Health Literacy and Patient and Family Engagement: Strategic Tools to Prevent CAUTI
Slide Presentation
Slide 1

Health Literacy and Patient and Family Engagement: Strategic Tools to Prevent CAUTI
Barbara Meyer Lucas, MD, MHSA
Project Consultant
Michigan Health & Hospital Association
Keystone Center for Patient Safety and Quality
Milisa Manojlovich, PhD, RN, CCRN
Associate Professor
Division of Nursing Business & Health Systems
University of Michigan School of Nursing
Slide 2
Learning Objectives
- Describe the importance of health literacy in CAUTI prevention
- Summarize ways to engage patients and families in CAUTI prevention
Slide 3
Part I: Health Literacy
Objectives:
- Define Health Literacy and Its Implications for Patient Care
- Understand Major Barriers to Health Literacy
- Review Strategies to Enhance Health Literacy
Slide 4
Defining Health Literacy
- Health Literacy is the ability to:
- Obtain,
- Understand, and
- Act on health information
- Dependent on clear communication between patient and the medical team
Slide 5
Why is Improved Medical Communication Important?
Big Picture:
Institute of Medicine Key Healthcare Dimensions:
- Patient Centered
- Timely
- Safe
- Effective
- Efficient
- Equitable
---*Crossing the Quality Chasm, 2001
Slide 6
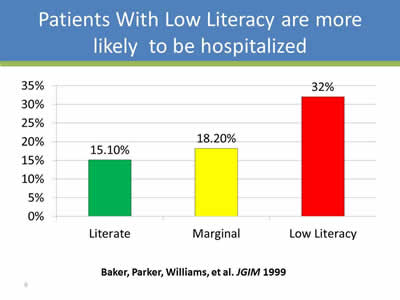
Patients With Low Literacy Are More Likely to be Hospitalized
Image: Bar chart showing hospitalization rates.
Literate: 15.1%
Marginal: 18.2%
Low Literacy: 32%
Baker, Parker, Williams, et al. JGIM 1999
Slide 7
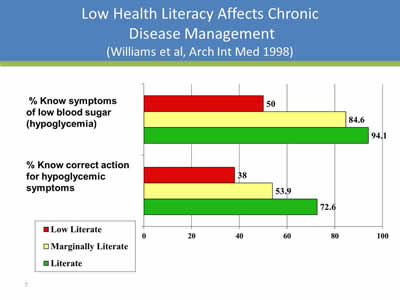
Low Health Literacy Affects Chronic Disease Management
(Williams et al, Arch Int Med 1998)
Image: Bar chart with the following data:
| Low Literate | Marginally Literate | Literate | |
|---|---|---|---|
| Percent know symptoms of low blood sugar (hypoglycemia) | 50 | 84.6 | 94.1 |
| Percent know correct action for hypoglycemic symptoms | 38 | 53.9 | 72.6 |
Slide 8
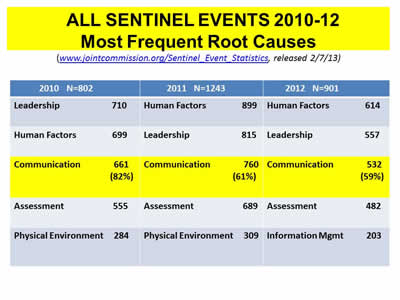
All Sentinel Events 2010-12: Most Frequent Root Causes
(www.jointcommission.org Sentinel_Event_Statistics, released 2/7/13)
| 2010 N=802 | 2011 N=1243 | 2012 N=901 |
| Leadership 710 | Human Factors 899 | Human Factors 614 |
| Human Factors 699 | Leadership 815 | Leadership 557 |
| Communication 661 (82%) | Communication 760 (61%) | Communication 532 (59%) |
| Assessment 555 | Assessment 689 | Assessment 482 |
| Physical Environment 284 | Physical Environment 309 | Information Management 203 |
Slide 9
Why is Improved Medical Education Important?
