Engaging the Nurse, Physician, Patient/Family, CUSP- Learn From Defects
Slide Presentation
Slide 1
Engaging The Nurse, Physician, Patient/Family; CUSP – Learn from Defects
Jenny Tuttle, RN, MSNEd, CNRN
Clinical Nurse Leader
Neuro/Medical/Surgical ICU
Tucson Medical Center
Tucson, Arizona
Christin Ko, MD, MBA, SFHM, FACP
Assistant Professor
Feinberg School of Medicine
Northwestern University
Chicago, IL
Images: Photos of the 2 presenters.
Slide 2
Sue Collier, MSN, RN, FABC
Clinical Content Development Lead
Health Research & Education Trust
American Hospital Association
Emily Pasola MSN, RN, CNL
Clinical Nurse Leader
Surgical Intensive Care Unit
Saint Joseph Mercy Hospital
Ann Arbor, Michigan
Images: Photos of the 2 presenters.
Slide 3
Learning Objectives
- Define nurse, physician, and patient and family engagement.
- Describe the benefits and examples of engaging key team members as partners in reducing CAUTI in the ICU
- Identify the key elements of the CUSP: Learning From Defects process and how it can be used to improve performance
- Identify the scope, and challenges and solutions around physician engagement
Slide 4
Case Study
- 08/02/12 – Ms. C is a 66 y.o. who is in the OR for an exploratory lap. An indwelling urinary catheter was inserted in OR. Ms. C was transferred to ICU post-op. Nurse OR gave report to Nurse ICU.
- 08/03/12 – Ms. C is stable. The indwelling urinary catheter is still in place. Ms. C’s son has been with her since surgery, but he has not been included in any rounds with the nurses or physicians, because they occur outside of visiting hours. Daily rounds and morning huddle did not include assessment of the indwelling catheter.
Slide 5
Case Study
- 08/04/12 – Ms. C is febrile (38.9°C) and complains of diffuse abdominal pain. WBC has increased to 19,000. She has cloudy, foul-smelling urine and urinalysis shows 2+ protein, + nitrite, 2+ leukocyte esterase, WBC – 15/mm3 of unspun urine and 3+ bacteria. Urine culture was 10,000 CFU/ml E. coli. The abdominal pain seems localized to the surgical area.
- 8/04/12 – Ms. C is diagnosed with a CAUTI by the attending physician. The physician ordered a course of antibiotics. During morning huddle the infection preventionist reviewed the prevalence of urinary catheter use. Several staff indicated that a higher prevalence of UTI in the ICU is not unusual. When Ms. C’s son was at the bedside during visiting hours, he stated he was angry and concerned that his mother has an infection.
Slide 6
How Might Nurse, Physician, and Patient/Family Engagement Impact This Scenario?
Consider these three elements as we discuss engagement of each role (nurse, physician, patient/family):
- Concerns/fears: What might be some unique issues or concerns each role has relative to UC?
- Skills/Knowledge (e.g. communication skills, information/education): What do they need to know to adopt new practices and to be confident it’s the right thing?
- System support (policies, protocols, check lists, teamwork): What can the system do to promote evidence-based practice and a culture of safety?
Slide 7
Reducing CAUTIs: Nurse Engagement in the ICU
Jenny Tuttle, RN, MSNEd, CNRN
Clinical Nurse Leader
Neuro/Medical/Surgical ICU
Tucson Medical Center
Tucson, Arizona
Image: Photo of the Tucson Medical Center sign.
Slide 8
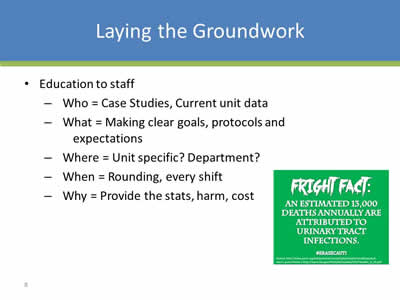
Laying the Groundwork
- Education to staff:
- Who = Case Studies, Current unit data
- What = Making clear goals, protocols and expectations
- Where = Unit specific? Department?
