- Poor communication between providers and between providers and patients, within and across care settings, has been identified as a source of medication error.
- Improving communication is a key aspect of decreasing medication errors and improving patient safety (Kitson, et al., 2013).
- Disparities in access to health information, services, and technology can result in:
- Less use of preventive services.
- Poorer chronic disease management.
- Higher hospitalization rates.
- Poorer reported health status (Berkman, et al., 2004).
- Patients need to understand their medication (indications, administration, adverse effects) to safely and effectively use it. But important medication information is given to patients in a haphazard way (Persell, 2013).
Integration of medication information measures include:
- People under age 65 with a usual source of care whose health provider usually asks about prescription medications and treatments from other doctors.
- Hospitals with electronic exchange of patient medication history with hospitals outside their system.
- Hospitals with electronic exchange of patient medication history with ambulatory providers outside their system.
People Whose Provider Usually Asks About Medications and Treatments From Other Doctors
People under age 65 with a usual source of care whose health provider usually asks about prescription medications and treatments from other doctors, by education and chronic conditions, 2002-2013
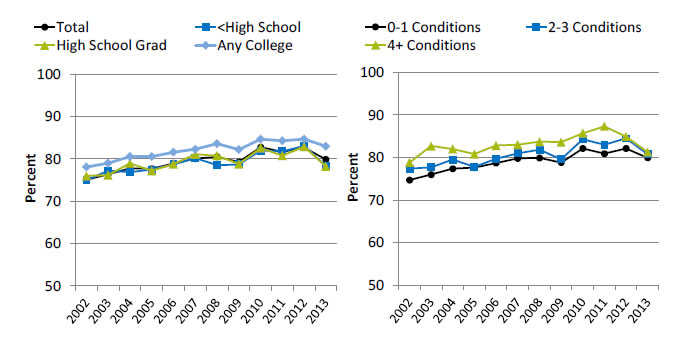
Left Chart:
| Education | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | 75.1 | 76.4 | 77.8 | 77.7 | 79 | 80.1 | 80.5 | 79.3 | 82.8 | 81.7 | 82.7 | 79.9 |
| Any College | 78.1 | 79 | 80.6 | 80.6 | 81.6 | 82.3 | 83.6 | 82.2 | 84.7 | 84.3 | 84.7 | 83 |
| High School Grad | 76 | 76.2 | 79 | 77.2 | 78.8 | 81.1 | 80.8 | 78.8 | 82.6 | 80.8 | 82.9 | 78.2 |
| <High School | 75 | 77.2 | 76.9 | 77.5 | 78.7 | 80.2 | 78.5 | 78.7 | 82 | 81.8 | 83.1 | 78.3 |
Right Chart:
| No. of Chronic Conditions | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0-1 Conditions | 74.7 | 76.0 | 77.4 | 77.6 | 78.7 | 79.8 | 79.9 | 78.8 | 82.1 | 80.9 | 82.1 | 79.9 |
| 2-3 Conditions | 77.4 | 77.7 | 79.5 | 77.8 | 79.7 | 81.0 | 81.8 | 79.6 | 84.3 | 83.0 | 84.5 | 80.7 |
| 4+ Conditions | 78.8 | 82.7 | 82.0 | 80.8 | 82.8 | 83.0 | 83.7 | 83.6 | 85.7 | 87.3 | 84.9 | 81.3 |
Source: Agency for Healthcare Research and Quality, Medical Expenditure Panel Survey, 2002-2013.
- Importance: Different providers may prescribe medications for the same patient. Patients must track all their medications, but medication information can be confusing, especially for patients on multiple medications. When care is not well coordinated and some providers do not know about all of a patient's medications, patients are at greater risk for adverse events related to drug interactions, overdosing, or underdosing. Medication information generated in different settings might not be sent to a patient's primary care provider, so the patient is the primary source of medication information. Actively gathering and managing all of a patient's medical information is an important part of care coordination.
- Trends:
- From 2002 to 2013, the percentage of people with a usual source of care whose health provider usually asked about prescription medications and treatments from other doctors improved from 75.1% to 79.9%.
- The percentage of people with a usual source of care whose health provider usually asked about prescription medications and treatments from other doctors showed improvement for patients of all educational levels and all groups with chronic conditions.