Applied to CAUTI Prevention:
- Improves patient understanding of catheters:
- Appropriate reasons for use
- Proper insertion and maintenance
- Why they need to come out as soon as possible
Slide 10
Why is Improved Medical Education Important?
Applied to CAUTI Prevention:
- Enhances patient-centered, compassionate care
- Improves patient safety by reducing infection risk
- Reduces prolonged hospital stays
Slide 11
Barriers to Health Literacy
- Barriers to health literacy are multifactorial:
- Complex healthcare system
- Patient factors (reading ability, age, emotions)
- Physician attitudes/communication skills
- Nursing issues (culture, time)
Slide 12
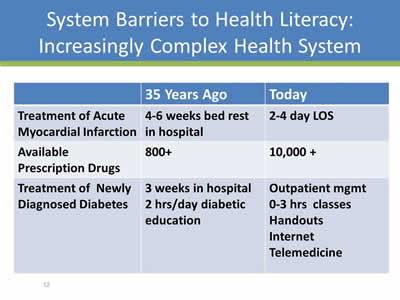
System Barriers to Health Literacy: Increasingly Complex Health System
| 35 Years Ago | Today | |
|---|---|---|
| Treatment of Acute Myocardial Infarction | 4-6 weeks bed rest in hospital | 2-4 day LOS |
| Available Prescription Drugs | 800+ | 10,000+ |
| Treatment of Newly Diagnosed Diabetes | 3 weeks in hospital 2 hrs/day diabetic education |
Outpatient management 0-3 hrs classes Handouts Internet Telemedicine |
Slide 13
System Barriers to Health Literacy
- Increasingly Complex Healthcare System
- Hospitalists, not your family physician
- More self-care and self-education expected
- Multiple handoffs / patient care unit cultural issues
Slide 14
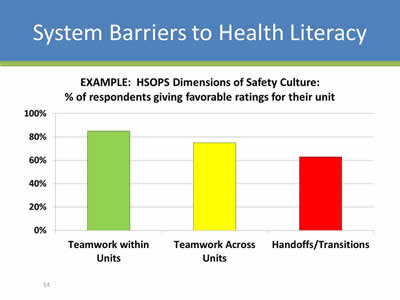
System Barriers to Health Literacy
Image: Bar chart titled Example: HSOPS Dimensions of Safety Culture: % of respondents giving favorable ratings for their unit.
Teamwork within Units: 82%
Teamwork across Units: 78%
Handoffs/Transitions: 62%
Slide 15
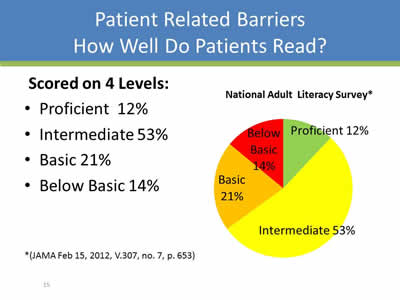
Patient Related Barriers: How Well Do Patients Read?
Scored on 4 Levels:
- Proficient 12%
- Intermediate 53%
- Basic 21%
- Below Basic 14%
Image: Bar chart showing the data in the bulleted list.
*(JAMA Feb 15, 2012, V.307, no. 7, p. 653)
Slide 16
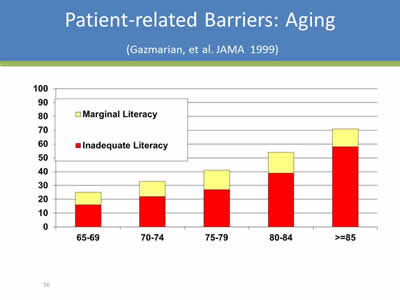
Patient-related Barriers: Aging
(Gazmarian, et al. JAMA 1999)
Image: Bar chart depicting the patient related barriers, with specific focus on Aging. Of the 65-69 age range, approximately 30% of patients are categorized as having marginal or inadequate literacy. The percentages goes up from there with the highest at 85+ years.
Slide 17
Patient-Related Barriers to Health Literacy: A Teachable Moment?
