Two-Day Training Content
The Team Leadership Module provides an overview of what teams are as well as how to lead teams effectively. The overview of teams can be taught in about 40 minutes using the approach described
The Team Leadership Module provides an overview of what teams are as well as how to lead teams effectively. The overview of teams can be taught in about 40 minutes using the approach described below. Training related to team leadership and leadership tools will take an additional 75 minutes. Depending on the time you have available, you may expand some training activities or drop some content totally to focus on the concepts or tools most relevant to your participants. Components you can use in this section include the following:
Teams Overview
- Introduction: 2 minutes
- Defining teams: 2 minutes
- Teamwork exercise: 6 minutes
- Integrating patients and families into teams: 5 minutes
- Multi-team systems: 10 minutes
- Team structure video discussion: 10 minutes
- Applying TeamSTEPPS exercise: 5 minutes
Team Leadership
- Leadership exercise: 15 minutes
- Introduction: 3 minutes
- Team leaders: 4 minutes
- Defining the plan and assigning tasks: 4 minutes
- Sharing the plan (brief): 4 minutes
- Exercise: Brief: 15 minutes
- Monitoring and modifying the plan (huddle): 3 minutes
- Reviewing the team’s performance (debrief): 8 minutes
- Facilitating conflict resolution and teamwork: 3 minutes
- Team formation video: 8 minutes
- Tools and strategies summary: 3 minutes
- Applying TeamSTEPPS exercise: 5 minutes
Teaching Goals
It’s important to continuously reinforce your enthusiasm for TeamSTEPPS and its importance to patients and healthcare workers. You also should continue to foster mutual respect, fun, and transparency through the use of active learning and listening throughout the section.
Specific goals for teaching this section include some related to an understanding of team structure and others focused on team leadership. Objectives for each are identified below.
Teams and Team Structure
- Understand the benefits of teamwork and clear team structure.
- Define a “team.”
- Identify the roles of patients and family caregivers within the care team.
- Describe the components and composition of a multi-team system.
Team Leadership
- Describe how leadership affects team processes and outcomes.
- Identify diverse types of team leaders.
- Describe the activities involved in successfully leading teams.
- Describe the tools for leading teams, including briefs, huddles, and debriefs.
- Apply the tools for leading teams to specific clinical scenarios.
Teaching Process
Introduction
Referring to Slide 1, “Team Leadership,” welcome the participants back to the start of Module 2. (Module 1 laid the groundwork needed to understand teams and how to lead them.) Explain that teaching about team leadership needs to start by clarifying what teams are and how they relate to each other in healthcare settings.

To further introduce teams and team structure, use Slide 2, “Understanding Teams and Team Structure.” Ask participants to identify what team comes to mind when they think of effective teams. You’ll probably get the names of sports teams, musical groups, or teams that collaborated to achieve a vital task. Their examples may differ from each other but note that they all have things in common. These common attributes are the topic of this module.
- Understanding the benefits of team structure in teamwork.
- Defining a “team.”
- Identifying the role of patients and their families as part of the care team.
- Describing the components and composition of a multi-team system, or MTS.
Defining Teams
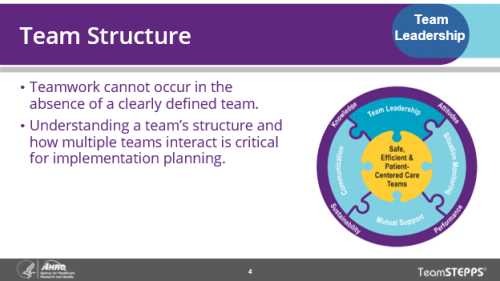
Explain that team structure (Slide 4) refers to the composition of an individual team or of an MTS. Team structure is an integral part of the teamwork process. Properly structured patient care teams facilitate effective communication, leadership, situation monitoring, and mutual support. Conversely, effective communication and leadership are necessary in establishing a good team structure at the outset.
Proper team structure can promote teamwork by including a clear leader, involving the patient, and ensuring that all team members commit to their roles.
Ask the participants why the structure of teams matters. Use their responses to reinforce the message that teamwork cannot occur in the absence of a clearly defined team. Note that for TeamSTEPPS, identifying the teams involved will affect who will need to be trained on the TeamSTEPPS tools.