- Groups With Disparities:
- In 8 of 12 years, people with less than a high school education were less likely than people with any college to be asked about prescription medications and treatments from other doctors.
- In 7 of 12 years, high school graduates were less likely than people with any college to be asked about prescription medications and treatments from other doctors.
Hospitals With Electronic Exchange of Patient’s Medication History With Other Hospitals
Hospitals with electronic exchange of patient's medication history with hospitals outside their system, by region and geographic location, 2009-2013
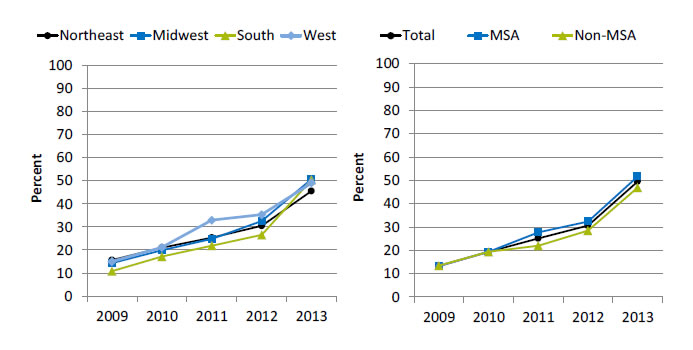
Left Chart:
| Region | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|
| Northeast | 15.6 | 21 | 25.3 | 30.5 | 45.6 |
| Midwest | 14.3 | 19.9 | 24.8 | 32.6 | 50.7 |
| South | 10.8 | 17.2 | 21.8 | 26.5 | 50.4 |
| West | 15 | 21.1 | 32.9 | 35.3 | 49 |
Right Chart:
| Location | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|
| Total | 13.4 | 19.4 | 25.2 | 30.7 | 49.6 |
| MSA | 13.3 | 19.4 | 27.8 | 32.4 | 51.7 |
| Non-MSA | 13.5 | 19.4 | 22 | 28.5 | 47 |
Key: MSA = metropolitan statistical area.
Source: American Hospital Association, Information Technology Supplement, 2009-2013.
- Importance: Health information exchange enables patients’ health information to follow them between delivery settings in order to support care coordination and avoid duplication of services. There is broad consensus that such connectivity is critical to improving care and reducing health care costs.
- Trends:
- From 2009 to 2013, the percentage of hospitals with electronic exchange of patient’s medication history with hospitals outside their system increased from 13.4% to 49.6%.
- From 2009 to 2013, the percentage of hospitals with electronic exchange of patient’s medication history with hospitals outside their system more than tripled for residents of all regions.
- From 2009 to 2013, the percentage of metropolitan hospitals that electronically exchanged patient medication history with hospitals outside their system significantly increased from 13.3% to 51.7%. The percentage of nonmetropolitan hospitals that electronically exchanged medication history increased from 13.5% to 47.0%.
- Differences:
- In 2013, hospitals in the Midwest were most likely to have electronic exchange with hospitals outside their system, followed by the South, West, and Northeast (50.7%, 50.4%, 49.0%, and 45.6%, respectively).