Image: Poster with the words "Medical Studies Indicate Most People Suffer A 68% Hearing Loss When Naked."
Slide 18
Clear Medical Communication: Physician Barriers
- Physician Attitudes
- Communication Skills
- Time
Image: Cartoon showing a doctor talking to a patient. The doctor says "I'm going to give you a mild sedative to counteract your really annoying questions."
Slide 19
Clear Medical Communication: Nursing Barriers
- Time
- Lack of Clarity of Daily Goals:
- (Including reason for the catheter!)
- Culture issues:
- Between physicians and nurses
- Between units
Slide 20
Strategies for Improving Medical Communication
System Level:
- Create a “Patient-Centered” Environment on Your Unit
- Assess all Patients for Literacy
As Individuals:
- Commit to Improving Your Communication Skills
Slide 21
System Approaches: Fostering a Patient-Centered Unit
Key Strategies:
- Adopt an attitude of helpfulness
- Respect patients’ privacy and dignity
- Convey a safe, non-judgmental attitude
Treat all patients as if they were your family!
Slide 22
System Approaches: Assess All Patients for Literacy
Key Strategies:
- Initial Patient Assessment:
- How far did they go in school?
- How do they best learn?
- Social history/support system
- Watch for subtle clues that they don’t read well
Slide 23
System Approaches: Assess All Patients for Literacy
Red Flags: Patients with literacy issues may:
- Have trouble completing forms
- Be unable to list their medications
- Be labeled “non-compliant” (missing appointments, tests, and referral visits)
- Seem angry or demanding
- Have difficulty explaining concerns or have no questions
Slide 24
For All Health Team Members: 4 Key Steps to Improve YOUR Skills
- Remember this is a dialogue:
- Sit at patient’s eye level
- Listen more than you speak!
- Allow time for questions
- Explain things clearly in plain language:
- Speak slowly
- Avoid jargon
Slide 25
For All Health Team Members: 4 Key Steps to Improve YOUR Skills
- Focus on key messages and repeat
Patients should leave you knowing 3 things:- What is wrong?
- What do I need to do about it?
- Why is it important that I follow this plan?
Slide 26
Example 1: One Key Message for a Patient with a Catheter
- What’s wrong?
- I need a catheter for a short time to drain the urine from my bladder.
- What do I need to do about it?
- Make sure that the staff and I always keep the drainage bag lower than my bladder.
- Why is it important that I follow these instructions?
- I can get a serious infection if the bag is not positioned correctly.
Slide 27
Example 2: One Key Message for a Patient with a Catheter
- What’s wrong?
- I need a catheter for a short time to drain the urine from my bladder.
- What do I need to do about it?
- Make sure that all staff clean their hands before and after touching my catheter.
- Why is it important that I follow these instructions?
- I can get a serious infection if staff don't clean their hands before caring for me.
Slide 28
For All Health Team Members: 4 Key Steps to Improve YOUR Skills
- Use a “teach back” or “show me” technique to check for understanding.
“Can you show me how you will manage your drainage bag when you go for a walk in the hall?
OR
“I want to be sure I explained everything clearly about your catheter, so can you please explain it back to me, so I can be sure I did a good job?”
Try not to ask, “Do you understand?”'
Slide 29
For Written Educational Materials: Patient-Friendly Guidelines
- For handouts:
- Simple words (1-2 syllables)
- Short sentences (4-6 words)
- Short paragraphs (2-3 sentences)
- No medical jargon
- Headings and bullets
- Lots of white space.
Slide 30
“Patient Friendly” Handouts: Additional Hints
- Show or draw only simple pictures
- Focus only on key points
- Emphasize what the patient should DO
- Minimize info about anatomy and physiology
- Be sensitive to cultural preferences.