Before displaying Slide 5, “What Defines a Team?,” ask the participants how they would define a team. Use their responses to introduce the definition of a team on the slide. While it’s not necessary to read this definition, note that team members:
- Include anyone involved in the process of patient care who can take action, including the leader.
- Have clearly defined roles and responsibilities.
- Are accountable to the team for their actions.
- Must stay continually informed for effective team functioning.
Explain (or mention) that teams can be virtual and that teams may have changing participants because of staffing and scheduling. These factors make teamwork more challenging but also more important to effective team functioning.
Teamwork Exercise
If time permits, use Slide 6 (Team Exercise) to elaborate on the centrality of teams to patient care through the following exercise. Have the group break into smaller groups, either in person or online using breakout rooms. Once the groups are formed, have them take 5 minutes to do the following:
- Identify a patient type that participants may frequently support—for example, patients entering the emergency department, a newly admitted nursing home resident, or a patient with an undiagnosed condition.
- List all the people (names or positions) responsible for directly or indirectly supporting the care of this type of patient.
- Are they all on one team or parts of separate teams supporting the patient?
Have each group report out on their patient type and the numbers of people on the teams supporting them. Probe to see whether groups have included night or weekend staff, the patient, family caregivers, medical interpreters, or other team members that are frequently overlooked. Use the exercise to emphasize the importance of these teams and the number of teams and team members needed to care for patients.
Integrating Patients and Families Into Teams
Using Slide 7 (Partnering with the Patient), ask participants for a story of when a patient was overlooked in a team decision that affected their care and what happened as a result. Use this story to reinforce the message that patients and their families are central to healthcare teams.
Further, ask participants to share any strategies besides those listed on Slide 8, “How Teams Can Foster Patient and Family Caregiver Involvement,” to engage patients in their teams. This discussion will require them to process the strategies on the slide and also think about additional approaches.
Before introducing the next slide (Slide 9, “Parents and Family Caregivers Can Function Effectively in Their Teams by:”), ask participants to share how efforts to include the patient have evolved since they entered healthcare. Use positive stories to celebrate progress but note that there is still room for improvement to achieve consistently patient-centered care.
Once you have introduced the slide, ask participants which of the strategies for embracing patients and families are used effectively where they work and where the biggest opportunities are for improvement. As you introduce Slide 9, note that it’s a mistake to define patient involvement in their care team as “doing what they are told.” Explain that patients and families are more likely to cooperate if they’re involved in discussions about their care plan and agree to it.
Patients and their family caregivers can use patient portals to understand the condition, ask questions, or review upcoming appointments. Ask participants for other examples of how patients and families can be effective team members. Note that the healthcare team may benefit from the patient and family caregivers in ensuring the patient receives effective and safe care. If you have time, ask a participant to share a story of when a team didn’t listen to a patient or family caregiver and how the failure to listen caused harm or a near-miss.
Multi-Team Systems
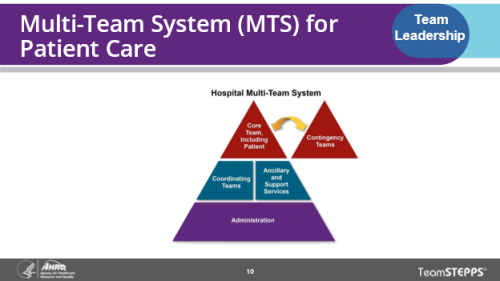
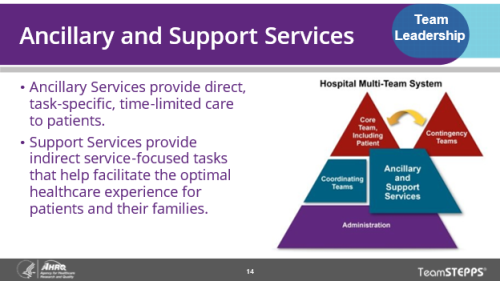
As you introduce Slide 10, “Multi-Team System (MTS) for Patient Care,” note that multiple teams are involved in patient care. Each team within an MTS is responsible for various parts of patient care, but the teams must coordinate with each other to ensure quality care. This coordination can be challenging within hospitals. It can be even more complex for outpatients obtaining care and support from providers affiliated with multiple care systems that do not share the same electronic medical record. Explain that for TeamSTEPPS to be effective, all teams involved need to understand and use the relevant tools.
