CAUTI Sustainability: Embedding CAUTI Policies, Using Data to Monitor Proress and Hardwiring CUSP Principles
Slide Presentation
Slide 1
CAUTI Sustainability: Embedding CAUTI Policies, Using Data to Monitor Progress and Hardwiring CUSP Principles
Diane Byrum, RN, MSN, CCRN, CCNS, FCCM
Manager, Quality Implementation Programs
Society of Critical Care Medicine
William S. Miles, MD, FACS, FCCM, FAPWCA
Director of Surgical Critical Care and the Medical Director of the Surgical Trauma Intensive Care Unit
Carolinas Medical Center, Charlotte, NC
Ginger Dickens, MSN, RN, CNML, CCRN
Nurse Manager
Maury Regional Medical Center, Columbia, TN
Pat Posa RN, BSN, MSA, FAAN
System Performance Improvement Leader
Saint Joseph Mercy Hospital, Ann Arbor, MI
Images: Photos of the 4 presenters.
Slide 2
Learning Objectives
- Describe how to use data to change culture and sustain goals.
- Explain ways that CUSP concepts can be used and sustained.
- Identify components for successful change.
Slide 3
Sustaining Gains: Embedding CAUTI Policies
Diane Byrum RN, MSN, CCRN, CCNS, FCCM
Manager, Quality Implementation Programs
Society of Critical Care Medicine
Image: Photo of Diane Byrum.
Slide 4

Project Impact
Society of Critical Care Medicine
Project Dispatch is focused on patient-centered outcomes research and aims to provide clinicians with information on how to adapt and adopt successful interventions in their own ICU.
Images: Logos of Project Dispatch, AHRQ, and the Society of Critical Care Medicine are shown on bottom of slide.
Slide 5
Quality Health Care-
“the degree to which health services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge” (p. 1161)
Lorh KN N Engl J Med. 1990;332:1161-71.
Slide 6
Change Requires RESPECT
Speak respectfully of the past, realistically of the present and optimistically of the future….
Slide 7
Begin with the END in mind
- Remember – Quality issues are often process related, not people related
- Fix the process, fix the problem:
- Standardize, simplify
- Decrease reliance on individual decision-making
Slide 8
Lessons Learned = Sustaining the Gain
- Recognize that change takes time
|
Change takes time. The problem is that people stop to change when they don't see the result immediately. —Wilson Kanadi Image: boardofwisdom.com and logo. |
Slide 9
Lessons Learned = Sustaining the Gain
- Ensure administration is aware of your efforts and results
- Encourage and reward participation and problem identification
- Avoid complacency with success
com.pla.cen.cy
Spelled[kuh m-pley-suh n-see]
–noun, plural -cies
- a feeling of quiet pleasure or security, often while unaware of some potential danger, defect, or the like; self-satisfaction or smug satisfaction with an existing situation, condition, etc.
Slide 10
Lessons Learned = Sustaining the Gain
- Keep CAUTI project on the “front burner”
- Staff meetings, create healthy competition
- Jerri’s Story: https://www.youtube.com/watch?v=wl_aZto-K8Q
Image: After the first bullet, a photo of 2 electric burners, one fully heated red.
Slide 11
Lessons Learned = Sustaining the Gain
- Continue to work on staff competency (insertion and foley care techniques)
- Hard wire Foley education into all new employee education
Image: Photo of health professional practicing catheter insertion and foley care techniques.
Slide 12
Lessons Learned = Sustaining the Gain
- Set short term attainable goals
- Celebrate success – Create fun!!!
- Continue to engage the nay-sayers
Images: 2 posters. The right poster says "Celebrate what you've accomplished, but raise the bar a little higher each time you succeed." Mia Hamm. The bottom poster shows four hands holding little signs saying Ha!, Never, No, and Impossible.
Slide 13
Lessons Learned = Sustaining the Gain
- Treat a “CAUTI with respect – Learning from defects tool
Image: Sign post with the top sign saying Past and pointing to the word Mistake. Underneath is a sign saying NOW Lesson. The bottom sign says Future and points to the word Success.
Slide 14
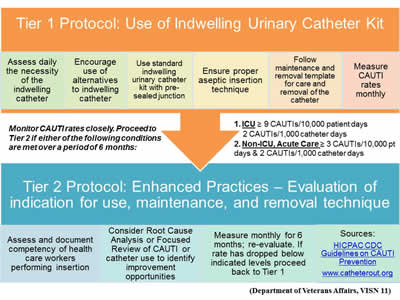
Image: Flowchart showing Tier 1 and Tier 2 Protocols for use of the indwelling urinary catheter kit and enhanced practices.
Slide 15

Lessons Learned = Sustaining the Gain
- Data drives practice and improvement….
Image: 3-dimensional graph with a large red line peaking with 3 cartoon images of smiling people.