Slide 31
Summary: Health Literacy
- As many as 35% of your patients may have health literacy issues
- Limits ability to obtain, understand, and act on health information
Slide 32
Summary: Health Literacy
- Impact of limited health literacy:
- Poor compliance with medical management
- Increased risk of:
- Poor outcomes/adverse events
- Infections/prolonged hospital stays
- Patient/family anxiety
Slide 33
Summary: Health Literacy and Patient Safety
- Barriers to health literacy are multifactorial:
- Complex healthcare system
- Patient factors (reading ability, age, emotional overlay)
- Physician attitudes/communication skills
- Nursing issues (culture, time)
Slide 34
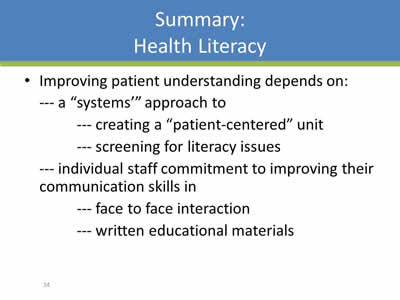
Summary: Health Literacy
- Improving patient understanding depends on:
- A “systems’” approach to:
- Creating a “patient-centered” unit
- Screening for literacy issues
- Individual staff commitment to improving their communication skills in:
- Face to face interaction
- Written educational materials
- A “systems’” approach to:
Slide 35
Part II: Engaging Patients and Families Strategies for Success
Objectives:
- Discuss how to engage patients and families in healthcare.
- Describe factors that influence patient and family participation in healthcare.
- Use strategies to educate patients and family members about catheter harms.
Slide 36
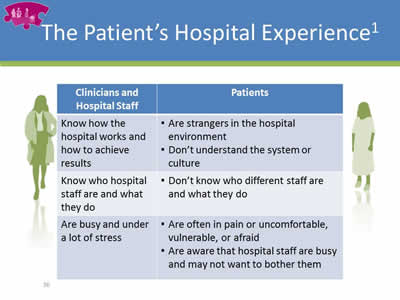
The Patient’s Hospital Experience1
| Clinicians and Hospital Staff | Patients |
|---|---|
| Know how the hospital works and how to achieve results |
|
| Know who hospital staff are and what they do |
|
| Are busy and under a lot of stress |
|
Slide 37
What is Patient/Family Engagement?2
Involves “…collaborating with patients and families of all ages, at all levels of care and in all health care settings…acknowledges that families, however they are defined, are essential to patients’ health and well-being…”
Slide 38
Patient/Family Engagement
Involves patients and family as:
- Members of the health care team
- Advisors who work with clinicians and leaders to improve policies and procedures
Slide 39
How to Engage Patients and Families1
When you enter the room:
- Read chart before stepping in.
- Make eye contact with the patient.
- Introduce yourself by name and role.
- Introduce new people in room by name, role, and what they will do.
Slide 40

How to Engage Patients & Families
When you first assess the patient:
- Ask how the patient prefers to be addressed
- Identify family that should be partners in their care
- Highlight main points of communication tools
- Invite the patient and family to use the white board to “talk” with clinicians
Slide 41
How to Engage Patients and Families1 (continued)
Ask about and listen to the patient and family’s needs and concerns:
- Use open-ended questions
- Listen to, respect, and act on what the patient and family say
- Help patients articulate their concerns when needed
- Obtain communication resources if the adviser or family member cannot understand you (i.e., translator)
Slide 42
How to Engage Patients and Families1 (continued)
Help the patient and family understand the diagnosis, condition, and next steps in their care:
- Give timely and complete information—take every opportunity to educate patient and family
- Use plain language
- Invite the patient or family to take notes
Slide 43
Engagement as a Strategy to Prevent CAUTI
- The past few slides have offered pointers on how to increase patient engagement in general.
- Now we’re going to zero in on patient and family engagement as a way to prevent CAUTI.
Slide 44
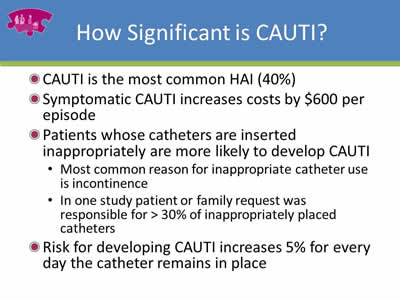
How Significant is CAUTI?