Note that a multi-team system within a hospital includes the Core Team, the Contingency Team, the Coordinating Team, Ancillary and Support Services, and Administration. For outpatients, team structures may be even more complex and varied. Frequently patients may have teams from different care settings supporting them. For example, a nursing home resident may have teams from their nursing home, teams from outpatient practices that care for them, and, if they are hospitalized, teams in the hospital. Some team meetings may occur in person with the patient and team members, while others may include a mix of in-person and virtual attendees. Acknowledge the challenges these factors can create for the patient and these teams in understanding and coordinating efforts to provide safe and effective care.
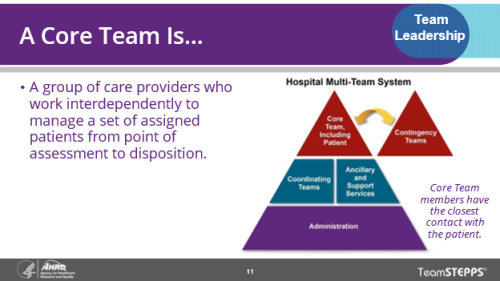
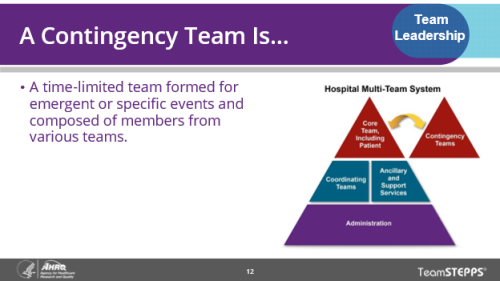
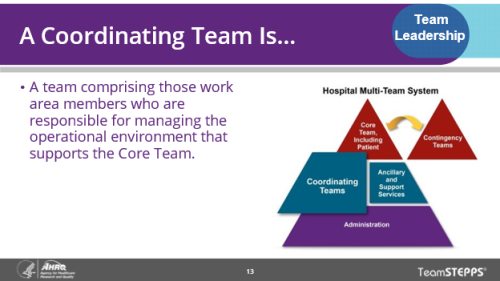
Using Slide 11, “A Core Team Is,” and the following four slides, call attention to the different teams making up a multi-team system. It’s not critical for participants to remember all the types of teams. However, emphasize that the patient is always part of the Core Team and may be involved with other teams less directly.
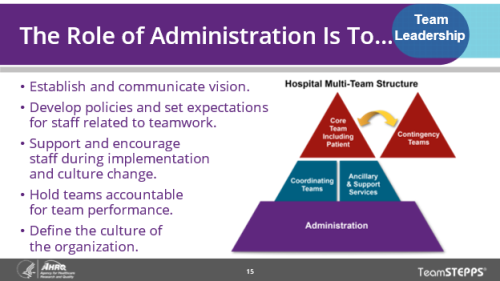
If participants include administrators, point out the ways administration can create an environment and culture to foster effective teamwork. These include:
- Establishing and communicating vision.
- Developing and enforcing policies and procedures that clearly articulate the roles and responsibilities of the other teams and team members.
- Setting expectations for staff.
- Providing resources needed for successful implementation.
- Holding teams accountable for team performance.
- Defining the culture of the organization.
Covering Slides 11-15 quickly is fine. However, ensure participants recognize the interdependencies between multiple teams in any care setting.
Team Structure Video Discussion
Using the Team Structure Video (embedded in Slide 16) or an alternative also listed in section 2 above), ask the class to view the video and then answer the questions on Slide 17, “Team Structure Discussion.”
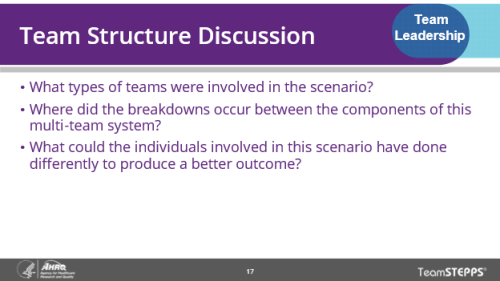
- What types of teams were involved in the team structure video scenario?
- The Core Team?
- The nurse (Amy). The physician was not involved at all.
- The Coordinating Team?
- The clerk (Sheri).