Slide 16
Using Data for Sustainability CAUTI Collaborative
William S. Miles, MD, FACS, FCCM
Director of Surgical Critical Care and the Medical Director of the Surgical Trauma Intensive Care Unit
CO-Lead COHORT 9
Image: Photo of Dr. Miles.
Slide 17
The Power of Measuring Results
- If you do not measure results, you can not tell success from failure.
- If you can not see success, you can not reward it.
- If you can not reward success, you are probably rewarding failure.
- If you can not see success, you can not learn from it.
- If you can not recognize failure, you can not correct it.
- If you can demonstrate results, you can win public support.
Adapted from Osborne & Gaebler, 1992
Slide 18
Learning from Data
- We don’t all define a process in the same way.
- We all assume steps without spelling them out.
- We don’t all address a problem in the same way, and there are variations in our processes.
- Without using data and validation, we will not get the same results.
Slide 19
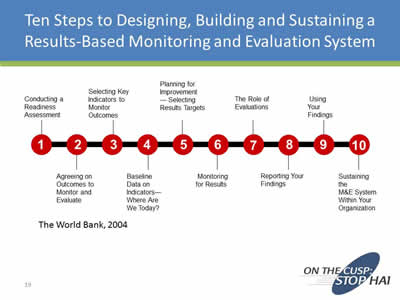
Ten Steps to Designing, Building and Sustaining a Results-Based Monitoring and Evaluation System
- Conducting a Readiness Assessment
- Agreeing on Outcomes to Monitor and Evaluate
- Selecting Key Indicators to Measure Outcomes
- Baseline Data on Indicators- Where Are We Today?
- Planning for Improvement - Selecting Results Targets
- Monitoring for Results
- The Role of Evaluations
- Reporting Your Findings
- Using Your Findings
- Sustaining the M&E System Within Your Organization
The World Bank, 2004
Slide 20
Ways to Use Data
Slide 21
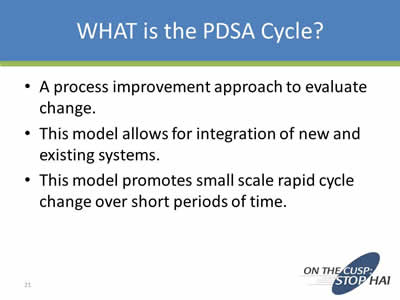
WHAT is the PDSA Cycle?
- A process improvement approach to evaluate change.
- This model allows for integration of new and existing systems.
- This model promotes small scale rapid cycle change over short periods of time.
Slide 22
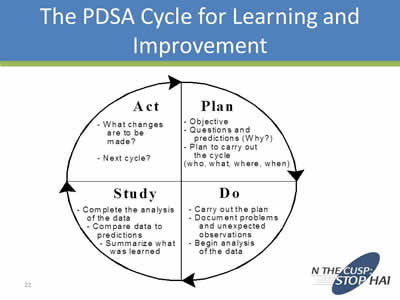
The PDSA Cycle for Learning and Improvement
Image: The PDSA Cycle.
Slide 23
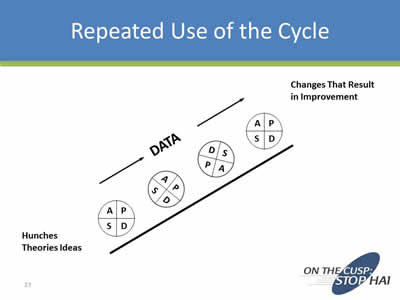
Repeated Use of the Cycle
Image: Drawing depicting circles of PDSA going up a hill. At the bottom is says Hunches Theories Ideas. Over the PDSA circles it has an arrow pointing up saying Data. At the top it says Changes That Result in Improvement.
Slide 24
Use the PDSA Cycle for:
- Testing or adapting a change
- Implementing an improvement
- Spreading the improvements to the rest of your organization
- Maintaining a process by reassessing and making it current
Slide 25
PDSA Cycles Must Be:
- Active:
- Quickly plan and make process changes
- Iterative:
- Cycle after cycle
- Learning:
- Take time to study effects of your actions
Slide 26
Root Cause Analysis
- A way of looking at unexpected events, data results, and outcomes to determine all of the underlying causes of the event and recommend changes that are likely to improve them.
- Data can be validated, vetted, and changes made to achieve outcomes
Slide 27
RCA Tools
- The 5 Whys?
- Appreciation
- Drill Downs
- Cause and Effect Diagrams (Fishbone Diagrams)
Slide 28
Success
“There are no secrets to success. It is the result of preparation, hard work, and learning from failure.”
General Colin L. Powell
Slide 29
Carrots and Sticks Methodology
- Base these carrots and sticks on your local hospital culture
- You know what drives your employees and staff
- Carrots: CAUTI-Carnival, CAUTI-Cash, Increased bonuses, etc.
- Sticks: Negative incentives, Peer Pressure, No bonus, etc.
