On September 18, 2011, Connie Savor Price, MD made this presentation at the 2011 Annual AHRQ HAI Investigators Meeting. Select to access the  Microsoft PowerPoint version - 394.16 KB .
Microsoft PowerPoint version - 394.16 KB .
Slide 1
Improving the Measurement of Surgical Site Infection (SSI) Risk Stratification and Outcome Detection
Connie Savor Price, MD
2nd Annual AHRQ HAI Investigators Meeting
September 18, 2011
Bethesda, Maryland
Slide 2
Background
- SSIs are a substantial cause of morbidity and mortality
- Accounted for ~16 % of ~1.7 million HAIs and 8,205 of the 98,987 HAI associated deaths (mortality= 3%).
- Financial burden significant
- Hospital cost of ~$25,546 per SSI and ~$7 billion annually
- Feedback on surgeon-specific rates is considered to be the cornerstone for preventing these infections.
- Surgeons must believe rates are reliable
- Current surveillance methods are perceived as limited in risk adjustment and detection
Slide 3
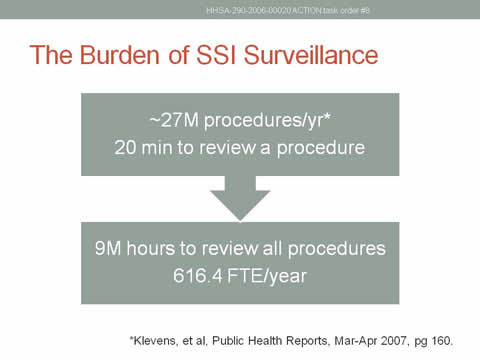
The Burden of SSI Surveillance
~27M procedures/yr*
20 min to review a procedure
Leads to:
9M hours to review all procedures
616.4 FTE/year
* Klevens, et al, Public Health Reports, Mar-Apr 2007, pg 160.
Slide 4
Aims
- Employ electronic detection algorithms to determine SSI rates for selected procedures* in 4 unique hospital settings
- Conduct focus groups to assess:
- Surgeons' acceptance of current risk stratification models and determine what risk factors surgeons deem important for future model development
- Adoption of electronic surveillance tool by Infection Prevention nurses
- Design and test methods to risk stratify on data elements available for electronic collection
* Coronary artery bypass graft, hernia repair, hip and knee arthroplasty
Slide 5
Images: Pictures of the 4 hospital settings involved in the study. Clockwise from top left: Denver Health, Intermountain Healthcare, Vail Valley Medical Center, and the Salt Lake City Veterans Administration.
Slide 6
Employ Electronic Detection Algorithms to Determine SSI Rates for Selected Procedures in 4 Unique Hospital Settings
Slide 7
Combining the Best of Both Worlds
- Human: smart, adaptable
PLUS - Machine: consistent, reliable, scalable
EQUALS - The best of both worlds: human-adjudication of electronically triaged cases
- Electronically eliminate most uncomplicated surgeries
- Utilize Infection Preventionist knowledge & experience in hard cases
- Highest sensitivity and negative predictive value desired
Slide 8

Methods
- Create Algorithm
- Literature review identified electronic data that are manifestations, but not risks of SSI to predict deep or organ-space SSI
- Train Algorithm
- Used randomly selected ½ of 2007-2009 VASQIP data for outcomes data
- Test Algorithm
- One-fold cross validation using other ½ of VASQIP data
- External validation at the 3 other systems
- "Portable" algorithms implemented and analyzed locally
- Data standardized to ensure interoperability
Slide 9
Results
Data Elements for Training Sets
- WBC count, WBC differential, erythrocyte sedimentation rate (ESR), c-reactive protein (CRP), microbiology results, and antimicrobial administration
- Fever
- Excluded as not available electronically at all sites
- Procalcitonin
- Excluded as this result is not widely available in the US
- Claims data
- Excluded as generally not available until well after an IP would be reviewing cases
Slide 10
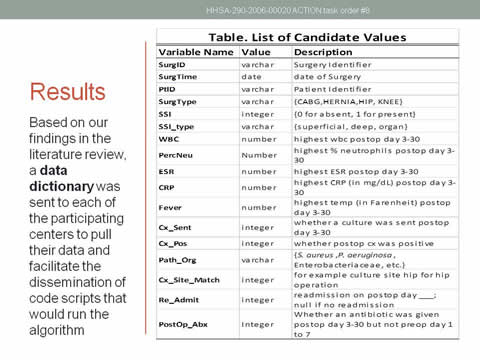
Results
Based on our findings in the literature review, a data dictionary was sent to each of the participating centers to pull their data and facilitate the dissemination of code scripts that would run the algorithm
A table showing example data names, values, and descriptions is included with this slide for illustrative purposes.