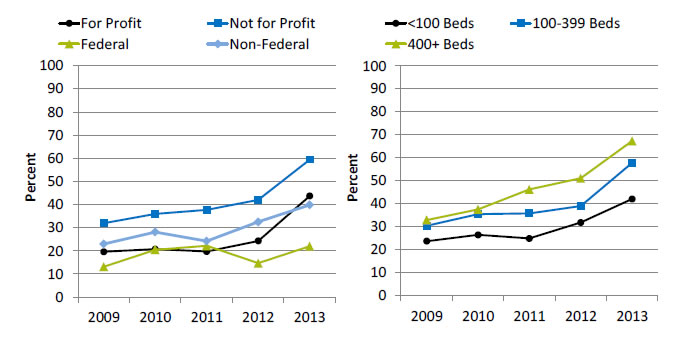
Hospitals With Electronic Exchange of Patient’s Medication History With Other Hospitals
Hospitals with electronic exchange of patient's medication history with hospitals outside their system, by ownership and bed size, 2009-2013
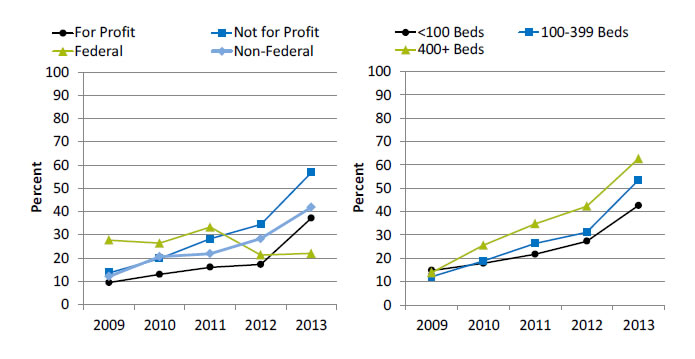
Left Chart:
| Hospital Type | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|
| For Profit | 9.4 | 12.9 | 16.0 | 17.2 | 37.2 |
| Not for Profit | 13.6 | 19.7 | 28.3 | 34.5 | 56.8 |
| Federal | 27.7 | 26.4 | 33.3 | 21.3 | 22 |
| Non-Federal | 12.0 | 20.6 | 21.8 | 28.3 | 41.8 |
Right Chart:
| Hospital Size | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|
| <100 Beds | 14.8 | 17.9 | 21.7 | 27.3 | 42.6 |
| 100-399 Beds | 12.1 | 18.9 | 26.4 | 31.1 | 53.5 |
| 400+ Beds | 13.9 | 25.6 | 34.8 | 42.3 | 62.7 |
Source: American Hospital Association, Information Technology Supplement, 2009-2013.
- Importance: Health information exchange enables patients’ health information to follow them between delivery settings in order to support care coordination and avoid duplication of services. There is broad consensus that such connectivity is critical to improving care and reducing health care costs.
- Trends:
- From 2009 to 2013, the percentage of hospitals that electronically exchanged patient medication history with hospitals outside their system increased:
- From 9.4% to 37.2% for for-profit hospitals.
- From 13.6% to 56.8% for not-for-profit hospitals.
- From 12.0% to 41.8% for non-Federal hospitals.
- For Federal hospitals, the percentage decreased from 27.7% to 22.0%.
- From 2009 to 2013, the percentage of hospitals that electronically exchanged patient medication history with hospitals outside their system increased:
- From 14.8% to 42.6% for hospitals with fewer than 100 beds.
- From 12.1% to 53.5% for hospitals with 100-399 beds.
- From 13.9% to 62.7% for hospitals with 400 or more beds.
- From 2009 to 2013, the percentage of hospitals that electronically exchanged patient medication history with hospitals outside their system increased:
- Differences:
- In 4 of 5 years, hospitals with fewer than 100 beds were less likely than large hospitals (400+ beds) to exchange information with hospitals outside their system.
- In 3 of 5 years, hospitals with 100-399 beds were less likely than large hospitals (400+ beds) to exchange information with hospitals outside their system.
Hospitals With Electronic Exchange of Patient’s Medication History With Ambulatory Providers
Hospitals with electronic exchange of patient's medication history with ambulatory providers outside their system, by region and geographic location, 2009-2013
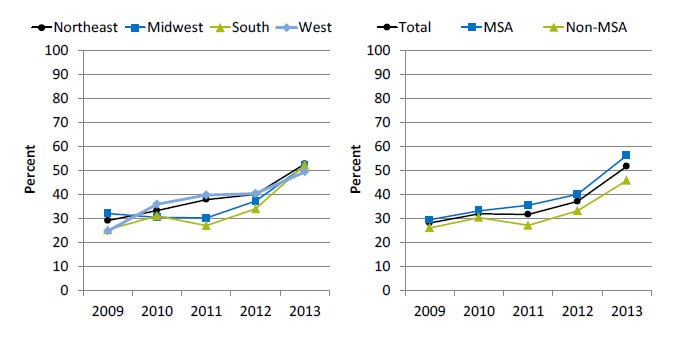
Left Chart:
| Region | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|
| Northeast | 29.2 | 33.4 | 38.0 | 40.2 | 52.8 |
| Midwest | 32.2 | 30.6 | 30.3 | 37.3 | 52 |
| South | 25.4 | 31.2 | 27.1 | 34.1 | 52.3 |
| West | 24.9 | 36.1 | 39.9 | 40.5 | 49.4 |
Right Chart:
| Location | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|
| Total | 28.2 | 32.1 | 31.8 | 37.2 | 51.8 |
| MSA | 29.6 | 33.3 | 35.6 | 40.2 | 56.4 |
| Non-MSA | 26.2 | 30.5 | 27.2 | 33.3 | 45.9 |
Key: MSA = metropolitan statistical area.