- CMS Value Based Purchasing
Slide 30
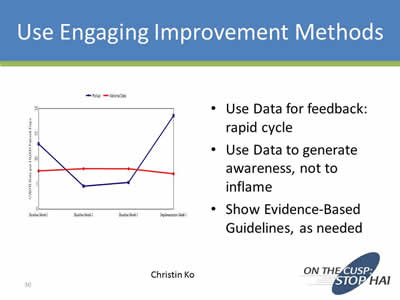
Use Engaging Improvement Methods
- Use Data for feedback: rapid cycle
- Use Data to generate awareness, not to inflame
- Show Evidence-Based Guidelines, as needed
Christin Ko
Image: Sample line chart showing CAUTI data.
Slide 31
Using Data for Sustainability
- Consider Cultural Assessment
- Present Data on CAUTI: Initially and Regularly
- Prevalence
- Morbidity
- Mortality
- Present the Business Case for CAUTI Prevention:
- CAUTI Cost Calculator
- LOS Reduction
- CMS Non-reimbursement Policy for HAI
Slide 32
Carrots and Sticks
Which one?
- Not as simple as choosing one or other
- Success depends on:
- Spin you put on incentives
- Having incentives real-time
- Continuing strategies your institution employs
- Carrots dressed as sticks may be most important
The Economist, “Designing Rewards: Carrots Dressed as Sticks,” print edition, January 16, 2010
Slide 33
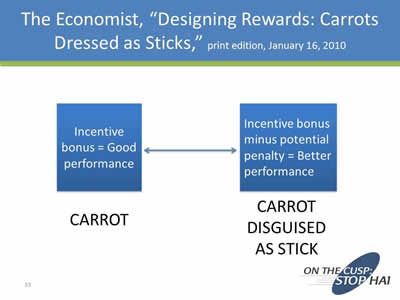
The Economist, “Designing Rewards: Carrots Dressed as Sticks,” print edition, January 16, 2010
Carrot: Incentive bonus = Good performance
Carrot Disguised as Stick: Incentive bonus minus potential penalty = Better performance
Slide 34
The Economist, “Designing Rewards: Carrots Dressed as Sticks,” print edition, January 16, 2010
- Clearly, both of these programs relied on carrots — but in one, the carrots were enticingly dangled to motivate positive efforts, while in the other, the carrots were “frozen,” and used to give employees the occasional whack when needed.
- What the researchers discovered was that “fear of loss was a better motivator than the prospect of gain.”
- Both approaches worked, but employees were more motivated to work harder to ensure that an award was not taken away.
- “Carrots...may work better if they can somehow be made to look like sticks.”
Slide 35
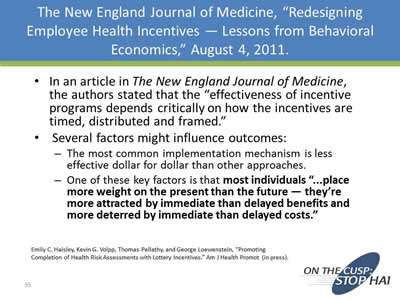
The New England Journal of Medicine, “Redesigning Employee Health Incentives — Lessons from Behavioral Economics,” August 4, 2011
- In an article in The New England Journal of Medicine, the authors stated that the “effectiveness of incentive programs depends critically on how the incentives are timed, distributed and framed.”
- Several factors might influence outcomes:
- The most common implementation mechanism is less effective dollar for dollar than other approaches.
- One of these key factors is that most individuals “...place more weight on the present than the future — they’re more attracted by immediate than delayed benefits and more deterred by immediate than delayed costs.”
Emily C. Haisley, Kevin G. Volpp, Thomas Pellathy, and George Loewenstein, “Promoting Completion of Health Risk Assessments with Lottery Incentives.” Am J Health Promot (in press).
Slide 36
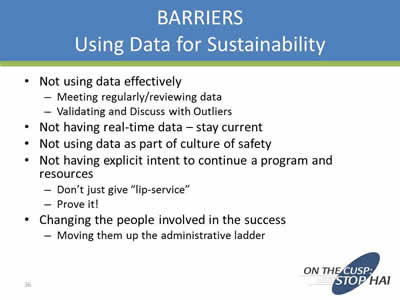
Barriers: Using Data for Sustainability
- Not using data effectively:
- Meeting regularly/reviewing data
- Validating and Discuss with Outliers
- Not having real-time data – stay current
- Not using data as part of culture of safety
- Not having explicit intent to continue a program and resources:
- Don’t just give “lip-service”
- Prove it!
- Changing the people involved in the success:
- Moving them up the administrative ladder
Slide 37
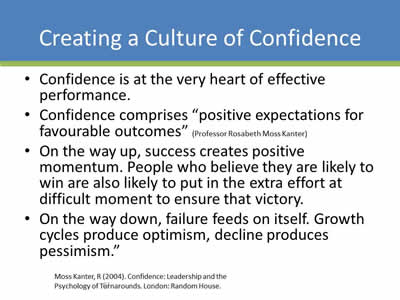
Creating a Culture of Confidence
- Confidence is at the very heart of effective performance.