Slide 11
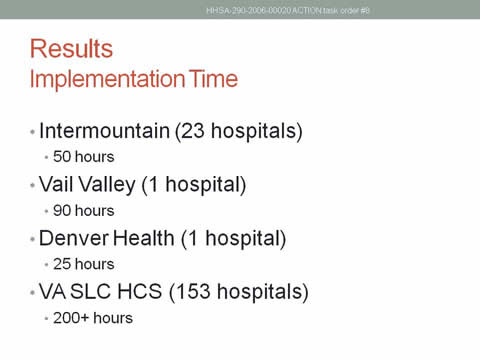
Results
Implementation Time
- Intermountain (23 hospitals)
- 50 hours
- Vail Valley (1 hospital)
- 90 hours
- Denver Health (1 hospital)
- 25 hours
- VA SLC HCS (153 hospitals)
- 200+ hours
Slide 12

Component Rules of the Classification Tree Algorithm
CABG:
All of the following:
Presence of a post-operative culture, and
Post-operative antibiotics were given, and
Maximum post-operative leukocyte count is not less than 11.85
Herniorrhaphy:
Either of the following:
Presence of a post-operative culture and
Maximum post-operative leukocyte count is not less than 7.78
Absence of a post-operative culture and one of the following criteria:
Post-operative antibiotics given and any post-operative leukocyte count test drawn
Post-operative antibiotics not given, but the patient had a post-operative admission
Total Knee Arthroplasty:
Either of the following:
Presence of a post-operative culture, or
Presence of a c-reactive protein and the maximum post-operative leukocyte count is not less than 9.45
Total Hip Arthroplasty:
All of the following:
Presence of a post-operative culture, and
Post-operative antibiotics were given, and
Maximum post-operative leukocyte count is not less than 7.55
Abbreviations: CABG, coronary artery bypass grafting
Slide 13
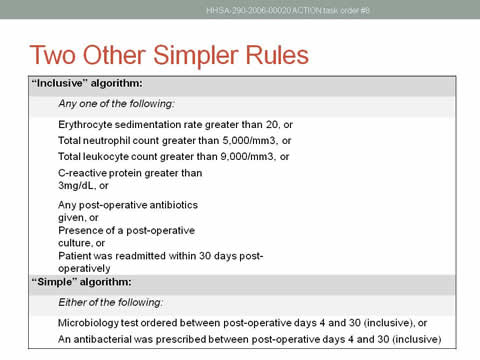
Two Other Simpler Rules
"Inclusive" algorithm:
Any one of the following:
Erythrocyte sedimentation rate greater than 20, or
Total neutrophil count greater than 5,000/mm3, or
Total leukocyte count greater than 9,000/mm3, or
C-reactive protein greater than 3mg/dL, or
Any post-operative antibiotics given, or
Presence of a post-operative culture, or
Patient was readmitted within 30 days post-operatively
"Simple" algorithm:
Either of the following:
Microbiology test ordered between post-operative days 4 and 30 (inclusive), or
An antibacterial was prescribed between post-operative days 4 and 30 (inclusive)
Slide 14
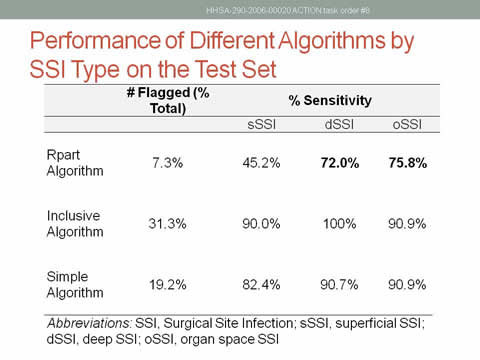
Performance of Different Algorithms by SSI Type on the Test Set
| # Flagged (% Total) |
% Sensitivity | |||
|---|---|---|---|---|
| sSSI | dSSI | oSSI | ||
| Rpart Algorithm | 7.3% | 45.2% | 72.0% | 75.8% |
| Inclusive Algorithm | 31.3% | 90.0% | 100% | 90.9% |
| Simple Algorithm | 19.2% | 82.4% | 90.7% | 90.9% |
Abbreviations: SSI, Surgical Site Infection; sSSI, superficial SSI; dSSI, deep SSI; oSSI, organ space SSI
Slide 15
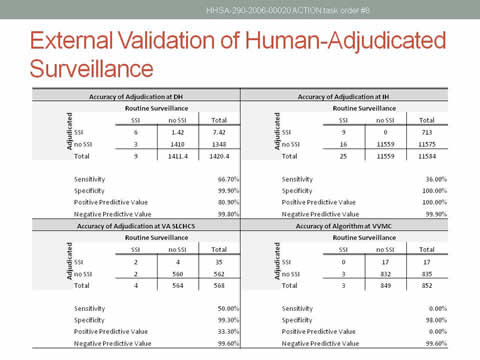
External Validation of Human-Adjudicated Surveillance
Table illustrating the accuracy of adjudication at each hospital site, as described in detail in the final report narrative.