- When = Rounding, every shift
- Why = Provide the stats, harm, cost
Image: Poster which says "Fright Fact: An estimated 13,000 deaths annually are attributed to urinary tract infections. #ERASECAUTI".
Slide 9
Providing the Tools to Succeed
- Review of current supplies
- Listen and identify opportunities to make workflow easier:
- Extra techs?
- Give staff an opportunity to be apart of the decision making.
- It may cost more in supplies but every CAUTI avoided is worth it
- Reminders – flyers, t-shirts, slogan, computer based assessments
Image: Poster which is titled: "Don't Be Naughty! Prevent CAUTI!".
Slide 10
Making Staff Accountable
- Are they following your hospital based guidelines?
- Auditing/survey – asking open questions
- Nursing based - Urinary insertion/removal protocol
- Providing current data:
- Bulletin board
- Unit newsletter
Slide 11
Acknowledge the Success
- Rewards:
- Even small rewards stand out
- “High five”
- Sunflower” (North Shore University Hospital, NY)
Images: Photos of four health professionals who were acknowledged for their success. On the right side of the slide is a smiley face with two hands in a "thumbs up" position with the words "Great Job!" above it.
Slide 12

Attaining Physician Engagement: From the Medical Executive to the Individual Physician
Christin H. Ko, MD, MBA
Image: Photo of two men shaking hands - one in a formal suit, and the other wearing a lab coat.
Slide 13
Agenda
- Definition of Physician Engagement
- Scope of Physician Engagement
- Challenges around Physician Engagement
- Solutions: General and Specific
- Putting It All Together: Scenario-Solution Summary
Slide 14
Definition of Physician Engagement
- An intentional and deliberate process
- To bring physicians and other stakeholders together
- To address problems and continuously improve care and the patient experience
Image: Photo of a hospital staff meeting.
Slide 15
What it Looks and Feels Like
- Invest their Time
- Curious
- Enthusiastic
- Contribute
- Influence Others
Adapted from J. Silversin
Slide 16
Why Does It Matter?
Evidence Links Physician Engagement to:
- Better Outcomes
- Greater Impact on Quality and Safety
- Dickinson H et al. Engaging Doctors in Leadership: Review of the literature. University of Birmingham 2008
- Reinertsen et al. Engaging Physicians in a Shared Quality Agenda. IHI Innovation Series White Paper. Cambridge, MA IHI 2007
- Ham C et al. Engaging Doctors in Leadership: What Can We Learn from International Experience and Research Evidence? University of Birmingham 2008
Slide 17
Scope of Physician Engagement
Slide 18
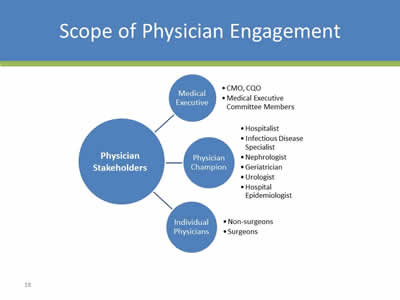
Scope of Physician Engagement
Image: This is a diagram which shows the relationship between physician stakeholders including medical executives, physician champions, and individual physicians. The different types of stakeholders are broken down into even more descriptions.
