plan, Do, Study, Act (PDSA) cycles, and data is shared based on the metrics and measures chosen. The SF Collaborative was assisted by the QI faculty and staff from the VCHIP and the materials from the CHAMP Learning Collaborative were adapted for use in SF. For a more detailed description of the approach that was adapted, refer to the article entitled “A primary care learning collaborative to improve office systems and clinical management of pediatric asthma” (Weinberger, 2019) which includes the tools used during the collaborative. Primary care practices participating in the CHAMP Learning Collaborative improved clinical asthma management measures through improvement of office systems to support asthma care. The initiative included evaluating seven months of medical record review data for improvements on eight clinical asthma management measures and the use of pre and post office systems inventory self-assessments.
In the SF Collaborative, practices followed a similar process to those used in the CHAMP Learning Collaborative in Vermont, attending a one-day face-to-face learning session and monthly collaborative conference calls. A sample agenda is available (PDF, 163.5 KB). Prior to the learning session, practice participants completed the QI knowledge survey (PDF, 208 KB). It is important to assess the attendees’ knowledge and experience with QI and adapting the collaborative to meet the learners’ needs. In the VT Collaborative, practices were members of the CHAMP statewide QI network, thus the level of attendee knowledge was already known. However, in the SF Collaborative a survey was designed to assess the knowledge base of potential collaborative attendees related to QI. Conducting such an assessment in advance of holding a collaborative and developing the final agenda and materials using this knowledge will help ensure the collaborative work starts at the appropriate level to promote progress in improving asthma care.
Baseline data is typically collected by the practice (through chart review) to establish practice performance relative to the agreed upon collaborative measures. Asthma measures and corresponding goals were decided by the IMPLEMENT team prior to the start of the learning collaborative. Select for descriptions of the measures monitored by the SF Collaborative (PDF, 259 KB). The document used for sample baseline chart review can be accessed as a PDF (KB, 333.5 KB).
At the learning session, topics included basic principles of QI, education including NHLBI guidelines for asthma care, and practice-level baseline data presentation (PDF, 684 KB) . Ample time was allowed for practice-based teams to develop their first PDSA cycle of improvement. Following the learning session, practices submitted monthly data and participated in monthly collaborative calls where project-level data was presented as progress towards collaborative goals.
A key tool used in the CHAMP Learning Collaborative and adapted for use in the SF Collaborative is the Office Systems Inventory (OSI), a document that categorizes and lists strategies to help improve asthma care. Access the tool (PDF, 237 KB). The OSI lists the strategies that healthcare professionals and primary care practices can use to improve their office systems to promote optimal asthma treatment. Examples of specific strategies included on the OSI are assessing the child's asthma control at every visit using a validated tool, using an asthma action plan as a communication tool with the family, and integrating education into all points of care by including members of all health care disciplines.
The purpose of the OSI strategies document is to help practices identify areas where there are gaps in their systems or processes that they can focus on in their improvement efforts. Teams can go through this document together at the start of an improvement effort and document if each of the strategies is: not done, done inconsistently, done consistently, or consistently done based on best practice. At the completion of an improvement effort, the practice team can complete the strategies self-assessment again to identify systems changes and improvements made.
To further support using the learning collaborative approach as the first phase in utilizing the PQMP asthma measure, VCHIP examined if participation in the CHAMP Learning Collaborative was associated with a decrease in asthma-related ED utilization over time compared to controls. The findings described in “Statewide Asthma Learning Collaborative Participation and Asthma-related Emergency Department Use” reports that participation in the CHAMP Learning Collaborative was associated with a substantial decrease in asthma-related ED visits, compared to controls, more than a year after the end of the collaborative (Harder, 2020).
Phase 2—Deep Dive to Understand Pediatric ED Use
When primary care practices have successfully engaged in asthma QI activities, a health plan, accountable care organization (ACO), or health system may choose work with practices to more closely examine or take a “deep dive” into the reasons patients are using the ED for pediatric asthma care. This phase involves a retrospective review process in primary care to understand the ‘population’ of each primary care practice’s patients who go to the ED. This deep dive process requires an organizational commitment and investment of resources including assisting with the identification of practice patients with ED visits, conducting the retrospective chart reviews, and supporting the application of QI methods to identify areas for improvement and coaching in improvement efforts.
The following section provides examples of tools that an organization can use in implementing Phase 2.
Taking a deep dive to understand the reasons patients are using the ED for pediatric asthma care involves three main steps:
- Identify practice patients with ED visits.