Source: American Hospital Association (AHA), Information Technology Supplement, 2009-2013.
- Importance: Health information exchange enables patients’ health information to follow them between delivery settings in order to support care coordination and avoid duplication of services. There is broad consensus that such connectivity is critical to improving care and reducing health care costs.
- Trends:
- From 2009 to 2013, the percentage of hospitals with electronic exchange of patient medication history with ambulatory providers outside their system increased from 28.2% to 51.8%.
- From 2009 to 2013, the percentage of hospitals that electronically exchanged patient medication history with ambulatory providers outside their system increased:
- From 29.2% to 52.8% in the Northeast.
- From 32.2% to 52.0% in the Midwest.
- From 25.4% to 52.3% in the South.
- From 24.9% to 49.4% in the West.
- From 2009 to 2013, the percentage of metropolitan hospitals that electronically exchanged patient medication history with ambulatory providers outside their system significantly increased from 29.6% to 56.4%. The percentage of nonmetropolitan hospitals that electronically exchanged patient medication history increased from 26.2% to 45.9%.
- Differences:
- In 2013, hospitals in metropolitan areas (56.4%) were more likely to exchange information with ambulatory providers outside their system than hospitals in nonmetropolitan areas (45.9%).
Hospitals With Electronic Exchange of Patient’s Medication History With Ambulatory Providers
Hospitals with electronic exchange of patient's medication history information with ambulatory providers outside their system, by ownership and bed size, 2009-2013
Left Chart:
| Hospital Type | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|
| For Profit | 19.6 | 20.8 | 19.7 | 24.3 | 43.7 |
| Not for Profit | 32.0 | 36.0 | 37.7 | 42 | 59.4 |
| Federal | 13.2 | 20.5 | 22.2 | 14.7 | 22 |
| Non-Federal | 23.0 | 28.1 | 24.2 | 32.5 | 39.8 |
Right Chart:
| Hospital Size | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|
| <100 Beds | 23.7 | 26.4 | 24.9 | 31.8 | 42.1 |
| 100-399 Beds | 30.4 | 35.5 | 35.8 | 39 | 57.8 |
| 400+ Beds | 32.9 | 37.5 | 46.2 | 51.1 | 67.3 |
Source: American Hospital Association, Information Technology Supplement, 2009-2013.
Note: Non-Federal hospitals refer to government hospitals.
- Importance: Health information exchange enables patients’ health information to follow them between delivery settings in order to support care coordination and avoid duplication of services. There is broad consensus that such connectivity is critical to improving care and reducing health care costs.
- Trends:
- From 2009 to 2013, the percentage of hospitals that electronically exchanged medication history with ambulatory providers outside their system increased:
- From 19.6% to 43.7% for for-profit hospitals.
- From 32.0% to 59.4% for not-for-profit hospitals.
- From 13.2% to 22% for Federal hospitals.
- From 23.0% to 39.8% for non-Federal hospitals.
- From 2009 to 2013, the percentage of hospitals that electronically exchanged patient medication history with hospitals outside their system increased:
- From 23.7% to 42.1% for hospitals with fewer than 100 beds.
- From 30.4% to 57.8% for hospitals with 100-399 beds.
- From 32.9% to 67.3% for hospitals with 400 or more beds.
- From 2009 to 2013, the percentage of hospitals that electronically exchanged medication history with ambulatory providers outside their system increased:
- Differences:
- In all years, not-for-profit hospitals were more likely to have electronic exchange with ambulatory providers outside their system than for-profit and Federal hospitals.
- In all years, hospitals with fewer than 100 beds were less likely than hospitals with 400 or more beds to electronically exchange medication history with ambulatory providers outside their system.