Slide 19
Challenges Around Physician Engagement
Slide 20
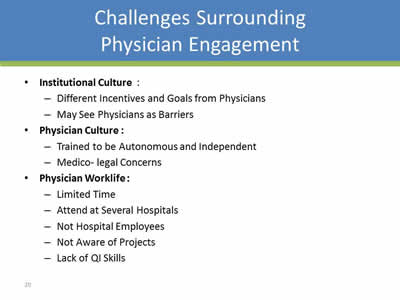
Challenges Surrounding Physician Engagement
- Institutional Culture:
- Different Incentives and Goals from Physicians
- May See Physicians as Barriers
- Physician Culture:
- Trained to be Autonomous and Independent
- Medico-legal Concerns
- Physician Worklife:
- Limited Time
- Attend at Several Hospitals
- Not Hospital Employees
- Not Aware of Projects
- Lack of QI Skills
Slide 21
Solutions: General
Slide 22
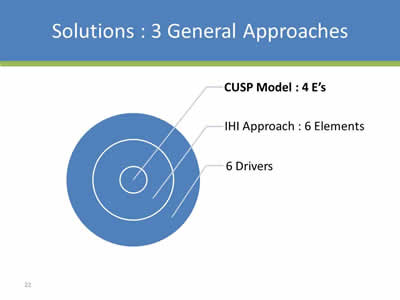
Solutions: 3 General Approaches
Image: Circle with 3 rings in it. The inner ring has text pointing to it that says "CUSP Model: 4E's", the middle ring is "IHI Approach: 6 Elements", and the outer ring is "6 Drivers".
Slide 23
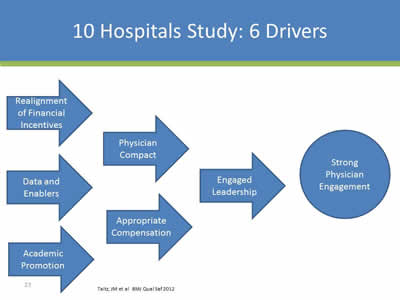
10 Hospitals Study: 6 Drivers
Image: Diagram showing the 6 drivers leading to strong physician engagement. The drivers are: Relalignment of Financial Incentives, Data and Enablers, Academic Promotion, Physician Compact, Appropriate Compensation, and Engaged Leadership.
Taitz, JM et al. BMJ Qual Saf 2012
Slide 24
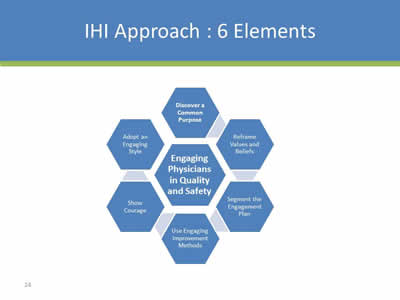
IHI Approach: 6 Elements
Image: Diagram showing the 6 elements of engaging physicians in quality and safety, which are: Discover a Common Purpose, Reframe Values and Beliefs, Segment the Engagement Plan, Use Engaging Improvement Methods, Show Courage, and Adopt an Engaging Style. In the center of the diagram it says "Engaging Physicians in Quality and Safety".
Slide 25

Discover A Common Purpose
Image: Venn diagram with a stethoscope in one oval, and a hospital symbol in the other. In the intersection is the text:
- Good Patient Outcomes
- Improved Efficiency
- Excellent Reputation
- Greater Cause
Slide 26
Reframe Values and Beliefs
View Physicians as Partners
Image: Photo of hands shaking - one in a doctor white coat, the other in a suit.
Slide 27
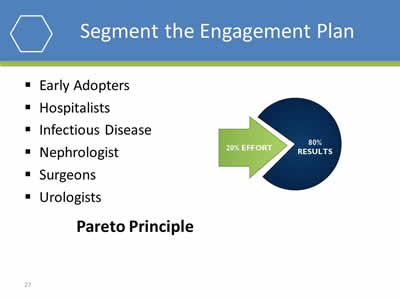
Segment the Engagement Plan
- Early Adopters
- Hospitalists
- Infectious Disease
- Nephrologist
- Surgeons
- Urologists
Pareto Principle
Image: Diagram showing that 20% effort leads to 80% better results.