- Use Practice Asthma Data Collection Tool to retrospectively examine asthmatics accessing the ED.
- Implement QI activities.
As an additional resource, the detailed strategies employed in the Vermont Learning Collaborative are summarized (PDF, 237 KB)
Deep Dive—Step 1. Identify practice patients with ED visits
Step 1 is designed to compile a complete and accurate identification of patients with asthma in each primary care practice and identify who has had an asthma-related ED visit in the last six to 12 months. While the list can be generated by a practice, a health plan, or a health care system (e.g., ACO), there are benefits and limitations of each scenario to consider. A practice-defined list provides the most comprehensive capture of patients. Health plan or ACO data is limited to the patients they insure or are accountable for, and thus may limit the generalizability of the chart review findings. Once the list of patients with asthma-related ED visits is compiled, the QI team should review the associated ED utilization data.
Although seemingly simple, a practice without an asthma registry may find it challenging to identify all their patients with asthma and then to determine if they have had an ED visit. Working with a health plan, ACO, or other organization with access to billing data for a specific population to provide the practice with a list of patients with ED visits could be beneficial but would be limited to the patients they insure.
Select to access a flow chart describing the process an entity can take to identify and monitor the pediatric asthma care provided to its members (PDF, 150 KB). Health plans are able to use the ICD-10 codes to define children with asthma and include them in the analysis. The codes are available to download as an Excel file (36, KB).
An example of a joint effort between a payer and a practice with an asthma registry to identify patients with an ED visit is described below:
A QI team, comprised of payer and practice staff, reviews data for children covered by the health plan. Additionally, the practice reviews the parameters of their asthma registry with the payer, including ICD-10 codes, medication groupers, and demographic data. While this measure is designed to be interpreted by the payer, interventions to improve process measures at the practice level must be agnostic of insurance coverage due to the potential for inequity. Because of this, practices should not be expected to provide process measures based on health plan coverage.
Deep Dive—Step 2. Use Practice Asthma Data Collection Tool to Retrospectively Examine Asthmatics Accessing the ED
Once asthmatics with one or more ED visit are identified, a retrospective chart review is conducted. The chart review involves a ‘look back’ from the date of the most recent ED visit and should include a range of ages from 3-21 years. In the VT Collaborative, 25 charts were reviewed, although that total number can vary depending upon the size of the practice and the number of asthmatics with ED visits. In smaller practices, this may cover close to a one-year period, while in larger practices, 25 charts may cover a shorter period. There is no prescribed number of charts, but the process should include sufficient numbers to capture gaps in care that could be identified as areas for improvement. Refer to the Practice Asthma Data Collection Form (PDF, 323 KB)
The chart review questions were developed and refined multiple times with broad input from clinicians and QI experts. Research Electronic Data Capture (REDCap), an online secure data collection tool that meets HIPAA compliance standards, housed the survey for the VT Collaborative. Sites wishing to import the Vermont survey directly into their own version of REDCap may download the REDCap survey tool as an Excel file (30 KB). Practices may opt to create a different mechanism for data capture and can use the questions in the file to inform their own survey development. The survey is broken into 10 areas, which capture the key themes of the NHLBI Expert Panel Report (EPR-3) guidelines: 1) patient demographics, 2) ED utilization, 3) prior healthcare utilization, 4) asthma severity and control, 5) medications, 6) spirometry, 7) asthma education and self-management, 8) tobacco use assessment, 9) allergies, and 10) other factors.
Once collected, the data are analyzed, and descriptive statistics (absolute counts and relative percentages) are produced. REDCap has the functionality for data analysis and a person familiar with REDCap should assist with this step.
The chart review data collected for the VT Collaborative included data from multiple insurers and analysis was conducted by an academic institution. Confidentiality was maintained and data was not shared beyond the practice. This approach can be replicated by health plans, ACOs, or health systems to monitor delivery of pediatric asthma care. They can work with clinicians and healthcare teams to collect and interpret the data, identify problems, and determine courses of action to drive improvement in patients’ health. The following example illustrates how one group of healthcare teams used this approach.
An example from the VT Collaborative using the chart audit tool is described below:
The QI team recognized that NHLBI guideline adherence alone would not address the root causes of why some children with asthma end up in the ED. To mitigate unnecessary ED visits, a system to collect information retrospectively from medical charts was developed, including information not typically captured in patient charts (e.g., information on social needs). Preferably the chart review is conducted by someone in the practice with a clinical background (MD, PA, NP, RN) because they are familiar with the practice and can participate in the review of the post-chart review data. In Vermont, two nurse practitioners conducted the chart review.