- CAUTI is the most common HAI (40%)
- Symptomatic CAUTI increases costs by $600 per episode
- Patients whose catheters are inserted inappropriately are more likely to develop CAUTI:
- Most common reason for inappropriate catheter use is incontinence
- In one study patient or family request was responsible for >30% of inappropriately placed catheters
- Risk for developing CAUTI increases 5% for every day the catheter remains in place
Slide 45
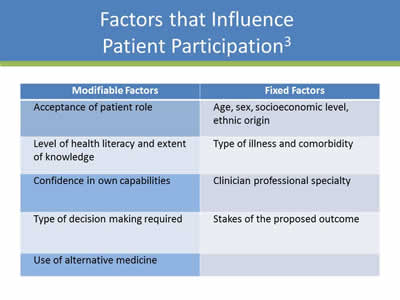
Factors that Influence Patient Participation3
| Modifiable Factors | Fixed Factors |
|---|---|
| Acceptance of patient role | Age, sex, socioeconomic level, ethnic origin |
| Level of health literacy and extent of knowledge | Type of illness and comorbidity |
| Confidence in own capabilities | Clinician professional specialty |
| Type of decision making required | Stakes of the proposed outcome |
| Use of alternative medicine |
Slide 46
Education Strategies
- Assess what patients/families already know about catheters.
- Assess readiness to learn.
- Ask how patient/family prefers to receive information (e.g., video, pamphlet).
- One-on-one versus group education.
Slide 47
Additional Education Strategies
- Take care of pain control, toileting, and other needs first.
- Make environment as conducive to learning as possible (e.g., turn TV off).
- Provide materials at 4th grade reading level.
- “Chunk” information into manageable pieces, and provide one “chunk” at a time.
Slide 48
A Valuable Resource
- Catheterout.org: a website developed as part of an NIH funded study co-led by Drs. Sarah Krein and Sanjay Saint
- Helpful information for clinicians and patients
http://catheterout.org/?q=patient-family-ed
Slide 49
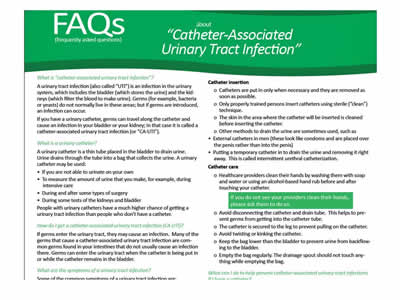
Image: Screen shot of a SHEA CAUTI Prevention flyer called FAQs about "Catheter-Associated Urinary Tract Infection".
Slide 50
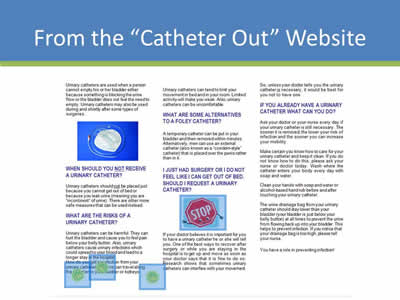
From the “Catheter Out” Website
Image: Screen shot of patient brochure found on http://www.catheterout.org website.
Slide 51
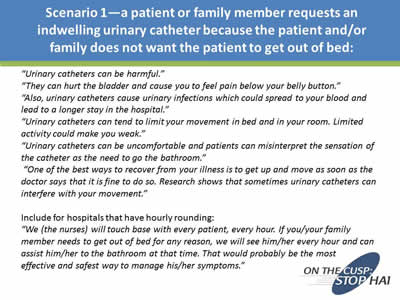
Scenario 1—a patient or family member requests an indwelling urinary catheter because the patient and/or family does not want the patient to get out of bed:
“Urinary catheters can be harmful.”
“They can hurt the bladder and cause you to feel pain below your belly button.”
“Also, urinary catheters cause urinary infections which could spread to your blood and lead to a longer stay in the hospital.”