Slide 28
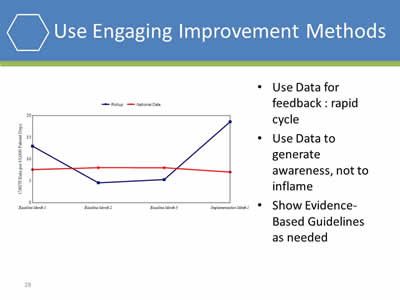
Use Engaging Improvement Methods
- Use Data for feedback: rapid cycle
- Use Data to generate awareness, not to inflame
- Show Evidence-Based Guidelines as needed
Image: Line graph showing theoretical results in implementing a CAUTI reduction program.
Slide 29
Show Courage
Image: Photo of a penguin holding a pair of cymbals on top of a sleeping polar bear.
Slide 30

Adopt an Engaging Style
- Involve Physicians from the Beginning
- Build Trust
- Communicate Often
- Value Their Time
Image: Photo of a group of smiling health professionals.
Slide 31
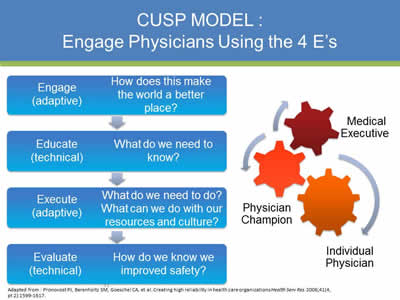
CUSP Model: Engage Physicians Using the 4 E’s
Engage (Adaptive): How does this make the world a better place?
↓
Educate (Technical): What do we need to know?
↓
Execute (Adaptive): What do we need to do? What can we do with our resources and culture?
↓
Evaluate (Technical): Hogw do we know we improved safety?
Adapted from: Pronovost PJ, Berenholtz SM, Goeschel CA, et al. Creating high reliability in health care organizations Health Serv Res 2006;41(4, pt 2):1599-1617.
Image: Three gears interacting. They are labeled: Medical Executive, Physician Champion, and Individual Physician.
Slide 32

Solutions: Specific
Slide 33
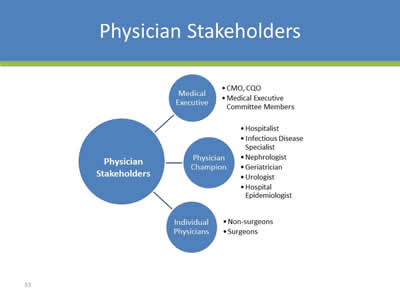
Physician Stakeholders
Image: This is a diagram explaining the scope of physican engagment. It describes the different types of physican stakeholders, including the medical executive, physician champion and individual physicians.
Slide 34
Medical Executives & Medical Executive Committee
- Consider Cultural Assessment
- Present Data on CAUTI: Initially and Regularly"
- Prevalence
- Morbidity
- Mortality
- Present the Business Case for CAUTI Prevention:
- CAUTI Cost Calculator
- LOS Reduction
- CMS Non-reimbursement Policy for HAI
Slide 35
Physician Champion: Choosing One
- Respected Clinician
- Courageous and Sociable
- Good Communication Skills
- Motivated – Internal Engine
- Consider Hospitalists, Infectious Disease, Urologist, Nephrologist, Geriatrician, Hospital Epidemiologist
Slide 36
Physician Champion: Roles and Responsibilities
- Communicate to other physicians
- Education of medical staff about the appropriate indications for urinary catheter use
- Assist with development of processes
- Assists with implementation of technical and adaptive components
- Assist with physician barrier removal
- Urologist, infectious disease specialist, hospitalist, quality/patient safety officer or any physician interested in improving safety and quality
Fakih, Mohamad. Building a Team and Process to Reduce CAUTI Risk. On the CUSP: Stop CAUTI Cohort 5 Onboarding Call #1; 2012.
Slide 37
Physician Champion: Equipping and Supporting
- Provide Materials and Resources
- Provide Leadership Support
- Connect with Early Adopters and Supporters
- Have a Communication Plan
- Consider Incentives/Recognition/Reward
Slide 38
Sample Script
- “I understand you feel that way, Bob. The evidence isn’t perfect. But it never is, is it?