- Confidence comprises “positive expectations for favourable outcomes” (Professor Rosabeth Moss Kanter)
- On the way up, success creates positive momentum. People who believe they are likely to win are also likely to put in the extra effort at difficult moment to ensure that victory.
- On the way down, failure feeds on itself. Growth cycles produce optimism, decline produces pessimism.”
Moss Kanter, R (2004). Confidence: Leadership and the Psychology of Turnarounds. London: Random House.
Slide 38
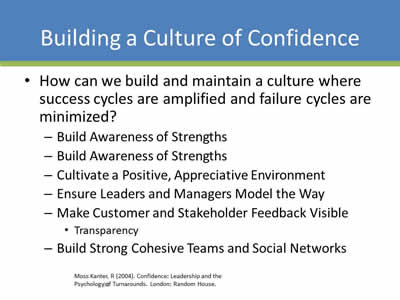
Building a Culture of Confidence
- How can we build and maintain a culture where success cycles are amplified and failure cycles are minimized?
- Build Awareness of Strengths
- Cultivate a Positive, Appreciative Environment
- Ensure Leaders and Managers Model the Way
- Make Customer and Stakeholder Feedback Visible:
- Transparency
- Build Strong Cohesive Teams and Social Networks
Moss Kanter, R (2004). Confidence: Leadership and the Psychology of Turnarounds. London: Random House.
Slide 39
Sustaining a Culture of Confidence
- Building a culture of confidence is largely about amplifying successes and strengths to ensure the ‘voices’ of possibility, optimism and self-belief drown out the ‘voices’ of self-doubt, negativity and pessimism.
- With the right mindset, approaches-using DATA and results real time, leaders can build accountability for the turnaround, focus on small ‘wins’ to start build confidence
- Inspires people to optimize their strengths and take initiative, accountability:
- Sustain a Culture of Confidence.
Slide 40
Successful Hospitals Examples
- Using validated resources:
- AHA/IHI collaboratives
- Adopting a culture of safety:
- AHRQ Culture of Safety Survey
- Take results seriously
- Educate and re-educate new/established hires
- Top Down/Down to Top Mentality:
- CEO to Environmental services to patients and families
Slide 41
Successful Hospitals Examples
- Process to evaluate, validate, publish, celebrate data:
- Know what works at your institution
- Make it a part of the culture/behavior
- Transparency – patients and families are part of committee
- Celebrate wins, publicly evaluate losses:
- Make your data and processes transparent
Slide 42

Quality Improvement is a Process, not an Event
Slide 43
Summary
- Use process to collect, evaluate, adapt, and publicize data
- Use real-time data/transparency
- Utilize specific data mining tools that work:
- Monitor and evaluate frequently
- Process of “Carrots and Sticks”
- Participate in AHA collaboratives and AHRQ resources to maximize effects
- Use your data to be accountable, transparent, and sustain your Culture of Confidence
Slide 44
Hospital Unit Story: Maury Regional Medical Center
Ginger Dickens, MSN, RN, CNML, CCRN
Nurse Manager
Maury Regional Medical Center Columbia, TN
Image: Photo of Ms. Dickens.
Slide 45
Maury Regional Medical Center Columbia, TN
- Largest hospital between Nashville, TN and Huntsville, AL
- 275 bed facility with a medical staff of more than 200 physicians and 2,000 employees
- Serves a region of more than a quarter of a million people in southern middle Tennessee
Maury Regional Health System
- Columbia
- Maury Regional Medical Center
- Family Health Group (100 providers)
- EMS Services
- Lewisburg
- Marshall Medical Center: 25 Beds
- Waynesboro
- Wayne Medical Center: 80 Beds
- EMS Services
- Hohenwald
- Lewis Health Center - Primary Care Clinic & Diagnostics open 14 hours per day
- EMS Services
- Spring Hill
- Imaging, Surgery Center, Radiation Oncology, Multi-Specialty Physician Clinics
- Pulaski
- Physical Medicine Services
Image: Photo of Maury Regional Medical Center.
Slide 46

Maury Regional Medical Center Columbia, TN
- MRMC is proud to have been recognized for its quality of care and operations
- Services include:
- Cancer Center
- Emergency Services
- Heart Center
- Neonatal Intensive Care
- Neurology and Neurosurgery
- Orthopedic Services
- Surgical Services
- Women’s Center
Slide 47

Quality of Care
- Recent recipient of the TNCPE 2014 Excellence Award
- 2015 – formally recognized as a “Planetree Designated®” Patient-Centered Hospital. It’s one of 28 hospitals in the U.S.. and the first in Tennessee.
Images: Logos of the Tennessee Center for Performance Excellence 2014 Excellence Award and the Planetree Designated hospital seal.
