Breaking Down Barriers to Aseptic Catheter Insertion
Slide Presentation
Slide 1
Breaking Down Barriers to Aseptic Catheter Insertion
Milisa Manojlovich, PhD, RN, CCRN
Associate Professor
University of Michigan School of Nursing
Stacy Martin, RN, BSN, CIC
Manager, Infection Prevention
Moffitt Cancer Center
Stephanie Carraway, MPH candidate
Infection Prevention Specialist
Moffitt Cancer Center
Images: Photos of the three presenters.
Slide 2
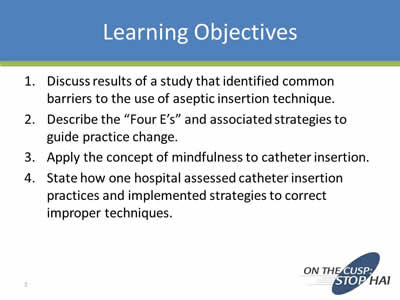
Learning Objectives
- Discuss results of a study that identified common barriers to the use of aseptic insertion technique.
- Describe the “Four E’s” and associated strategies to guide practice change.
- Apply the concept of mindfulness to catheter insertion.
- State how one hospital assessed catheter insertion practices and implemented strategies to correct improper techniques.
Slide 3
Polling Question
What is your role at the hospital?
- Infection Preventionist
- Physician
- Nurse leader or nurse educator
- Bedside nurse
- Other…
Slide 4
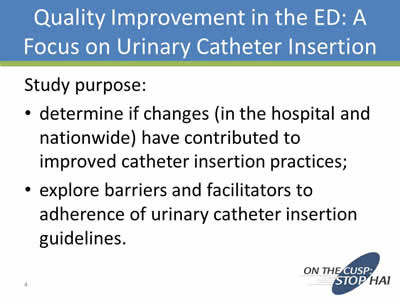
Quality Improvement in the ED: A Focus on Urinary Catheter Insertion
Study purpose:
- Determine if changes (in the hospital and nationwide) have contributed to improved catheter insertion practices;
- Explore barriers and facilitators to adherence of urinary catheter insertion guidelines.
Slide 5
Methods
- 2 teams of nursing students
- 0630 – 2100, in 4 or 8 hour blocks of time
- January 29 – June 30, 2014
- Observation, checklists, field notes
Slide 6
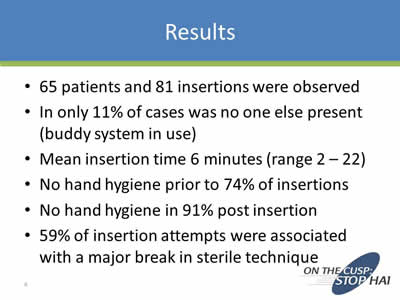
Results
- 65 patients and 81 insertions were observed
- In only 11% of cases was no one else present (buddy system in use)
- Mean insertion time 6 minutes (range 2 – 22)
- No hand hygiene prior to 74% of insertions
- No hand hygiene in 91% post insertion
- 59% of insertion attempts were associated with a major break in sterile technique
Slide 7
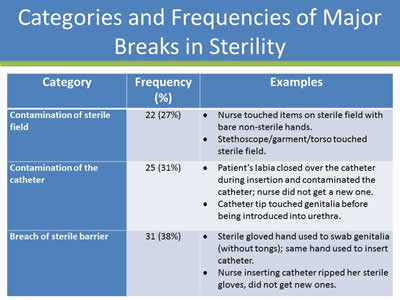
Categories and Frequencies of Major Breaks in Sterility
| Category | Frequency | Examples |
|---|---|---|
| Contamination of sterile field | 22 (27%) |
|
| Contamination of the catheter | 25 (31%) |
|
| Breach of sterile barrier | 31 (38%) |
|
Slide 8
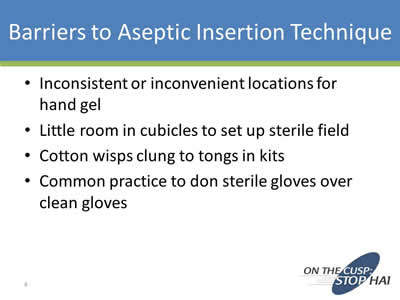
Barriers to Aseptic Insertion Technique
- Inconsistent or inconvenient locations for hand gel
- Little room in cubicles to set up sterile field
- Cotton wisps clung to tongs in kits
- Common practice to don sterile gloves over clean gloves
Slide 9
Successful Strategies to Guide Practice Change: 4 E’s
- Engagement
- Education
- Execution
- Evaluation
Slide 10
Engagement
- Activities strictly within the nursing domain may not perceived as being important or of much value, compared to activities that cross disciplinary boundaries.
