National Healthcare Quality and Disparities Report
Trends in Quality Measures
Number and percentage of all quality measures that are improving, not changing, or worsening through 2013, overall and by NQS priority
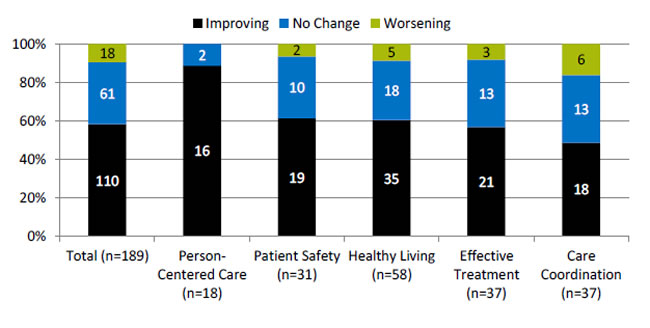
| Priority | Improving | No Change | Worsening |
|---|---|---|---|
| Total (n=189) | 110 | 61 | 18 |
| Person-Centered Care (n=18) | 16 | 2 | |
| Patient Safety (n=31) | 19 | 10 | 2 |
| Healthy Living (n=58) | 35 | 18 | 5 |
| Effective Treatment (n=37) | 21 | 13 | 3 |
| Care Coordination (n=37) | 18 | 13 | 6 |
Key: n = number of measures.
Note: For the majority of measures, trend data are available from 2001 to 2013. Measures of Care Affordability are included in the Total but not shown separately.
For each measure with at least four estimates over time, log-linear regression is used to calculate average annual percentage change relative to the baseline year and to assess statistical significance. Measures are aligned so that positive change indicates improved care.
- Improving = Rates of change are positive at 1% per year or greater and are statistically significant.
- No Change = Rates of change are less than 1% per year or not statistically significant.
- Worsening = Rates of change are negative at -1% per year or greater and are statistically significant.
- Through 2013, across a broad spectrum of measures of health care quality, 60% showed improvement.
- Nearly all measures of Person-Centered Care improved.
- About 60% of measures of Effective Treatment, Healthy Living, and Patient Safety improved.
- Fewer than half of measures of Care Coordination improved.
- Fewer than a dozen measures of Care Affordability are tracked in the report, too few to summarize this way.
Person-Centered Care Measures That Achieved Success
- Person-Centered Care measures that achieved 95% performance:
- Children who had a doctor's office or clinic visit in the last 12 months whose health providers—
- Sometimes or never listened carefully.
- Sometimes or never explained things in a way they or their parents could understand.
- Sometimes or never showed respect for what they or their parents had to say.
- Children who had a doctor's office or clinic visit in the last 12 months whose health providers—
- No measures improved quickly (greater than 10% average annual percent change).
Measures that achieve 95% performance will no longer be reported in the chartbook. The measures will continue to be tracked and can be found in the QDR data query system.
Disparities in Quality of Care
Number and percentage of person-centered care measures for which members of selected groups experienced better, same, or worse quality of care compared with reference group
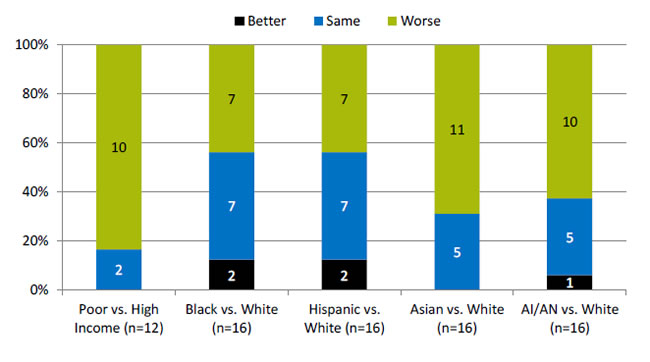
| Poor vs. High Income (n=12) | Black vs. White (n=16) | Hispanic vs. White (n=16) | Asian vs. White (n=16) | AI/AN vs. White (n=16) | |
|---|---|---|---|---|---|
| Better | 2 | 2 | 1 | ||
| Same | 2 | 7 | 7 | 5 | 5 |
| Worse | 10 | 7 | 7 | 11 | 10 |
Key: n = number of measures; AI/AN = American Indian or Alaska Native.
Note: Poor indicates family income less than the Federal poverty level; High Income indicates family income four times the Federal poverty level or greater. Numbers of measures differ across groups because of sample size limitations. For most measures, data from 2012 are shown.
The relative difference between a selected group and its reference group is used to assess disparities.
- Better = Population received better quality of care than reference group. Differences are statistically significant, are equal to or larger than 10%, and favor the selected group.
- Same = Population and reference group received about the same quality of care. Differences are not statistically significant or are smaller than 10%.
- Worse = Population received worse quality of care than reference group. Differences are statistically significant, are equal to or larger than 10%, and favor the reference group.
- For 83% of person-centered care measures, people in poor households received worse care than people in high-income households.
- Racial and ethnic disparities in person-centered care were also common.
Person-Centered Care Measure With Elimination of Disparities
- Adults who had a doctor’s office or clinic visit in the last 12 months whose health providers sometimes or never spent enough time with them
Person-Centered Care Measures With Widening of Disparities
- Adults who had a doctor’s office or clinic visit in the last 12 months who reported poor communication with health providers.
- Children who had a doctor’s office or clinic visit in the last 12 months whose parents reported poor communication with health providers.
- Adult hospital patients who sometimes or never had good communication with—
- Doctors in the hospital.
- Nurses in the hospital.
- Rating of health care 0-6 on a scale from 0 to 10 (best grade) by—
- Adults who had a doctor's office or clinic visit in the last 12 months.
- Children who had a doctor's office or clinic visit in the last 12 months.
- Adult hospital patients who sometimes or never had good communication about medications they received in the hospital.
The measures of poor communication for adults and children are composites of four measures, all of which individually showed widening of disparities:
- Adults [Children] who had a doctor’s office or clinic visit in the last 12 months whose health providers sometimes or never listened carefully to them.
- Adults [Children] who had a doctor’s office or clinic visit in the last 12 months whose health providers sometimes or never explained things in a way they could understand.
- Adults [Children] who had a doctor’s office or clinic visit in the last 12 months whose health providers sometimes or never showed respect for what they had to say.
- Adults [Children] who had a doctor’s office or clinic visit in the last 12 months whose health providers sometimes or never spent enough time with them.
The last two measures are not included in this chartbook. Data are available through the QDR data query system.