Deep Dive—Step 3. Review of key practice-wide process measure performance and initiation of QI activity
As noted, this deep dive process requires a skilled QI coach to assist practices with analysis of the chart review data and to help determine areas for improvement. Step 3 involves a highly iterative process and requires significant clinician engagement and training in QI. The QI coach should be familiar with QI methods and strategies and will choose the approach most appropriate for the practice staff and clinician(s) knowledge and skills and the available resources devoted to the improvement process.
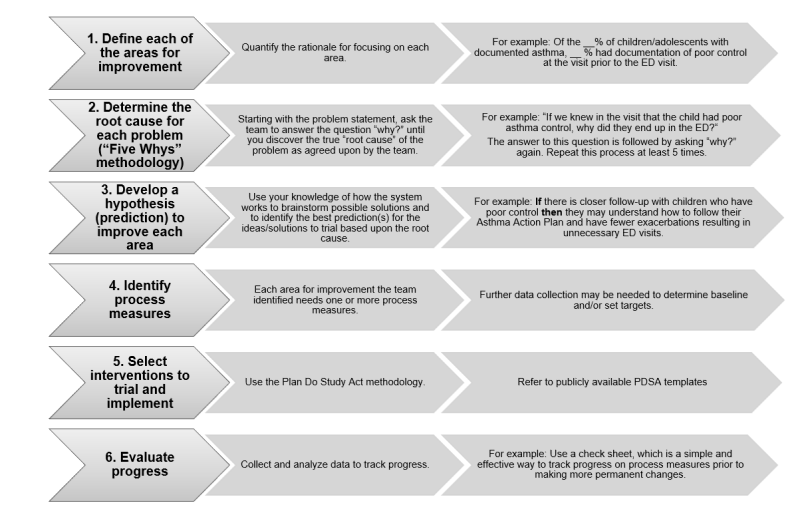
The following flow diagram depicts the typical steps required in ongoing QI work.
Flow Diagram of the Steps in the QI Problem-Solving Process
The iterative process used to achieve success in the VT Collaborative is described below as an illustrative example of Step 3:
Targeted coaching on use of data. The primary care clinical team received targeted coaching to increase the team’s fundamental knowledge, aptitude for developing impactful interventions, and practical skills. The QI coaches conducted learning sessions about interpreting the data and understanding the implications of strategies to improve office systems (e.g., workflows, resources, team approaches). During these sessions, clinicians developed theories and planned interventions. Between meetings, clinicians conducted observations of office systems. These observations were discussed at the quality team meetings and the team engaged in fruitful discussions about the nature of variation in any system. Differences in practice patterns between office personnel were identified as central to either wasteful or highly effective workflows. The improvement team integrated hypotheses, data, and office systems into meaningful process measures that they anticipated would lead to eventual improvement in the outcome measure (e.g., Increase percent of follow-up calls to provide asthma education and information to patients/families when the patient had documentation of poor asthma control at the visit).
Identifying opportunities for improvement. The team then sought to identify the most significant problems or improvement opportunities, to understand why they were occurring, and to address the opportunities for improvement. Using a flowchart to understand the processes in which the problems occur can be helpful, especially when the team includes members who have differing levels of knowledge about and experience with practice processes. Based upon their review and discussion of the results of the chart audit, the team identified four specific areas for improvement that, if addressed, could help to decrease potentially avoidable ED visits. The team assessed each of the four areas for improvement individually to gain a deeper understanding and to identify and understand the “root cause” of the factors that could lead to these ED visits.
Conducting a root cause analysis. The QI coach facilitated the root cause analysis and helped the team to further explore each of the four areas identified for improvement. The team was then able to identify specific process measures and select interventions to trial and implement in the practice setting. The root cause analysis was used working with the full healthcare team’s involvement so they could gain optimal understanding of “how” the system works using the “Five Whys” Root Cause Analysis process. The IHI describes this process and provides a PDF guide at http://www.ihi.org/resources/Pages/Tools/5-Whys-Finding-the-Root-Cause.aspx.
References
5 Whys: Finding the Root Cause. Boston: Institute for Healthcare Improvement. Retrieved from http://www.ihi.org/resources/Pages/Tools/5-Whys-Finding-the-Root-Cause.aspx.
Child Health Advances Measured in Practice (CHAMP). Vermont Child Health Improvement Program, University of Vermont. Last modified November 2019. Retrieved from http://www.med.uvm.edu/vchip/champ.
