Workforce Capacity
- Ensuring well-coordinated, high-quality health care requires the establishment of a supportive health system infrastructure (IOM, 2010).
- Key elements include:
- Well-distributed capable and qualified workforce.
- Organizational capacity to support culturally competent services and ongoing improvement efforts.
- Health care safety net for hospital admissions of vulnerable populations.
Infrastructure Measures
- Physicians and surgeons per 100,000 population, by race and ethnicity.
- Primary care medical residents per 100,000 population, by sex and ethnicity.
- Characteristics of HRSA-supported health center population versus U.S. population.
- Distribution of trauma center utilization (Level I and II) for severe injuries in the United States, by age and geographic location.
- Medicaid and uninsured discharges in U.S. short-term acute hospitals, by facility characteristics.
Rate of Physicians and Surgeons
Physicians and surgeons per 100,000 population, by race and ethnicity, 2006-2013

Left Chart:
| Year | AI/AN | Asian | Black | White |
|---|---|---|---|---|
| 2006 | 79.9 | 1228.3 | 113.3 | 287.2 |
| 2007 | 96.1 | 1205.4 | 118.4 | 293.7 |
| 2008 | 1163.2 | 121 | 299.2 | |
| 2009 | 60.3 | 1153.5 | 113.9 | 290.6 |
| 2010 | 82.7 | 1155.2 | 115.2 | 289.9 |
| 2011 | 72.6 | 1200.8 | 125.6 | 296.6 |
| 2012 | 68.1 | 1123.2 | 120.6 | 298.6 |
| 2013 | 1212.5 | 130.3 | 297.5 |
Right Chart:
| Year | White | Black | Hispanic |
|---|---|---|---|
| 2006 | 301.6 | 113 | 112.8 |
| 2007 | 312 | 118.5 | 101.4 |
| 2008 | 322.9 | 122.4 | 112 |
| 2009 | 313.3 | 115.8 | 108.7 |
| 2010 | 317.3 | 114.2 | 104.8 |
| 2011 | 325.7 | 127.8 | 101.3 |
| 2012 | 325.8 | 120.7 | 113.9 |
| 2013 | 325.7 | 130.3 | 115.5 |
Key: AI/AN = American Indian or Alaska Native.
Source: U.S. Census Bureau, American Community Survey, 2006-2013.
Note: The 2008 and 2013 data for AI/ANs did not meet the criteria for statistical reliability, data quality, or confidentiality. White and Black are non-Hispanic. Hispanic includes all races. The rate of physicians is calculated by dividing the number of reported physicians from the American Community Survey by the U.S. population sample.
- Importance:
- Diversity in the composition of the health care workforce is important because it affects outcomes, quality, safety, and satisfaction. Racial and ethnic concordance in health care provider-patient relationships has been shown to improve care. Race-concordant patient-provider relationships, as opposed to race-discordant, have been found to result in longer medical visits with higher ratings of positive affect, shared decisionmaking, and satisfaction (Schoenthaler, et al., 2012).
- Additional research has found that health care providers from groups underrepresented in the health professions are more likely to serve minority and economically disadvantaged patients. It has also been found that Black and Hispanic physicians practice in areas with larger Black and Hispanic populations than other physicians (Brown, et al., 2009) and that Black and Hispanic Americans were likely to seek race- concordant physicians due to several factors, including language accessibility (Saha, et. al., 2000).
- Further studies have also shown patient trust with providers may influence clinical outcomes and medication adherence regardless of patient–physician racial/ethnic composition.
- Groups With Disparities:
- From 2006 to 2013, the rate of physicians per 100,000 population was higher for Asians than for Whites, Blacks, and American Indians and Alaska Natives (through 2012).
- From 2006 to 2013, the rate of physicians per 100,000 population was higher for non-Hispanic Whites than for non-Hispanic Blacks. The rate of physicians per 100,000 population was lower for Hispanics from 2007 to 2013.