- And the leading minds - the CDC, AHRQ and the IDSA - have all recommended we make this change.
- I don’t think we’re going to reinvent science here at this hospital and I think we should adopt these changes.
- Sure, there might be risk in making the change but we’ve seen the evidence of the harm that’s occurring with our current approach.
- What is the risk to our patients of not making the changes?”
Adapted from IHI
Slide 39
Individual Physicians: General Physicians and Specialists
- Make it As Easy as Possible
- Involve Early in Decisions: Design and Plans
- Physician Champion Presentation at Staff Meetings
- Provide Data and Feedback
- Appeal to Professional Pride
- Engage Medical Leadership support, eg Chief of Staff
- Use Scripts to Engage
- Frame it: “WIIFM”
- One on One Education
- Listen Carefully
- Ask: “What will it take for you to Participate or Commit”
- Rewards/Recognition
Slide 40
Individual Physicians: Surgeons
A Chief of Staff and a Surgeon: “ Surgeons are very tribal… so what you need to do if you have something you think is a best practice at your hospital… you need to get….either the Chair of Surgery or some reasonable surgeon…If you come in and you’re an internist… into a group of surgeons…the first thing we’re going to do is say ‘Look, you’re not one of us’…the way to get buy-in from surgeons is you got to have a surgeon on your team”.
Saint et al. Joint Comm Journal Qual Safety 2009
Slide 41
What NOT to do……
- Use Inflammatory Language: Message Carefully
- Adopt “One Size Fits All” Mentality
- Use Only Educational Material/Meetings
- Give Up
Slide 42

Putting It All Together: Scenario – Solution Summary
Slide 43
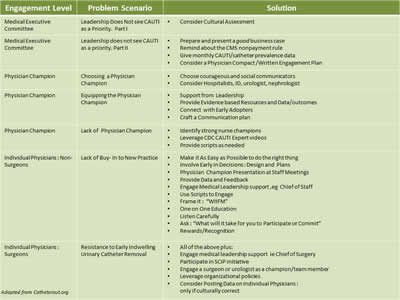
| Engagement Level | Problem Scenario | Solution |
|---|---|---|
| Medical Executive Committee | Leadership Does Not see CAUTI as a Priority. Part I |
|
| Medical Executive Committee | Leadership Does Not see CAUTI as a Priority. Part II |
|
| Physician Champion | Choosing a Physician Champion |
|
| Physician Champion | Equipping a Physician Champion |
|
| Individual Physicians: Non-Surgeons | Lack of Buy-In to New Practice |
|
| Individual Physicians: Non-Surgeons | Resistance to Early Indwelling Urinary Catheter Removal |
|
Adapted from Catheterout.org
Slide 44
Patient and Family Engagement
Sue Collier, RN, MSN, FABC
Clinical Content Development Lead
Health Research & Education Trust
American Hospital Association
Slide 45

Patient and Family Engagement (PFE)
Consider these three elements as we discuss engagement of the patient and their family:
- Concerns/fears: What are their unique concerns or issues?
- Skills/Knowledge: What do they need to know to be part of the team?
- System support: What can the system do to promote PFE?
Slide 46
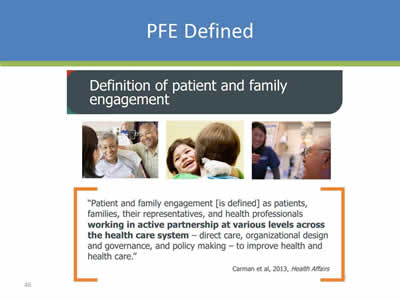
PFE Defined
Definition of patient and family engagement.
"Patient and family engagment is defined as patients, families and their representatives, and health professionals working in active partnership at various levels across the health care system - direct care, organizational design and governance, and policy making, to improve health and health care."
Carman et al., 2013, Health Affairs
Images: 3 photos of patients and families engaging with health professionals.