“Urinary catheters can tend to limit your movement in bed and in your room. Limited activity could make you weak.”
“Urinary catheters can be uncomfortable and patients can misinterpret the sensation of the catheter as the need to go the bathroom.”
“One of the best ways to recover from your illness is to get up and move as soon as the doctor says that it is fine to do so. Research shows that sometimes urinary catheters can interfere with your movement.”
Include for hospitals that have hourly rounding:
“We (the nurses) will touch base with every patient, every hour. If you/your family member needs to get out of bed for any reason, we will see him/her every hour and can assist him/her to the bathroom at that time. That would probably be the most effective and safest way to manage his/her symptoms.”
Slide 52
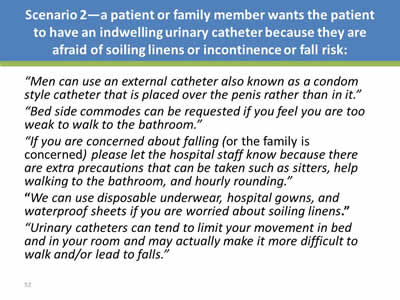
Scenario 2—a patient or family member wants the patient to have an indwelling urinary catheter because they are afraid of soiling linens or incontinence or fall risk:
“Men can use an external catheter also known as a condom style catheter that is placed over the penis rather than in it.”
“Bed side commodes can be requested if you feel you are too weak to walk to the bathroom.”
“If you are concerned about falling (or the family is concerned) please let the hospital staff know because there are extra precautions that can be taken such as sitters, help walking to the bathroom, and hourly rounding.”
“We can use disposable underwear, hospital gowns, and waterproof sheets if you are worried about soiling linens.”
“Urinary catheters can tend to limit your movement in bed and in your room and may actually make it more difficult to walk and/or lead to falls.”
Slide 53
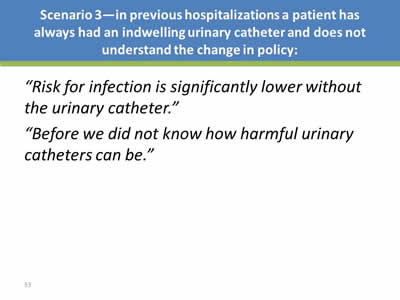
Scenario 3—in previous hospitalizations a patient has always had an indwelling urinary catheter and does not understand the change in policy:
“Risk for infection is significantly lower without the urinary catheter.”
“Before we did not know how harmful urinary catheters can be.”
Slide 54
Summary
- As healthcare providers, we forget how frightening a hospital can be.
- It’s hard for patients/families to engage when we don’t give them opportunities to participate in care.
- CAUTI remains a major, serious HAI.
- Strategies to promote health literacy and engagement may be important adjuncts in our efforts to reduce CAUTI.
Slide 55
Thank you!
Questions?
Slide 56
References
- Guide to Patient and Family Engagement in Hospital Quality and Safety. Rockville, MD: Agency for Healthcare Research and Quality; July 2013. http://www.ahrq.gov/professionals/systems/hospital/engagingfamilies/patfamilyengageguide/index.html.
- Conway J, Johnson B, Edgman-Levitan S, et.al. Partnering with Patients and Families to Design a Patient- and Family-Centered Health Care System: A Roadmap for the Future. A work in progress. (Requested by Robert Wood Johnson Foundation). Bethesda, MD: Institute for Family-Centered Care, June 2006.
- Longtin Y, Sax H, Leape L, Sheridan SE, Donaldson L, Pittet D. (2010). Patient participation: Current knowledge and applicability to patient safety. Mayo Clinic Proceedings 85(1), 53-62.
Slide 57
Funding
Prepared by the Health Research & Educational Trust of the American Hospital Association with contract funding provided by the Agency for Healthcare Research and Quality through the contract, “National Implementation of Comprehensive Unit-based Safety Program (CUSP) to Reduce Catheter-Associated Urinary Tract Infection (CAUTI), project number HHSA290201000025I/HHSA29032001T, Task Order #1.”