Slide 16
Post-Mortem
- All false negatives were reviewed
- Some cases were arguably not deep or organ-space SSI
- Some cases were flagged as SSI outside of 30-day window
- The most commonly cited source of information that could have prevented a false negative was in clinical notes.
Slide 17
Lessons Learned
- Common electronic data markers of infection are not informative enough.
- Variation in practice can alter the performance of algorithms between facilities.
- Over-fitting is likely under-recognized in the literature because of small numbers of facilities.
- Even though the VA system is large, individual hospital practices and data storage are more like each other than community facilities
- Post-discharge surveillance is still an issue.
Slide 18
Future Directions
- Natural Language Processing may be necessary to generate more informative data.
- Training algorithms should include a large number of diverse hospitals.
- Algorithms may be better used to estimate the likelihood of SSI for triage as opposed to a complete rule-out determination (likelihood score for validation of publicly reported data)?
- Denver Health had modified the algorithm to tailor the surveillance to our institution for a variety of surgeries; sensitivity 100 percent, with a 60 percent decrease in chart review time.
Slide 19
Conduct Focus Groups
Slide 20
Methods
- Surgeon: 6 surgeons with research interests in SSI, representing multiple health system types (4 academic, 2 private, 2 safety net, 1 VA) and surgical specialties (5 general, 2 trauma/critical care, 1 surgical oncology).
- Infection Prevention (Denver): 5 Infection Preventionists from 4 private hospitals and 1 public hospital. Average years as an IP = 10.
Slide 21
Results and Implications
- Surgeons feel that current risk adjustment models are inadequate
- Too simplistic.
- IPs receptive to concept of electronic triage with human adjudication
- Needs to be adaptable to variety of systems, low/no cost.
- More refined models may improve acceptance of data and benchmarks.
- Further research to identify evidence-based risk factors for SSI is needed.
- Risk Factors were suggested by surgeons for future models.
Slide 22
Design and Test Methods to Risk Stratify on Data Elements Available for Electronic Collection
Slide 23
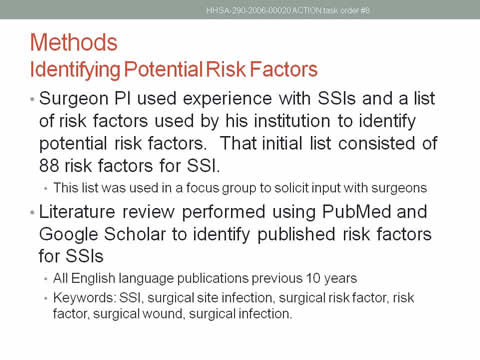
Methods.
Identifying Potential Risk Factors:
- Surgeon PI used experience with SSIs and a list of risk factors used by his institution to identify potential risk factors. That initial list consisted of 88 risk factors for SSI.
- This list was used in a focus group to solicit input with surgeons.
- Literature review was performed using PubMed and Google Scholar to identify published risk factors for SSIs
- All English language publications [in] previous 10 years
- Keywords: SSI, surgical site infection, surgical risk factor, risk factor, surgical wound, surgical infection.