Slide 47
Image: Top of a journal article titled: "Evidence Boost: A Review of Research Highlighting How Patient Engagement Contributes to Improved Care". The author is G. Ross Baker, Ph.D. August 2014
Slide 48
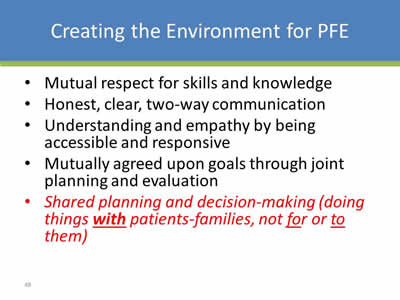
Creating the Environment for PFE
- Mutual respect for skills and knowledge
- Honest, clear, two-way communication
- Understanding and empathy by being accessible and responsive
- Mutually agreed upon goals through joint planning and evaluation
- Shared planning and decision-making (doing things with patients-families, not for or to them)
Slide 49
Examples of PFE Practices
- Including patient/family in rounds
- Supporting family presence
- Including patient/family in CAUTI prevention education
- Sharing patient stories in quality team meetings
- Developing Patient-family advisor roles and councils
- Encouraging Patient Advisors to serve on safety and quality performance improvement teams
Images: 3 photos of patients and families engaging with health professionals.
Slide 50
SSCM and AACN PFE Initiatives
SCCM
- Project Dispatch (Disseminating Patient-Centered Outcomes Research to Healthcare Professionals)
- THRIVE project (effects of ICU)
- ACCCM Statement on EOL Care in ICU
- Podcasts (Family Presence, Family-centered rounds, Integrating communication bundles)
AACN
- Scope & Standards for Acute & Critical Care Nursing Practice
- Practice Alert: Family Presence During Resuscitation and Invasive Procedures
- Clinical Practice Guidelines for Support of the Family in ICU
Images: Screen shots of publications from Society of Critical Care Medicine (SCCM) and American Association of Critical Care Nurses (AACN).
Slide 51
Your Organization's PFE Practices
- How does your organization demonstrate the principles and practices of patient and family engagement in infection prevention, especially CAUTI prevention?
- What is your organization’s long-term plan to advance patient- and family-centered care across all areas of patient safety, especially CAUTI prevention?
- Who is guiding your unit’s or organization’s efforts in this area?
Slide 52
Selected Resources For Engaging Patients and Families as Partners in Safety
AHRQ CUSP Toolkit, Patient Family Engagement. Retrieved from http://www.ahrq.gov/professionals/education/curriculum-tools/cusptoolkit/modules/patfamilyengagement/index.html.
Association for Professional in infection Control and Epidemiology. Patient safety resources for consumers. Retrieved from http://www.apic.org/For-Consumers/Patient-safety-resources.
Institute for Patient and Family Centered Care. Retrieved from http://www.ipfcc.org
Centers for Disease Control and Prevention. FAQs about Catheter-Associated Urinary Tract Infection. Retrieved from http://www.cdc.gov/HAI/ca_uti/uti.html
Carman KL, Dardess P, Maurer ME, Workman T, Ganachari D, Pathak-Sen E. A Roadmap for Patient and Family Engagement in Healthcare Practice and Research. September 2014. www.patientfamilyengagement.org and http://patientfamilyengagement.org/#sthash.ACZ81zY8.dpuf
Reinertsen JL, Bisognano M, Pugh MD. Seven Leadership Leverage Points for Organization-Level Improvement in Health Care (Second Edition). Cambridge, Massachusetts: Institute for Healthcare Improvement; 2008. Available on www.ihi.org
Guide to Patient and Family Engagement in Hospital Quality and Safety, Rockville, MD; Agency for Healthcare Research and Quality; May 2013, AHRQ Publication No. 13-0033. http://www.ahrq.gov/professionals/systems/hospital/engagingfamilies/index.html
Slide 53
Learn From a Defect
Emily Pasola MSN, RN, CNL
Clinical Nurse Leader
Surgical Intensive Care Unit
Saint Joseph Mercy Hospital
Ann Arbor, Michigan
Slide 54
Finding the Defects
- Staff feedback:
- Shift huddles, staff meetings
- Event reporting:
- Root Cause Analysis, hospital reporting system
- Quality and safety measures:
- Monthly data reports
- Recurring gaps
- Staff Safety Assessment survey
Anything that you do not want to happen again….