- Catheter insertion may be perceived as one of many “tasks” rather than as a component of evidence-based practice.
Slide 11
Strategies to Promote Engagement
- Aseptic insertion of indwelling urinary catheters is a component of evidence-based practice, no matter what the discipline.
- Develop a culture where evidence-based practice is recognized and rewarded.
- Think in terms of nursing practice components rather than a set of tasks to be completed.
Slide 12
Education
- There are few similarities between the controlled environment in which health care providers learn to insert catheters and the chaotic work environments in which they practice.
- Health care providers may not have the skills to maintain aseptic technique given work environment constraints.
- They may observe peers inserting catheters and notice that aseptic technique is not used.
Slide 13

Education Strategies
- Develop competencies and consider annual competency testing for catheter insertion technique.
- Require that there be oversight for catheter insertion by a licensed provider.
- Use a buddy system at first when catheter insertion is necessary.
- Develop a policy on catheter insertion techniques if none is in place.
Slide 14
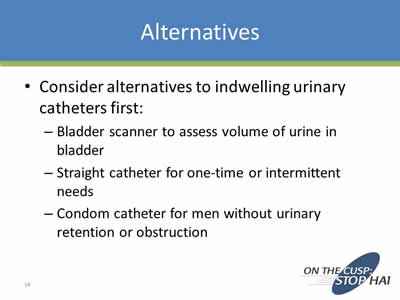
Alternatives
- Consider alternatives to indwelling urinary catheters first:
- Bladder scanner to assess volume of urine in bladder
- Straight catheter for one-time or intermittent needs
- Condom catheter for men without urinary retention or obstruction
Slide 15
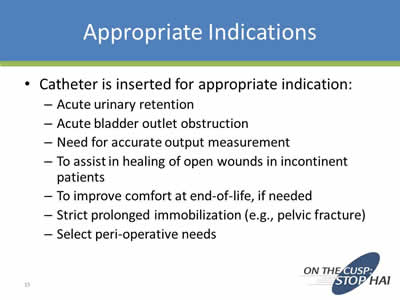
Appropriate Indications
- Catheter is inserted for appropriate indication:
- Acute urinary retention
- Acute bladder outlet obstruction
- Need for accurate output measurement
- To assist in healing of open wounds in incontinent patients
- To improve comfort at end-of-life, if needed
- Strict prolonged immobilization (e.g., pelvic fracture)
- Select peri-operative needs
Slide 16
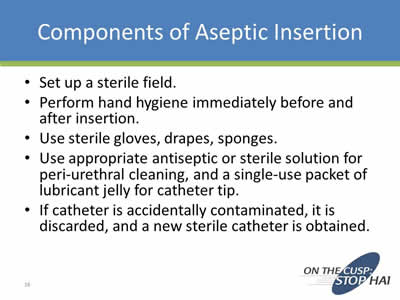
Components of Aseptic Insertion
- Set up a sterile field.
- Perform hand hygiene immediately before and after insertion.
- Use sterile gloves, drapes, sponges.
- Use appropriate antiseptic or sterile solution for peri-urethral cleaning, and a single-use packet of lubricant jelly for catheter tip.
- If catheter is accidentally contaminated, it is discarded, and a new sterile catheter is obtained.