Slide 24

Methods
Identifying Electronic Availability
- Master List of potential risk factors sent to each of the four study sites.
- Each potential risk factor clinically reviewed and categorized as modifiable or nonmodifiable.
- Each site determined if they had electronic access to the individual risk factors.
- Union set of 34 electronically available potential risk factors common to all sites identified and defined.
Slide 25
Methods.
Identifying Potential Risks and Outcomes in Procedures of Interest
- Each site collected potential risk factor variables for adults who had undergone CABG, herniorrhaphies, hip arthroplasty and knee arthroplasty.
- SSI* outcome noted for each patient.
*CDC/NHSN methodology
Slide 26
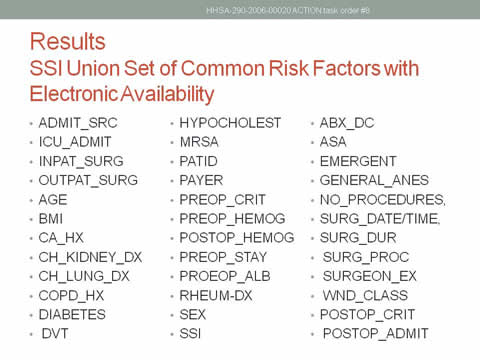
Results
SSI Union Set of Common Risk Factors with Electronic Availability
List of common factors available for collection as existing electronic data from all sites, as described in the final report narrative.
Slide 27
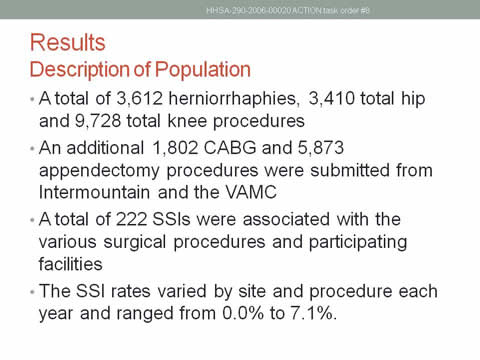
Results
Description of Population
- A total of 3,612 herniorrhaphies, 3,410 total hip and 9,728 total knee procedures.
- An additional 1,802 CABG and 5,873 appendectomy procedures were submitted from Intermountain and the VAMC.
- A total of 222 SSIs were associated with the various surgical procedures and participating facilities.
- The SSI rates varied by site and procedure each year and ranged from 0.0% to 7.1%.
Slide 28
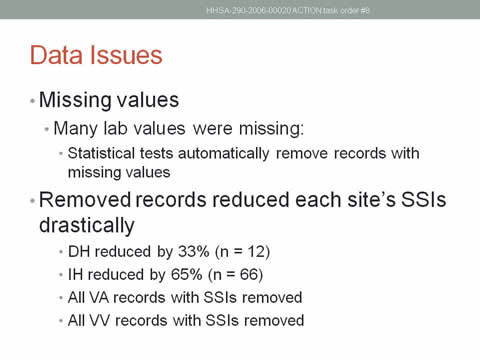
Data Issues
- Missing values:
- Many lab values were missing.
- Statistical tests automatically remove records with missing values.
- Many lab values were missing.
- Removed records reduced each site's SSIs drastically:
- DH reduced by 33% (n = 12)
- IH reduced by 65% (n = 66)
- All VA records with SSIs removed
- All VV records with SSIs removed.
Slide 29
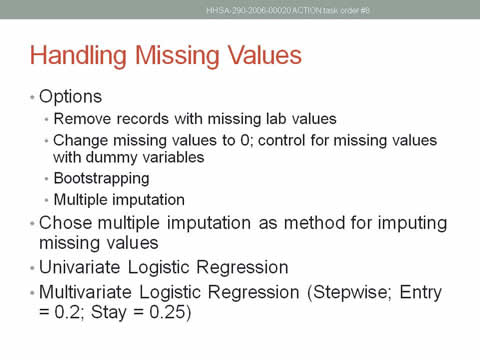
Handling Missing Values
- Options:
- Remove records with missing lab values
- Change missing values to 0; control for missing values with dummy variables
- Bootstrapping
- Multiple imputation.
- Chose multiple imputation as method for imputing missing values.