Slide 55
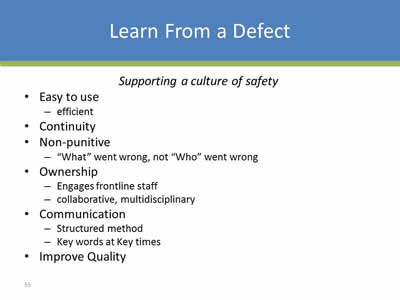
Learn From a Defect
Supporting a culture of safety
- Easy to use:
- Efficient
- Continuity
- Non-punitive:
- “What” went wrong, not “Who” went wrong
- Ownership:
- Engages frontline staff
- Collaborative, multidisciplinary
- Communication:
- Structured method
- Key words at Key times
- Improve Quality
Slide 56
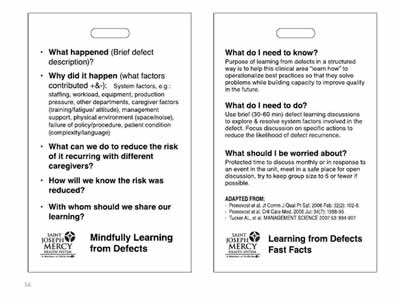
Images: 2 safety posters on learning from defects created by the Saint Joseph Mercy Health System.
Slide 57
Examples
Slide 58

Image: Sample incident report.
Slide 59
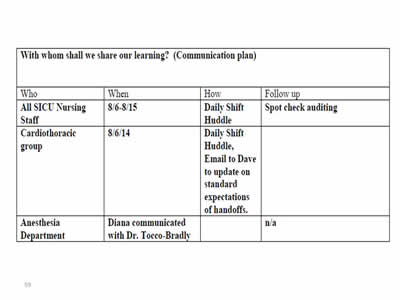
Image: Sample communication plan.
Slide 60
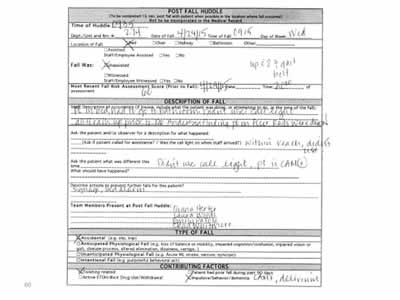
Image: Sample Post Fall Huddle report.
Slide 61
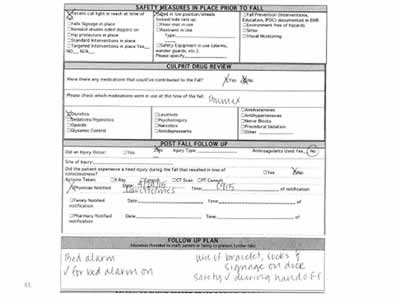
Image: Sample Post Fall Huddle report continued.
Slide 62

Next Steps:
- Assess your ICU’s level of engagement of nurses, physicians and patients/families:
- Are there opportunities for improvement?
- What are the barriers you are facing with regards to engagement?
- Utilize the learning from defects tool
- Review the concepts and tools referenced here today to help bolster your ICU’s level of physician/nurse/patient and family engagement
Slide 63
Thank you!
Questions
Slide 64
Funding
Prepared by the Health Research & Educational Trust of the American Hospital Association with contract funding provided by the Agency for Healthcare Research and Quality through the contract, “National Implementation of Comprehensive Unit-based Safety Program (CUSP) to Reduce Catheter-Associated Urinary Tract Infection (CAUTI), project number HHSA290201000025I/HHSA29032001T, Task Order #1.”