- The Contingency Team?
- No members of this team appeared in the video. However, when Mrs. Everett coded, the members of the team that responded would make up the Contingency Team.
- Ancillary and Support Services?
- The med tech (Greg).
- The Core Team?
- Where did the breakdowns occur between the components of this multi-team system?
- The med tech did not provide any information to the clerk to indicate there was a real concern that the clerk needed to share with the nurse.
- The med tech and the nurse never followed up with one another to share information.
- Because the nurse was not aware of the med tech’s observations and concerns, the physician was never alerted to the changes in Mrs. Everett’s behavior.
- What could the individuals involved in this scenario have done differently to produce a better outcome?
Applying TeamSTEPPS Exercise
If the training includes participants preparing to implement TeamSTEPPS in their facility, use Slide 18, “Applying TeamSTEPPS Exercise,” to facilitate their efforts to apply their understanding of teams to the problem they are attempting to solve. Using the TeamSTEPPS Implementation Worksheet, they can think about the area in which they intend to use TeamSTEPPS to improve performance.
Ask them to think about:
- What types of team members make up each team?
- How do the teams in your unit or area interact with one another?
- How might each of the teams fit into your TeamSTEPPS implementation plan?
Ask a few individuals to report on the multi-team system that will be affected by their intended TeamSTEPPS implementation. If most participants are the only representatives from their organization, you may skip this activity or pose a hypothetical scenario for the table groups to work through as an example.
Leadership Exercise
As you transition from the discussion of teams and team structure to leadership (Slide 19, “Leading Teams”), note that leadership is key to effective teams in a multi-team system. Ask participants to return to their breakout groups (in person or virtual) and to follow the instructions for the leadership exercise on Slide 20. Give them 6-8 minutes to develop their responses.
Upon completion, have one group share their list of traits of an effective team leader. Then ask the other groups what they would add to this list. Next, pick a different group to share their list of traits of ineffective leaders and ask the other groups to add to this list. Then lead the entire group in a discussion of whether leadership is innate or something that can be taught and learned. Note that while some people may have traits and life experiences that make them better leaders, leadership is a skill that anyone can become better at. The next section will show participants how.
Introduction
Display the five learning objectives shown on Slide 21. You don’t need to read all of these, but participants should know the objectives for the following section.
Team Leaders
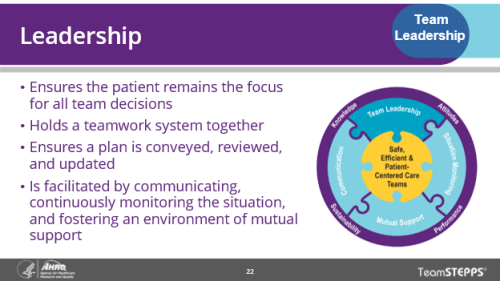
Remind participants that team leadership is one of the four pillars of TeamSTEPPS. Using Slide 22, “Leadership,” note the four contributions that leaders should make to their teams, beginning with keeping the patient at the center of all team decisions.
Team leaders can be designated or situational, as explained in Slide 23, “Types of Team Leaders.” Most team members may function as a team leader in some situations, and many team members may acquire more leadership responsibilities over time. Everyone should see leadership as relevant to their job, because they may play that role at times and not just follow others.
Ask participants to review the list of characteristics of an effective team leader (using Slide 24, “Effective Team Leaders”) and for someone to share a story of a time when a leader’s failure to do one of these things harmed the patient or team. See whether any other traits of effective leaders should be added to this list.
Defining the Plan and Assigning Tasks
Note that one responsibility of the leader is to define the plan for caring for the patient (Slide 25, “Defining the Plan”). While the leader may define the plan, it should always be based on listening to others on the team to ensure their insights are considered. Effective leaders give teams an opportunity to comment or make suggestions for improving the plan, including the patient or family caregivers.
If you have time, you can ask the class:
- How do your team leaders communicate a care plan to the care team?
- Which strategies have been effective, and which have not been effective?
- How do your team leaders communicate changes to the care plan to the care team?
You may choose to modify Slide 26, “Case Study Discussion,” if most participants work in non-acute care settings. Every care setting has processes that can be confusing or complex. Alternatively, elicit a case study from the participants or have each small group create their own. In any of these cases, ask the group to consider:
- How can the plan address patient needs, time, people, equipment, and information?