Slide 48

The Joint Commission
- Disease-Specific Care for Inpatient Diabetes
- Disease Specific Care for Joint Replacement - Hips
- Disease Specific Care for Joint Replacement – Knee
- Disease Specific Care for Sepsis
- Disease Specific Congestive Heart Failure
Image: Logo of Joint Commission National Quality Approval seal.
Slide 49
Critical Care at MRMC
- 24 beds of critical care on two floors
- One team of staff servicing all areas
- 24/7 Intensivist coverage
- NP 7 days per week
- All admissions require Intensivist consult
- 60% BSN or higher (39 BSN and 4 MSN)
- 47% CCRN Certified Nurses (34)
Image: Photo of a group of hospital staff.
Slide 50

Team Design
- Physician Champion
- Infection Prevention
- Frontline staff/Champions
- Clinical Educator
- Wound Care
- Supply Chain
- Senior Leadership/Administration
Slide 51
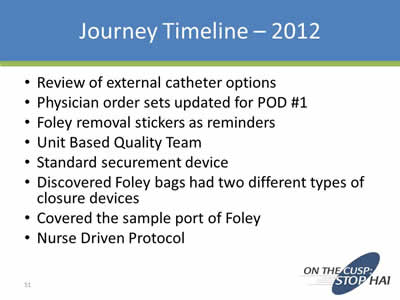
Journey Timeline - 2012
- Review of external catheter options
- Physician order sets updated for POD #1
- Foley removal stickers as reminders
- Unit Based Quality Team
- Standard securement device
- Discovered Foley bags had two different types of closure devices
- Covered the sample port of Foley
- Nurse Driven Protocol
Slide 52
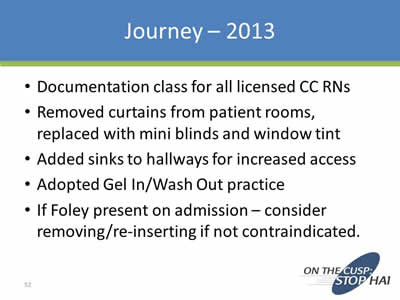
Journey - 2013
- Documentation class for all licensed CC RNs
- Removed curtains from patient rooms, replaced with mini blinds and window tint
- Added sinks to hallways for increased access
- Adopted Gel In/Wash Out practice
- If Foley present on admission – consider removing/re-inserting if not contraindicated.
Slide 53
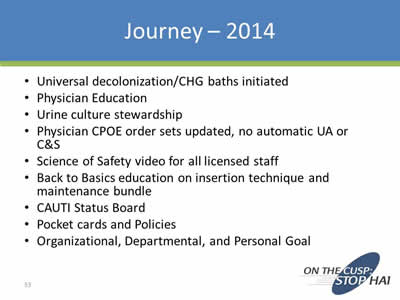
Journey - 2014
- Universal decolonization/CHG baths initiated
- Physician Education
- Urine culture stewardship
- Physician CPOE order sets updated, no automatic UA or C&S
- Science of Safety video for all licensed staff
- Back to Basics education on insertion technique and maintenance bundle
- CAUTI Status Board
- Pocket cards and Policies
- Organizational, Departmental, and Personal Goal
Slide 54
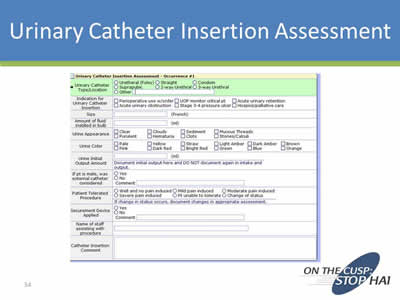
Urinary Catheter Insertion Assessment
Image: Screen show of a urinary catheter insertion assessment form.
Slide 55
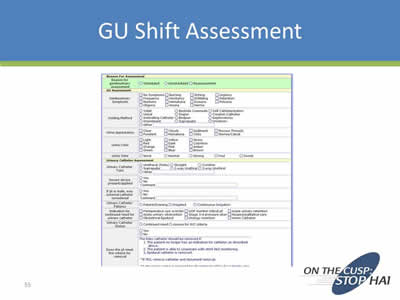
GU Shift Assessment
Image: Screen shot of GU Assessment form.
Slide 56
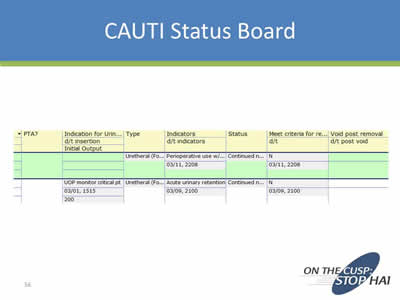
CAUTI Status Board
Image: Screen shot of CAUTI Status Board.