- Univariate Logistic Regression
- Multivariate Logistic Regression (Stepwise; Entry = 0.2; Stay = 0.25)
Slide 30
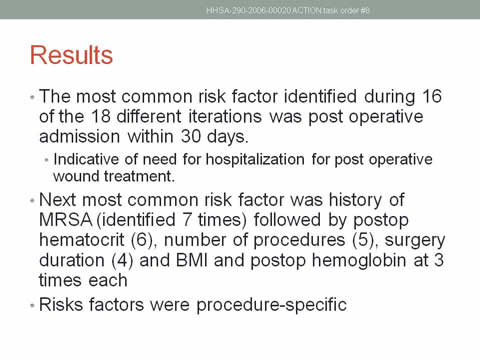
Results
- The most common risk factor identified during 16 of the 18 different iterations was postoperative admission within 30 days.
- Indicative of need for hospitalization for postoperative wound treatment.
- Next most common risk factor was history of MRSA (identified 7 times) followed by postop hematocrit (6 times), number of procedures (5 times), surgery duration (4 times), and BMI and postop hemoglobin (3 times each).
- Risk factors were procedure-specific.
Slide 31
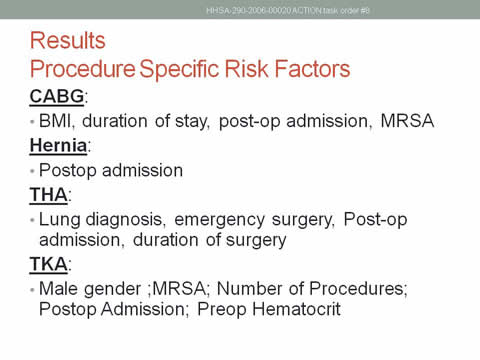
Results
Procedure Specific Risk Factors
CABG:
- BMI, duration of stay, postop admission, MRSA.
Hernia:
- Postop admission.
THA:
- Lung diagnosis, emergency surgery, Postop admission, duration of surgery.
TKA:
- Male gender; MRSA; Number of Procedures; Postop Admission; Preop Hematocrit.
Slide 32
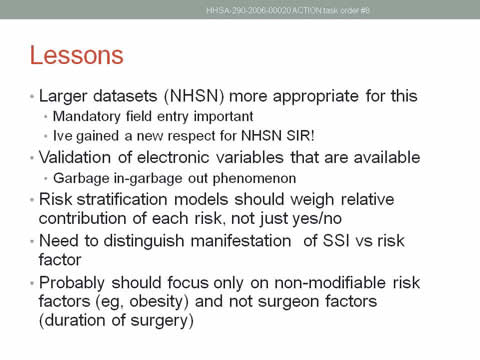
Lessons
- Larger datasets (NHSN) more appropriate for this
- Mandatory field entry important.
- New respect gained for NHSN SIR!
- Validation of electronic variables that are available.
- Garbage in–garbage out phenomenon.
- Risk stratification models should weigh relative contribution of each risk, not just yes/no.
- Need to distinguish manifestation of SSI vs risk factor.
- Probably should focus only on nonmodifiable risk factors (eg, obesity) and not surgeon factors (duration of surgery).
Slide 33
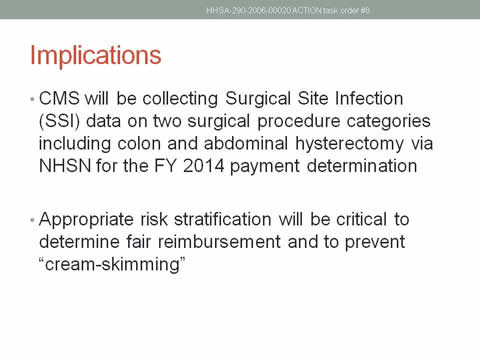
Implications
- CMS will be collecting Surgical Site Infection (SSI) data on two surgical procedure categories including colon and abdominal hysterectomy via NHSN for the FY 2014 payment determination.
- Appropriate risk stratification will be critical to determine fair reimbursement and to prevent “cream-skimming.”