- What other principles of effective leadership and planning should guide the plan and how it is created?
Note that a plan will not be successful unless every team member knows what their individual tasks and responsibilities are (Slide 27, “Assigning Tasks and Responsibilities”). Each of the four actions on the slide is important, but the instructor doesn’t need to read all of them. Ask participants to share an example of when a failure to assign tasks and roles created confusion or harmed a patient. Emphasize the need to allow feedback on the assignments. Some team members may have other responsibilities that could keep them from performing the tasks they’ve been assigned. If all team members agree to their responsibilities and tasks, they’ve made a commitment they will feel more obligated to keep.
Sharing the Plan (Brief)
Introduce the brief (Slide 28, “Sharing the Plan: Briefs”) as a strategy for sharing the plan (or adjustments to the plan) with other team members. Review the four key goals of a brief. Next ask the class to watch the briefing video in the slides, or as an alternative, to observe a brief. Use the two discussion questions to have participants reflect on the brief they’ve observed.
- How did the video illustrate each recommended phase of a team brief?
- Which elements of the brief are most commonly omitted in teams you are part of?
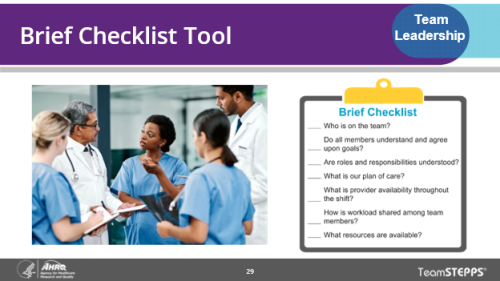
As you introduce Slide 29, “Brief Checklist Tool,” explain that the tool is a useful resource for ensuring the completeness of each brief. Ask participants whether any use a brief checklist and, if so, how useful it has been. Note that the checklist is both a useful mental tool for leaders to ensure they haven’t left out key brief elements and a way for leaders to assess how well briefs are being conducted. Also note that when teams are supporting patients with limited English proficiency, it is important to include the medical interpreter in the team and in relevant team briefs, huddles and debriefs.
Exercise: Brief
The additional brief exercise (Slide 30, “Exercise: Brief”) can be used by selecting a scenario as reflected in instruction 1 on the slide. If participants are from the same facility or unit preparing to implement TeamSTEPPS, instruct them to focus on a team from their unit or group. Explain that the purpose of this exercise is to gain experience with checklists that can help facilitate briefs.
If participants are from different organizations, omit this exercise and spend more time in other class discussions.
The TeamSTEPPS curriculum now includes a set of video-based simulation training activities that teach key concepts related to briefs, huddles, and debriefs. You may want to use parts of or all of that resource to teach these concepts. Select to view the video and materials.
Monitoring and Modifying the Plan (Huddle)
Introduce the huddle as a tool for communicating adjustments to a care plan that is already in place (Slide 31, “Monitoring and Modifying the Plan: Huddle”). When a plan needs to be altered because of changes in the patient’s condition or team membership or because aspects of the current plan are not working, either the designated leader or a situational leader should convene a huddle. When leading teams, it is important to quickly and effectively communicate such changes so the team members all know the plan for providing the best care to the patient.
Explain that information updates within the team should occur as often as needed. At times, the designated team leader may be managing multiple patients simultaneously and relying on other team members to provide vital information about the patient’s status and how the established care plan is working. Such important updates can be provided during huddles.
Ask participants to watch the huddle illustrated in the embedded video in Slide 31 or another video based on a different care setting. Then ask the class to discuss:
- What event necessitated the need for the huddle?
- The patient’s electrocardiogram indicated a possible acute myocardial infarction, requiring additional team action, planning, and coordination due to the emergent nature of the patient’s condition.
- What key information was shared in the huddle?
- Most recent patient history and current status
- Distribution of tasks and workload
- Emergent plan of care
- What change could they make in their teams to improve the quality of their own huddles?