Slide 57
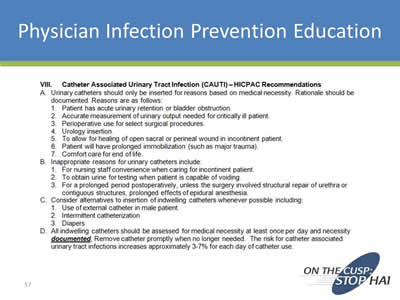
Physician Infection Prevention Education
Image: Screen shot of HICPAC Recommendations for CAUTI prevention.
Slide 58
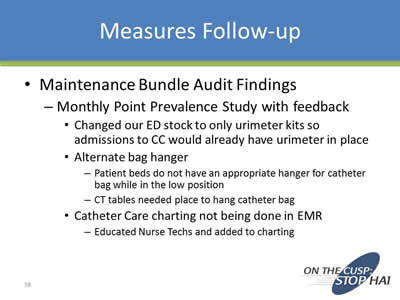
Measures Follow-up
- Maintenance Bundle Audit Findings
- Monthly Point Prevalence Study with feedback:
- Changed our ED stock to only urimeter kits so admissions to CC would already have urimeter in place
- Alternate bag hanger:
- Patient beds do not have an appropriate hanger for catheter bag while in the low position
- CT tables needed place to hang catheter bag
- Catheter Care charting not being done in EMR:
- Educated Nurse Techs and added to charting
- Monthly Point Prevalence Study with feedback:
Slide 59
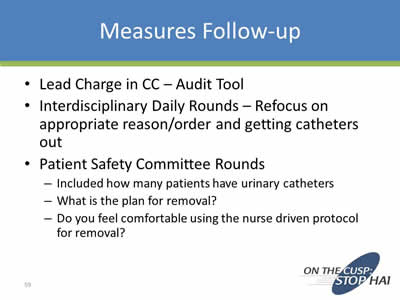
Measures Follow-up
- Lead Charge in CC – Audit Tool
- Interdisciplinary Daily Rounds – Refocus on appropriate reason/order and getting catheters out
- Patient Safety Committee Rounds:
- Included how many patients have urinary catheters
- What is the plan for removal?
- Do you feel comfortable using the nurse driven protocol for removal?
Slide 60
Nurse Driven Removal Protocol
- 2014 – tightened the indications for insertion, maintenance, and removal to strictly mirror the 2009 HICPAC guidelines
- With rounding learned some staff were not comfortable using protocol for removal without physician’s order:
- Have to keep checking back with, educating staff\
- Lead charge nurses conduct audit nightly
- Made the decision to replace any catheter that comes into critical care with seal broken
Slide 61
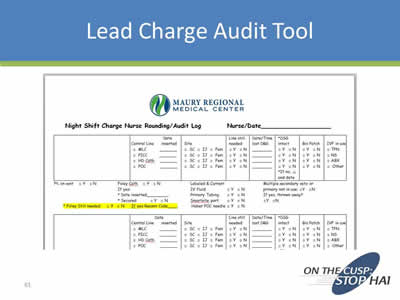
Lead Charge Audit Tool
Image: Screen shot of the top of a Night Shift Charge Nurse Rounding/Audit Log
Slide 62

Critical Care Interdisciplinary Rounding Tool
Image: Screen shot of the Critical Care Multidisciplinary Round Goals form.
Slide 63
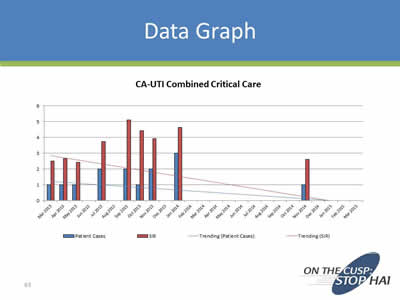
Data Graph
Image: Bar chart titled "CA-UTI Combined Critical Care. It shows a downward trend in cases from March 2013 to November 2014.
Slide 64

Celebrate Success!
- Mark the milestones
- Newsletters
- Unit Meetings
- Management Team Recognition
Slide 65
What Happens When a CAUTI Occurs?
- Event Analysis
- Team notification – Nurse Manager, Medical Director, and Frontline staff notification – email and huddle
- Infection Prevention Council report out
Slide 66
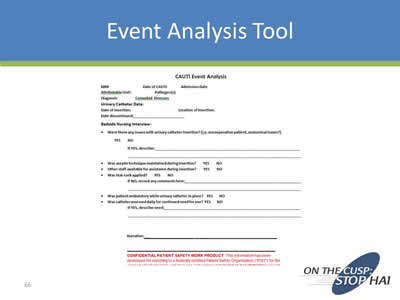
Event Analysis Tool
Image: Screen shot of a CAUTI Event Analysis form.