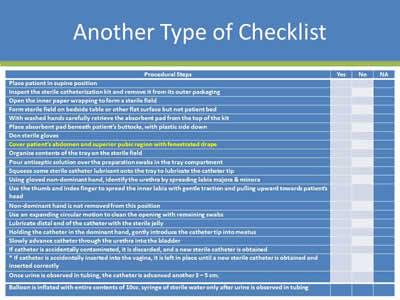
Slide 17
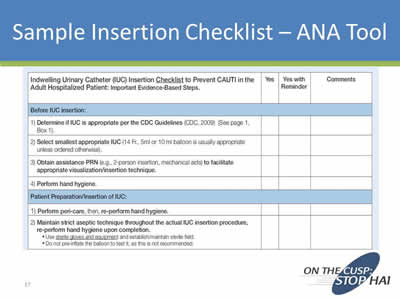
Sample Insertion Checklist – ANA Tool
Image: Screen shot of a sample insertion checklist.
Slide 18
Another Type of Checklist
Image: Screen shot of a catheter insertion checklist.
Slide 19
Execution: Lack of Awareness
- Those who insert catheters may not be aware of the consequences when aseptic insertion technique is violated.
- Patients move from the ED to other units, and there is no systematic process to let ED staff know of patient outcomes.
Slide 20
Execution: Raising Awareness
- Unit level strategies:
- Report monthly CAUTI rates during staff meetings.
- Post monthly CAUTI rates in a prominent location.
- Organizational level strategies:
- Post CAUTI rates for all units, so that comparisons can be seen.
Slide 21
Execution: Lack of Resources
- Time, financial, space, equipment constraints can all contribute to situations where aseptic insertion techniques are not used.
- Variation in human resources contributes to poor execution as well:
- High turnover
- Understaffing
- Enough IPs to do the work
Slide 22
Execution Strategies that Focus on Improving or Reallocating Resources
- Adequate supplies:
- Over-the-bed tables
- Hand sanitizers
- Sterile gloves
- Best type of kit to stock for your patient population
- Would individual supplies be better than a kit?
- Adequate facilities for hand hygiene
- Location:
- Where are kits located in relation to where the procedure is to take place?
Slide 23
Other Strategies to Improve Execution
- A non-punitive culture
- Visible and supportive leadership
- Identify system-wide barriers to aseptic insertion:
- Lack of adequate supplies
- Lack of space for sterile field set-ups
- Lack of manpower
- Allocate resources to overcome as many barriers as possible
Slide 24
Evaluation
- CAUTI rates, catheter days, costs of UTIs
- Compliance with catheter insertion guidelines
- Compliance with catheter maintenance and care
- Hand hygiene rates
Slide 25
Other Resources
- www.Catheterout.org
- Strategies to Prevent CAUTI in Acute Care Hospitals, 2014 Update from SHEA:
http://www.jstor.org/stable/10.1086/675718
Slide 26
Mindful Practice
- Catheter insertion is really a very complex task:
- Multiple steps
- Something can go wrong at any point
- Does not evoke visceral response, yet harms are very real
Slide 27
Mindfulness
- A mode of thinking based on sorting and prioritizing cognitive tasks
- Used to achieve organizational goals
- A flexible state of mind “engaged in the present with acute awareness of external events”
Slide 28
Becoming Mindful
- Mindful practice is a cognitive process that tailors evidence-based practice recommendations to the individual patient by considering patient and contextual factors.
- Maintain a big picture view.
- Stay “in the moment.”
http://www.jstor.org/stable/10.1086/673147
Slide 29
Conclusion
- Urinary catheters should only be inserted if there is an appropriate indication.
- Aseptic insertion technique is strongly recommended, but multiple barriers can arise.
- An approach that blends “The 4 E’s” with mindfulness may be successful at overcoming barriers.
Slide 30

Moffitt Cancer Center
Mission: Contribute to the prevention and cure of cancer
Image: Photo of the Moffitt Cancer Center.