Reviewing the Team's Performance (Debrief)
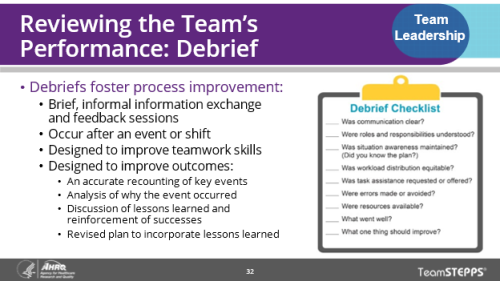
Explain that another tool for team leaders is the debrief (Slide 32, “Reviewing the Team’s Performance: Debrief”) and that the goal of a debrief is to improve team performance. Note that the focus of debriefs should be on team performance and that if a single team member had a performance problem, that should be addressed in a different setting. Debriefs will be most effective under the following conditions:
- They are conducted in an environment where mistakes are viewed as learning opportunities.
- They are a brief (about 3 minutes or less) team event, typically initiated and facilitated by the team leader.
- They relate to specific team goals or address specific issues related to recent team actions.
- They focus on performance improvement. It is important to reinforce what went well and avoid assigning blame or failure to any individual regarding what did not go well.
Review the four ways debriefs can help with process improvement and introduce the debrief checklist as a tool that can help leaders improve their ability to debrief effectively.
Ask your trainees to watch the embedded debrief video (Slide 33, “Debrief Video ”) or another example of a debrief drawn from the TeamSTEPPS curriculum or another source.
Afterward, ask the participants:
- What were some of the positive effects from this debrief?
- Team members shared best practices that improved individual and overall team performance.
- All team members were encouraged to participate.
- It reinforced that teamwork skills produce good outcomes.
- How would you describe the tone Dr. Upton set for the debrief?
- Set a positive tone for open communication.
- Encouraged feedback.
- Facilitated lessons learned.
- Reinforced team behaviors and successes with the team.
- What one change would make debriefs in their teams work more effectively?
Facilitating Conflict Resolution and Teamwork
Next, explain that leaders play a key role in facilitating conflict resolution (Slide 34). Conflict is inevitable and can be caused by differences in clinical knowledge, work approaches, values, opinions, or personalities. Resolution of conflict is necessary in the delivery of safe, quality care. Leadership skill in conflict resolution can enhance team effectiveness and performance. An effective team leader does not allow interpersonal or irrelevant issues to negatively affect the team.
In addition to conflict, other disruptive behaviors can affect the effectiveness of teams. Other tools for managing conflict include the Two-Challenge Rule and the DESC script that will be discussed in the Mutual Support module.
Explain that effective team leaders must model, value, and reinforce effective team behaviors. This approach helps team members understand performance expectations and helps cultivate desired team behaviors. Designated team leaders should engage in the five actions noted on Slide 35, “Promoting and Modeling Teamwork.”
Team Formation Video
If time permits, ask participants to watch the case of 27-year-old Mrs. Keys (Slide 36, “Team Leadership Video”). Instruct them to consider the questions on the screen while they watch a team that uses effective and timely leadership strategies, including:
- Briefs.
- Huddles.
- Brief checklists.
- Conflict resolution.
- Debriefs.
Labor & Delivery: Successful Outcome Using TeamSTEPPS Techniques (5:03)
Once the video is complete, ask participants to discuss (either as a group or in their breakout sessions):
- What leadership tools and strategies did Dr. Dean use?
- Conducted a huddle with the team before registered nurse shift change
- Briefed team about concerns and current status of Mrs. Keys
- Established himself as current situational team leader
- Verbalized the current plan of care
- How did the nurses demonstrate leadership?
- Conducted a huddle at shift change to discuss high threats, even with competing tasks and distractions
- Prompted the “timeout” checklist
- Offered valuable feedback during the debrief
- What leadership tools and strategies did Dr. Upton use?
- Conducted a huddle for the emergent need to perform a C-section
- Used a preprocedure brief checklist
- Included the patient in the “timeout”
- Held a debrief to recap the event and share lessons learned
- Empowered team members to speak freely and share team workload
Team leaders ensure that information is being shared, all team members have the resources they need to do their job, the situation within the work environment is continually monitored, and appropriate behaviors are modeled and reinforced across the team.