Rate of Primary Care Medical Residents
Primary care medical residents per 100,000 population, by sex and race/ethnicity, 2013-2014
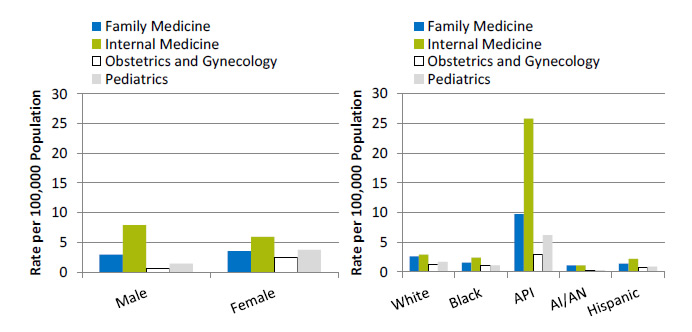
Left Chart:
| Sex | Family Medicine | Internal Medicine | Obstetrics and Gynecology | Pediatrics |
|---|---|---|---|---|
| Male | 2.9 | 7.9 | 0.6 | 1.4 |
| Female | 3.5 | 5.9 | 2.5 | 3.7 |
Right Chart:
| Race/Ethnicity | Family Medicine | Internal Medicine | Obstetrics and Gynecology | Pediatrics |
|---|---|---|---|---|
| White | 2.6 | 2.9 | 1.3 | 1.7 |
| Black | 1.6 | 2.4 | 1.1 | 1.1 |
| API | 9.7 | 25.8 | 2.9 | 6.2 |
| AI/AN | 1.1 | 1.1 | 0.3 | 0.3 |
| Hispanic | 1.4 | 2.2 | 0.7 | 0.9 |
Key: AI/AN = American Indian or Alaska Native; API = Asian or Pacific Islander.
Source: Accreditation Council for Graduate Medical Education, Data Resource Book, Academic Year 2013-2014. http://www.acgme.org/acgmeweb/tabid/259/Publications/GraduateMedicalEducationDataResourceBook.aspx.
Note: White, Black, API, and AI/AN are non-Hispanic. Hispanic includes all races. Rates are based on American Community Survey 1-year population estimates for 2013.
- Importance:
- Primary care providers and patients who have established clear communication and trusting relationships can yield better outcomes for patients; however, not all providers and patients can establish these relationships. Increased racial and ethnic diversity among primary care medical residents may lend itself to a provider workforce with strong cultural competency.
- Groups With Disparities:
- In 2013-2014, the rate of primary care medical residents was higher for females than for males in family medicine, obstetrics and gynecology, and pediatrics. The rate for males was higher than for females in internal medicine.
- In 2013-2014, the rate of primary care medical residents was higher for Asians and Pacific Islanders than for all other racial/ethnic groups, with the highest rate in internal medicine.
- In 2013-2014, American Indian and Alaska Native medical residents had the smallest rate of representation across all medical specialties.
Patient Characteristics of HRSA Health Center Population
Patient characteristics of HRSA-supported health center population versus U.S. population, 2014
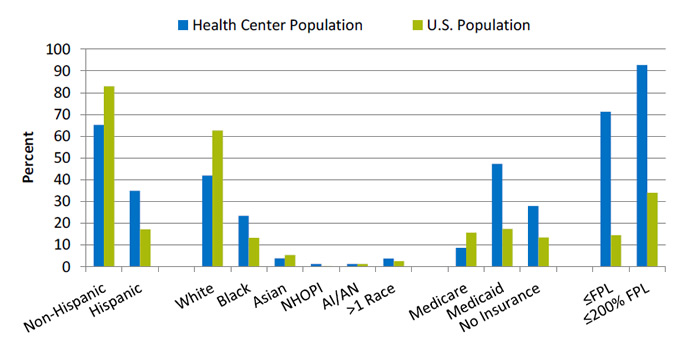
| Patient Characteristics | Health Center Population | U.S. Population |
|---|---|---|
| Non-Hispanic | 65.2 | 82.9 |
| Hispanic | 34.9 | 17.1 |
| White | 41.9 | 62.6 |
| Black | 23.4 | 13.2 |
| Asian | 3.8 | 5.3 |
| NHOPI | 1.2 | 0.2 |
| AI/AN | 1.3 | 1.2 |
| >1 Race | 3.7 | 2.4 |
| Medicare | 8.6 | 15.6 |
| Medicaid | 47.3 | 17.3 |
| No Insurance | 27.9 | 13.4 |
| <FPL | 71.2 | 14.5 |
| <200% FPL | 92.8 | 33.9 |
Key: AI/AN = American Indian or Alaska Native; NHOPI = Native Hawaiian or Other Pacific Islander; FPL = Federal poverty level.
Source: Health Resources and Services Administration, Bureau of Primary Health Care, Uniform Data System, 2014. http://bphc.hrsa.gov/uds/datasnapshot.aspx.