Slide 67
Reporting
- Scorecard – Zero CAUTI is goal
- Critical Care Committee
- Patient Safety Council
- Quality Council
- Senior Leader and Administrative Support
Slide 68
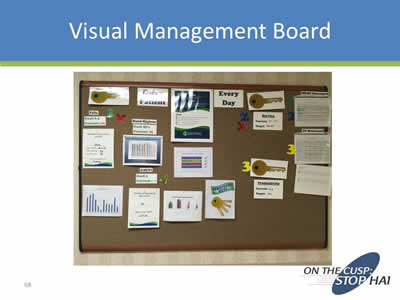
Visual Management Board
Image: Photo of a bulletin board with milestones and goals on it for CAUTI prevention.
Slide 69
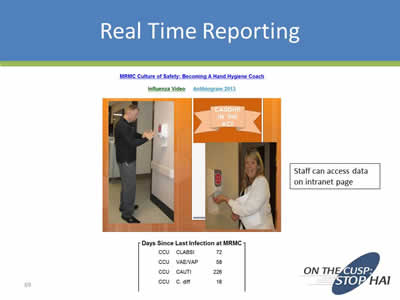
Real Time Reporting
Images: Photos of staff using the automatic hand cleaning dispenser. Next to one of the staff members it says "Caught in the Act". Below the photos is a table showing by department how many days since the last infection was reported.
Slide 70
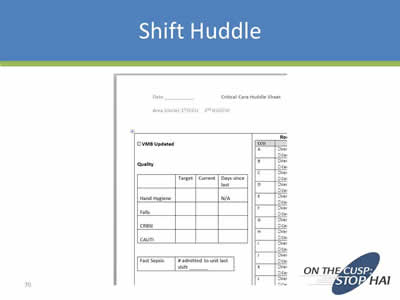
Shift Huddle
Image: Screen shot of a Critical Care Huddle Sheet form.
Slide 71
CUSP Initiative Takeaways
- Team formation/engagement
- Have senior leadership support
- Understand safety as a system design
- Process review – educate and execute
- Learn from what goes well and what does not
- Communicate
Slide 72
Succession Planning
- This is not a project – it is who we are
- Onboarding new staff
- Common Goal nurtures/enhances MD and RN relationships
- Senior Leader Quote – Wish we had done it sooner!
Slide 73
Sustaining CUSP
Pat Posa RN, BSN, MSA, FAAN
System Performance Improvement Leader
Saint Joseph Mercy Hospital
Ann Arbor, Michigan
patposa@gmail.com
Image: Photo of Pat Posa.
Slide 74
Sustaining CUSP
- Sustaining CUSP takes work and your team should expect to face challenges. The struggles often come because the team has lost sight of the steps of CUSP.
Slide 75
The Comprehensive Unit-based Safety Program (CUSP)
- Educate staff on the science of safety
- Identify defects
- Partner with the Senior Executive
- Learn from defects
- Improve teamwork and communication
Slide 76
How is CUSP Different?
- CUSP identifies problem areas:
- What staff think are impeding patient care vs. what managers/directors think are priority areas
- CUSP improvement tools are designed for bedside caregivers – easy for busy staff to use:
- Unit drives its own quality
- Lean/Six Sigma/CQI – focus more on streamlining the process than identifying the problem areas
- CUSP can complement other quality improvement methods – must use multiple tools!
Slide 77
Integrate & Coordinate With Other Efforts
Images: Logos of other patient safety programs including Six Sigma, Lean, TeamSTEPPS, PDSA, On the CUSP: Stop HAI, and Just Culture.
Slide 78
Basic Principles of Safe Design
- Standardize
- Create independent checks for key process
- Learn from mistakes
Slide 79
Basic Principles of Safe Design
Assess whether your unit continues to practice safe design principles
- Have your CUSP team name the 3 principles of safe design and write down an example of how you or your team has applied each of these principles.
Slide 80
Identifying Defects: Defects Can Come From Many Different Sources
- Staff feedback
- Event reporting
- Quality and safety measures
- Gaps in application of the evidence
- Staff Safety Assessment survey
- How will the next patient be harmed?
- What steps can you do to prevent this harm?
- By either preventing the mistake, making the mistake visible or mitigating the harm
Talk about administering the SSA survey every 6 months to 1 year
- Great tool to help staff own patient safety
Keep track of the safety issues identified and status of resolution
Image: Screen shot of the Armstrong Institute CUSP Tool Science of Safety Issues form.
Slide 81
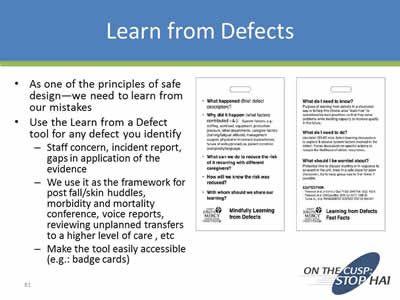
Learn from Defects
- As one of the principles of safe design—we need to learn from our mistakes
- Use the Learn from a Defect tool for any defect you identify:
- Staff concern, incident report, gaps in application of the evidence
- We use it as the framework for post fall/skin huddles, morbidity and mortality conference, voice reports, reviewing unplanned transfers to a higher level of care, etc.