Slide 34

Acknowledgements
Denver Health:
- Susan Moore, Connie Price, Walt Biffl, Josh Durfee
Salt Lake VA:
- Mike Rubin, Makoto Jones, Matt Samore
Intermountain:
- Lucy Savitz, Jason Scott, Scott Evans, Jef Huntington, Pat Nechodom
Vail Valley:
- Heather Gilmartin
CDC:
- Sandra Berrios-Torres, Jonathan Edwards, Teresa Horan
AHRQ:
- Kendall Hall
Slide 35
Extra Slides
Slide 36
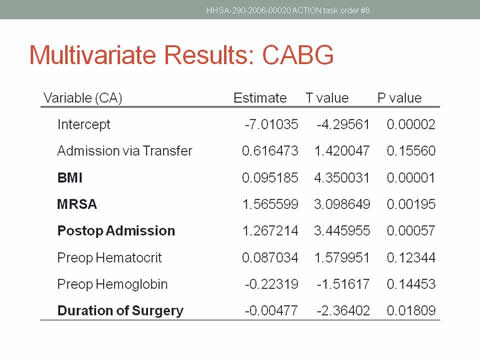
Multivariate results: CABG
| Variable (CA) | Estimate | T value | P value |
|---|---|---|---|
| Intercept | -7.01035 | -4.29561 | 0.00002 |
| Admission via Transfer | 0.616473 | 1.420047 | 0.15560 |
| BMI | 0.095185 | 4.350031 | 0.00001 |
| MRSA | 1.565599 | 3.098649 | 0.00195 |
| Postop Admission | 1.267214 | 3.445955 | 0.00057 |
| Preop Hematocrit | 0.087034 | 1.579951 | 0.12344 |
| Preop Hemoglobin | -0.22319 | -1.51617 | 0.14453 |
| Duration of Surgery | -0.00477 | -2.36402 | 0.01809 |
Slide 37
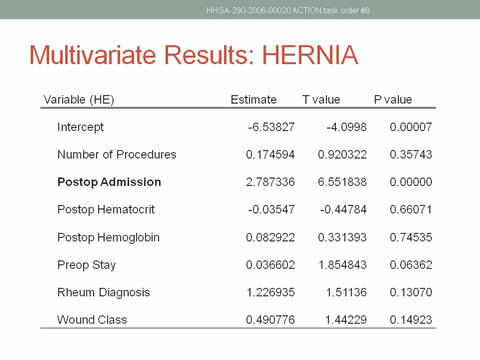
Multivariate Results: HERNIA
| Variable (HE) | Estimate | T value | P value |
|---|---|---|---|
| Intercept | -6.53827 | -4.0998 | 0.00007 |
| Number of Procedures | 0.174594 | 0.920322 | 0.35743 |
| Postop Admission | 2.787336 | 6.551838 | 0.00000 |
| Postop Hematocrit | -0.03547 | -0.44784 | 0.66071 |
| Postop Hemoglobin | 0.082922 | 0.331393 | 0.74535 |
| Preop Stay | 0.036602 | 1.854843 | 0.06362 |
| Rheum Diagnosis | 1.226935 | 1.51136 | 0.13070 |
| Wound Class | 0.490776 | 1.44229 | 0.14923 |
Slide 38
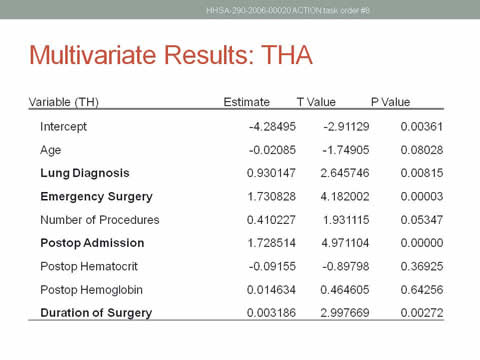
Multivariate Results: THA
| Variable (TH) | Estimate | T Value | P Value |
|---|---|---|---|
| Intercept | -4.28495 | -2.91129 | 0.00361 |
| Age | -0.02085 | -1.74905 | 0.08028 |
| Lung Diagnosis | 0.930147 | 2.645746 | 0.00815 |
| Emergency Surgery | 1.730828 | 4.182002 | 0.00003 |
| Number of Procedures | 0.410227 | 1.931115 | 1.931115 |
| Postop admission | 1.728514 | 4.971104 | 0.00000 |
| Postop Hematocrit | -0.09155 | -0.89798 | 0.36925 |
| Postop Hemoglobin | 0.014634 | 0.464605 | 0.64256 |
| Duration of Surgery | 0.003186 | 2.997669 | 0.00272 |