Tools and Strategies Summary
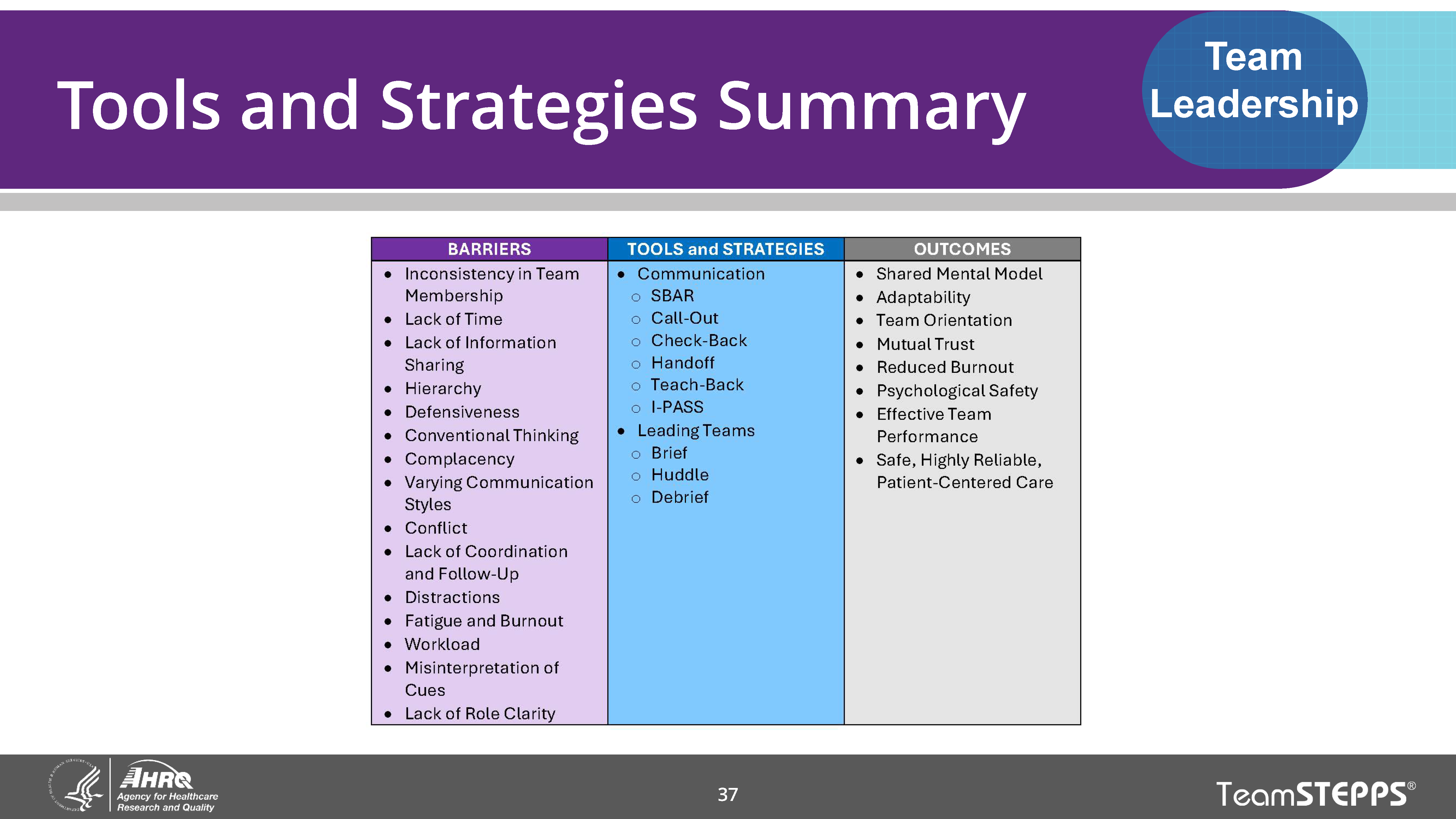
If you have time, ask the class which team leadership tool you’ve just discussed that they are the most eager to use. Encouraging participants to publicly identify a tool they intend to try will increase the likelihood that they will begin to use it in their work.
Applying TeamSTEPPS Exercise
As specified in Slide 38, “Applying TeamSTEPPS Exercise,” instruct the groups to think about these things:
- Who is the designated leader on the team that is at the center of your TeamSTEPPS implementation?
- Are there teamwork issues that this leader must work with you to address?
- If so, what are the issues and can any of the tools or strategies learned in this module be used to address them?
Ask a few individuals to report on their responses to these three questions.