Note: Racial groups include Hispanics and non-Hispanics. Health center population includes 1,202 program grantees data only.
- Importance: Patients who receive health care in health centers may experience greater disparities in care compared with the general U.S. population.
- Population Differences:
- In 2014, slightly more than one-third (34.9%) of the health center population was Hispanic, which was twice as much as the percentage in the U.S. population (17.1%). Nearly one-quarter (23.4%) of the health center population was Black, almost twice as much as the percentage in the U.S. population (13.2%).
- The health center population also had higher percentages of uninsurance (27.9%) and Medicaid enrollment (47.3%) than the U.S. population (13.4% and 17.3%, respectively).
- In 2014, 71.2% of the health center population was at or below the Federal poverty level compared with 14.5% of the U.S. population.
Trauma Center Utilization for Severe Injuries
- Trauma care systems were developed to provide complex medical care to injured patients using a network of care facilities.
- Trauma systems are composed of levels ranging from level I to III centers, with level I denoting the most clinically sophisticated hospital.
- The hospital with the highest level is designated as the lead hospital in a trauma care system.
- Trauma center levels are:
- Level I: Required to have a specific number of surgeons and anesthesiologists on duty at all times, as well as education, prevention, and outreach programs. The 24-hour coverage of surgery in level I facilities also provides trauma patients with many surgical specialties, including neurosurgery, as well as radiology, internal medicine, and critical care.
- Level II: Provide initial definitive trauma care regardless of the severity of the injury. When a level II center cannot provide the required care, the patient may be triaged to a Level I center.
- Level III: Typically considered community or rural-based hospitals that provide prompt assessment, resuscitation, stabilization, emergency operations, and treatment. Level III facilities may transfer patients to hospitals with additional resources.
Distribution of trauma center utilization (level I and II) for severe injuries in the United States, by age, 2010-2013
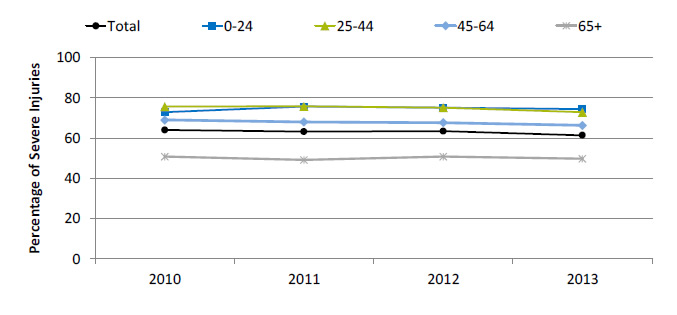
| Age | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|
| Total | 64.0 | 63.2 | 63.4 | 61.4 |
| 0-24 | 72.9 | 75.7 | 75.1 | 74.4 |
| 25-44 | 75.7 | 75.8 | 75.2 | 72.9 |
| 45-64 | 69.0 | 68.0 | 67.6 | 66.3 |
| 65+ | 50.8 | 49.1 | 50.8 | 49.7 |
Source: Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project, Nationwide Emergency Department Sample, 2010-2013.
- Importance: Well-coordinated and timely treatment for trauma patients can prevent needless injury to those who have suffered from an accident or other life-threating condition. Trauma centers in the United States provide care for both pediatric and adult populations. People the age of 45 years use trauma center services at a higher rate.
- Trends: From 2010 to 2013, the percentage of people who used trauma centers declined overall and among people ages 25-44 and 45-64.
- Groups With Disparities: From 2010 to 2013, people age 65 and over were less likely to use level I and II trauma centers than people under age 65.
Trauma Center Utilization, by Geographic Location
Distribution of trauma center utilization (Level I and II) for severe injuries in the United States, by geographic location, 2010-2013
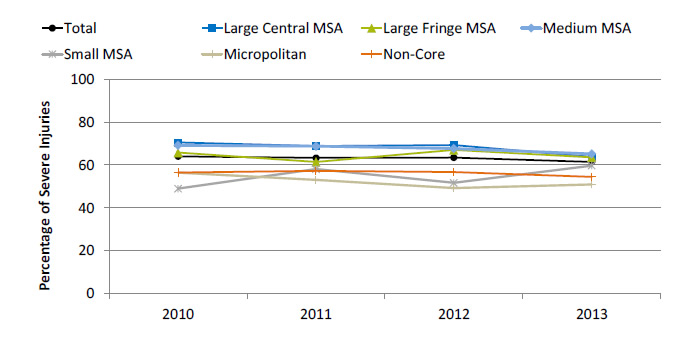
| Geographic Location | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|
| Total | 64.0 | 63.2 | 63.4 | 61.4 |
| Large Central MSA | 70.5 | 68.8 | 69.2 | 63.8 |
| Large Fringe MSA | 65.7 | 61.4 | 67.0 | 63.5 |
| Medium MSA | 69.1 | 68.7 | 67.6 | 65.2 |
| Small MSA | 48.9 | 58.0 | 51.6 | 59.6 |
| Micropolitan | 56.3 | 53.0 | 49.2 | 50.9 |
| Non-Core | 56.4 | 57.3 | 56.6 | 54.4 |
Key: MSA = metropolitan statistical area.