Slide 31
A Cancer Center’s Journey
- Journey began 10/2011:
- Expanded surveillance house-wide
- Established CAUTI Committee:
- Promote best practice re: Foley use & management
- Reduce utilization by 20%
- Reduce CAUTI rates by 10%
Slide 32
Identifying the Issue
- Analysis of data showed high utilization:
- Little comparative data specific for Cancer Centers
- ICU chosen as pilot unit:
- Trialed a daily needs assessment program
- Not a success!
- Partnered with industry to perform Foley Management Point Prevalence Study
Slide 33
What We Found
- Results were surprising!
- Foley management is an issue
- Back to the basics
- Engaged the unit managers:
- Education, education, education
- Audit what you expect
- Compliance increased
Slide 34
Keeping Our Eyes on the Goal
- Journey continues: 05/2012:
- FHA HEN Project introduced
- Moffitt joined & submitted house-wide data
- Adopted On the CUSP: Stop CAUTI
- FHA HEN Project introduced
- CAUTI Rates added to Nursing Unit Dashboards
- Case reviews of each CAUTI
- Unit audits continued
Slide 35
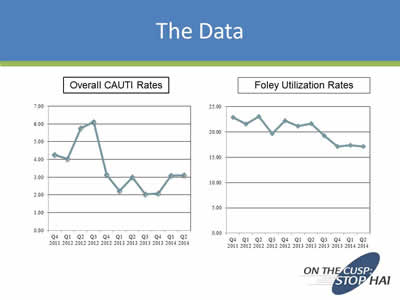
The Data
Images: Line charts titled Overall CAUTI Rates and Foley Utilization Rates. Both charts shown a downward trend from the 4th quarter of 2011 to the 2nd quarter of 2014.
Slide 36
Refocusing Efforts
- CAUTI rates plateaued:
- Foley manufacturer offered program to assess insertion technique
- Back to the basic basics!
- Results were surprising—again!
- Correct insertion technique observed in only 1 out of 10
- Assessed RN & Onc Tech
- Experienced & novice
Slide 37
Polling Question
Does your institution allow Nurse Techs/Nurse Aides to insert Foley?
- Yes
- No
Slide 38
The 4 E’s in Action
- Engagement:
- Presented the results to managers & staff
- Education:
- Utilized “Train the Trainer” model
- Execution:
- Combined new product rollout w/competency demonstration
- Industry involved in re-design of tray = engineered compliance
- Evaluation:
- Pending
Slide 39
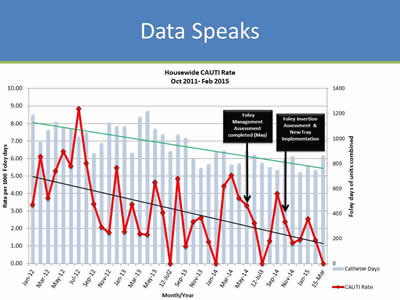
Data Speaks
Image: Screen show of line graph titled Housewise CAUTI Rate Oct 2011-Feb 2015. Text boxes point to 2 points: Foley Management Assessent completed (May 2013) and Foley Insertion Assessent & New Tray Implementation (Oct. 2015). The CAUTI rates trend downward to zero incidents in March 2015.
Slide 40
Learning & Sustaining
- Lessons Learned:
- Basics do need to be assessed and addressed
- Ongoing competency & audits necessary
- Industry helpful in patient care improvement
- Plans for Future & Sustainability:
- Perform follow-up evaluation
- Implement Nurse Driven Removal Protocol
Slide 41
Thank you!
Questions?
Slide 42
Funding
Prepared by the Health Research & Educational Trust of the American Hospital Association with contract funding provided by the Agency for Healthcare Research and Quality through the contract, “National Implementation of Comprehensive Unit-based Safety Program (CUSP) to Reduce Catheter-Associated Urinary Tract Infection (CAUTI), project number HHSA290201000025I/HHSA29032001T, Task Order #1.”