Slide 39
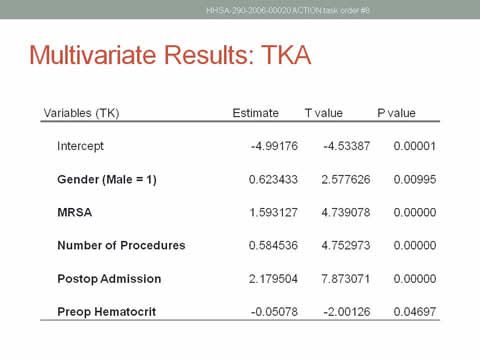
Multivariate Results: TKA
| Variables (TK) | Estimate | T value | P value |
|---|---|---|---|
| Intercept | -4.99176 | -4.53387 | 0.00001 |
| Gender (Male = 1) | 0.623433 | 2.577626 | 0.00995 |
| MRSA | 1.593127 | 4.739078 | 0.00000 |
| Number of Procedures | 0.584536 | 4.752973 | 0.00000 |
| Postop Admission | 2.179504 | 7.873071 | 0.00000 |
| Preop Hematocrit | -0.05078 | -2.00126 | 0.04697 |
Slide 40
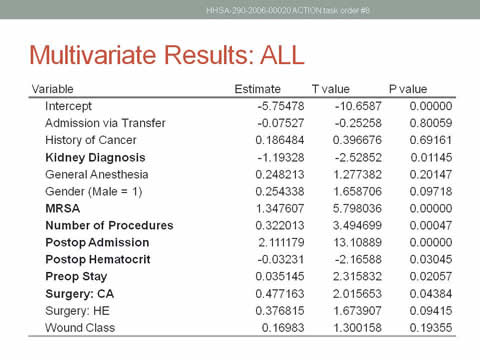
| Variable | Estimate | T value | P value |
|---|---|---|---|
| Intercept | -5.75478 | -10.6587 | 0.00000 |
| Admission via Transfer | -0.07527 | -0.25258 | -0.25258 |
| History of Cancer | 0.186484 | 0.396676 | 0.69161 |
| Kidney Diagnosis | -1.19328 | -2.52852 | 0.01145 |
| General Anesthesia | 0.248213 | 1.277382 | 0.20147 |
| Gender (Male = 1) | 0.254338 | 1.658706 | 0.09718 |
| MRSA | 1.347607 | 5.798036 | 0.00000 |
| Number of Procedures | 0.322013 | 3.494699 | 0.00047 |
| Postop Admission | 2.111179 | 13.10889 | 0.00000 |
| Postop Hematocrit | -0.03231 | -2.16588 | 0.03045 |
| Preop Stay | 0.035145 | 2.315832 | 0.02057 |
| Surgery: CA | 0.477163 | 2.015653 | 0.04384 |
| Surgery: HE | 0.376815 | 1.673907 | 0.09415 |
| Wound Class | 0.16983 | 1.300158 | 0.19355 |
Slide 41
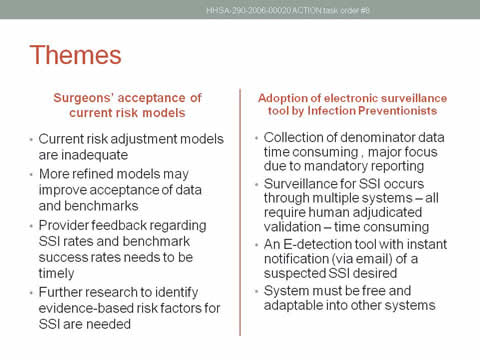
Themes
Surgeons' acceptance of current risk models
- Current risk adjustment models are inadequate
- More refined models may improve acceptance of data and benchmarks
- Provider feedback regarding SSI rates and benchmark success rates needs to be timely
- Further research to identify evidence-based risk factors for SSI are needed
Adoption of electronic surveillance tool by Infection Preventionists
- Collection of denominator data time consuming , major focus due to mandatory reporting
- Surveillance for SSI occurs through multiple systems - all require human adjudicated validation - time consuming
- An E-detection tool with instant notification (via email) of a suspected SSI desired
- System must be free and adaptable into other systems