- Make the tool easily accessible (e.g...: badge cards)
Images: Screen shots of 2 information sheets from Saint Joseph Mercy Hospital. One is titled "Mindfully Learning from Defects" and the other "Learning from Defects Fast Facts".
Slide 82
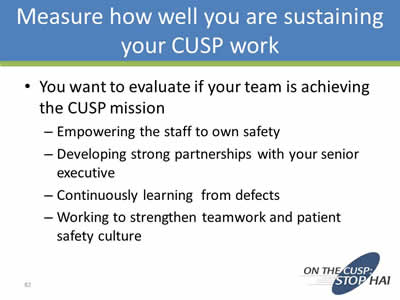
Measure How Well You Are Sustaining Your CUSP Work
- You want to evaluate if your team is achieving the CUSP mission:
- Empowering the staff to own safety
- Developing strong partnerships with your senior executive
- Continuously learning from defects
- Working to strengthen teamwork and patient safety culture
Slide 83
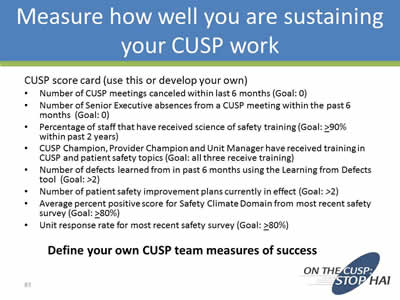
Measure How Well You Are Sustaining Your CUSP Work
CUSP score card (use this or develop your own)
- Number of CUSP meetings canceled within last 6 months (Goal: 0)
- Number of Senior Executive absences from a CUSP meeting within the past 6 months (Goal: 0)
- Percentage of staff that have received science of safety training (Goal: >90% within past 2 years)
- CUSP Champion, Provider Champion and Unit Manager have received training in CUSP and patient safety topics (Goal: all three receive training)
- Number of defects learned from in past 6 months using the Learning from Defects tool (Goal: >2)
- Number of patient safety improvement plans currently in effect (Goal: >2)
- Average percent positive score for Safety Climate Domain from most recent safety survey (Goal: >80%)
- Unit response rate for most recent safety survey (Goal: >80%)
Define your own CUSP team measures of success
Slide 84
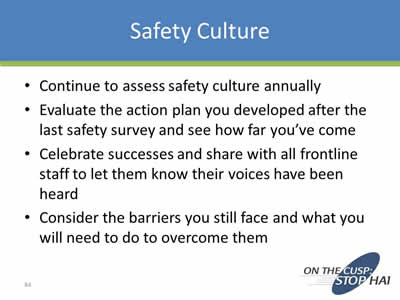
Safety Culture
- Continue to assess safety culture annually
- Evaluate the action plan you developed after the last safety survey and see how far you’ve come
- Celebrate successes and share with all frontline staff to let them know their voices have been heard
- Consider the barriers you still face and what you will need to do to overcome them
Slide 85
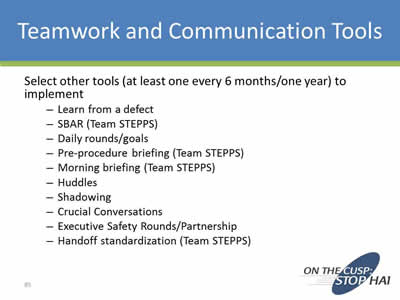
Teamwork and Communication Tools
Select other tools (at least one every 6 months/one year) to implement:
- Learn from a defect
- SBAR (Team STEPPS)
- Daily rounds/goals
- Pre-procedure briefing (Team STEPPS)
- Morning briefing (Team STEPPS)
- Huddles
- Shadowing
- Crucial Conversations
- Executive Safety Rounds/Partnership
- Handoff standardization (Team STEPPS)
Slide 86
Other Strategies to Sustain CUSP
- Make science of safety training a part of orientation for all new staff regardless of role (Goal: 90% of all staff trained every two years)
- Advertise CUSP meetings widely and open meetings to new team members
- Encourage new staff to take an active role in CUSP
- Hold periodic meetings for new staff to provide an overview of the CUSP approach and the important role of frontline staff
- Regularly ask staff to identify defects (can use SSA, part of Executive safety rounds)
- Make the CUSP initiative visible (e.g..: through bulletin boards, newsletters, review of results from LFD, etc.)
- Expand the CUSP team/concepts to other units
Slide 87
Thank you!
Questions?
Slide 88
Funding
Prepared by the Health Research & Educational Trust of the American Hospital Association with contract funding provided by the Agency for Healthcare Research and Quality through the contract, “National Implementation of Comprehensive Unit-based Safety Program (CUSP) to Reduce Catheter-Associated Urinary Tract Infection (CAUTI), project number HHSA290201000025I/HHSA29032001T, Task Order #1.”
Return to CAUTI Toolkit Information for Specialty Audiences