Source: Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project, Nationwide Emergency Department Sample, 2010-2013.
- Importance: In 2013, patients with intracranial injuries represented 53.6% of trauma center visits. Triaging patients to level I and II trauma centers with intracranial or other injuries is driven by many variables, including geographic proximity of the trauma center. Therefore, residents of rural areas may have difficulty gaining access to care in trauma centers.
- Trends: From 2010 to 2013, the percentage of people who used trauma centers declined among residents of large central metropolitan areas, medium metropolitan areas, and micropolitan areas.
- Groups With Disparities: In 2013, 63.8% of residents from a large central metropolitan area were treated in a level I or II trauma center compared with 50.9% of residents from a micropolitan area.
Medicaid and Uninsured Hospital Discharges
Rate of Medicaid and uninsured discharges in U.S. short-term acute hospitals, by facility characteristics, 2012-2013
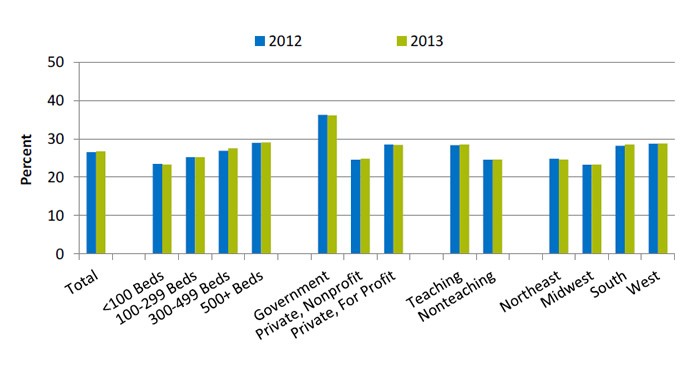
| Facility Characteristics | 2012 | 2013 |
|---|---|---|
| Total | 26.5 | 26.7 |
| <100 Beds | 23.4 | 23.3 |
| 100-299 Beds | 25.2 | 25.2 |
| 300-499 Beds | 26.9 | 27.5 |
| 500+ Beds | 28.9 | 29 |
| Government | 36.2 | 36 |
| Private, Nonprofit | 24.5 | 24.8 |
| Private, For Profit | 28.5 | 28.4 |
| Teaching | 28.3 | 28.5 |
| Nonteaching | 24.5 | 24.6 |
| Northeast | 24.8 | 24.6 |
| Midwest | 23.2 | 23.3 |
| South | 28.2 | 28.5 |
| West | 28.7 | 28.8 |
Source: Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project, HCUPnet, 2013.
Note: Government refers to hospitals that are operated by Federal, State, county, city, or hospital district governments.
- Importance: Some hospitals contribute to the safety net and provide care for more Medicaid and uninsured patients than others.
- Trends:
- There were no statistically significant changes in Medicaid and uninsured patient discharges from 2012 to 2013.
- Differences Between Types of Hospitals:
- In 2013, compared with hospitals with 500 or more beds (29.0%), hospitals with bed sizes under 300 (23.3% for <100 beds and 25.2% for 100-299 beds) had a smaller percentage of Medicaid or uninsured patients.
- In 2013, 28.4% of patients in private, for-profit hospitals had Medicaid or were uninsured, compared with 36.0% in government hospitals.
- Also in 2013, teaching hospitals (28.5%) had a larger percentage of Medicaid or uninsured patients compared with nonteaching hospitals (24.6%).
- In 2013, hospitals in the West and in the South had a greater percentage of Medicaid and uninsured patients (28.8% and 28.5%, respectively), while hospitals in the Midwest had the lowest percentage of these patients (23.3%).