Allen ED, Montgomery T, Ayres G, Cooper J, Gillespie J, Gleeson, SP, Groner J, Hersey S, McGwire G, Rowe C, Snyder D, Stukus D, Stukus KS, Timan C, Wegener N, Brilli RJ. Quality Improvement-Driven Reduction in Countywide Medicaid Acute Asthma Health Care Utilization. Academic Pediatrics 2019 Mar;19(2):216-226. doi:10.1016/j.acap.2018.12.005.
The Breakthrough Series: IHI’s Collaborative Model for Achieving Breakthrough Improvement. IHI Innovation Series white paper. Boston: Institute for Healthcare Improvement; 2003. Retrieved from http://www.ihi.org/resources/Pages/IHIWhitePapers/TheBreakthroughSeriesIHIsCollaborativeModelforAchievingBreakthroughImprovement.aspx.
Bryant-Stephens T, Kurian C, Guo R, Zhao H. Impact of a household environmental intervention delivered by lay health workers on asthma symptom control in urban, disadvantaged children with asthma. Am J Public Health 2009;99 Suppl 3(Suppl 3):S657‐S665. doi:10.2105/AJPH.2009.165423Bottom of Form
Cabana MD, Slish KK, Evans D, et al. Impact of Physician Asthma Care Education on Patient Outcomes. Pediatrics 2006;117(6):2149-2157.
Chong YY, Mak YW, Leung SP, Lam SY, Loke AY. Acceptance and Commitment Therapy for Parental Management of Childhood Asthma: An RCT. Pediatrics 2019;143(2):e20181723. doi:10.1542/peds.2018-1723.
Greineder DK, Loane KC, Parks P. A randomized controlled trial of a pediatric asthma outreach program. J Allergy Clin Immunol 1999;103(3 Pt 1):436‐440. doi:10.1016/s0091-6749(99)70468-9
Harder VS, Shaw JS, McCulloch CE, Kill L, Robinson KJ, Shepard MT, Cabana MD, Bardach NS. Statewide Asthma Learning Collaborative Participation and Asthma-related Emergency Department Use. Pediatrics 2020. [in press]
Harris K, Kneale D, Lasserson TJ, McDonald VM, Grigg J, Thomas J. School-based Self-Management Interventions for Asthma in Children and Adolescents: A Mixed Methods Systematic Review. Cochrane Database of Systematic Reviews 2019 Jan 28;1(1):CD011651. doi: 10.1002/14651858.CD011651.pub2.
Kaplan HC, Provost LP, Froehle CM, & Margolis PA. (2012). The Model for Understanding Success in Quality (MUSIQ): building a theory of context in healthcare quality improvement. BMJ quality & safety 21(1), 13–20. https://doi.org/10.1136/bmjqs-2011-000010
Kattan M, Crain EF, Steinbach S, et al. A randomized clinical trial of clinician feedback to improve quality of care for inner-city children with asthma. Pediatrics 2006;117(6):e1095‐e1103. doi:10.1542/peds.2005-2160
National Asthma Education and Prevention Program Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma. U.S. Department of Health and Human Services, National Heart, Lung, and Blood Institute. 2007. Retrieved from https://www.nhlbi.nih.gov/sites/default/files/media/docs/EPR-3_Asthma_Full_Report_2007.pdf.
Nelson KA, Highstein GR, Garbutt J, et al. A randomized controlled trial of parental asthma coaching to improve outcomes among urban minority children. Arch Pediatr Adolesc Med 2011;165(6):520‐526. doi:10.1001/archpediatrics.2011.57
Resources: Institute for Healthcare Improvement (IHI). (2020). Retrieved July 13, 2020, from http://www.ihi.org/resources/Pages/default.aspx.
Shaw JS, Norlin C, Gillespie RJ, Weissman M, McGrath J. The national improvement partnership network: state-based partnerships that improve primary care quality. Academic pediatrics 2013; 13(6 Suppl):S84-94. PMID: 24268091
Weinberger SJ, Cowan KJ, Robinson KJ, Pellegrino CA, Frankowski BL, Chmielewski MV, Shaw JS, & Harder VS. (2019) A primary care learning collaborative to improve office systems and clinical management of pediatric asthma, Journal of Asthma DOI: 10.1080/02770903.2019.1702199
Yawn BP, Wollan PC, Rank MA, Bertram SL, Juhn Y, Pace W. Use of Asthma APGAR Tools in Primary Care Practices: A Cluster-Randomized Controlled Trial. Ann Fam Med 2018;16(2):100‐110. doi:10.1370/afm.2179



