Leveraging Cultural Change to Reduce Urinary Catheter Use
Slide Presentation
Slide 1
Leveraging Cultural Change to Reduce Urinary Catheter Use
Linda Greene, RN,MPS,CIC
Manager Infection Prevention
Highland Hospital
Jennifer Tuttle, RN, MSNEd
Adult Critical Care Unit
Tucson Medical Center
Images: Photos of the 2 presenters.
Slide 2
Learning Objectives
- Describe the way in which improvement in the clinical culture can facilitate efforts to reduce urinary catheter use
- Identify ways in which use of the HSOPS results and the team check-up tool can identify opportunities for improvement
- Utilize case studies to develop strategies to overcome barriers to decreasing urinary catheter device utilization
Slide 3
Polling Question #1
What is your background:
- State Lead
- CUSP Faculty
- Fellow or Mentor for CAUTI project
- Unit champion
- Team member
- Other
Slide 4
Polling Question #2
What is your greatest challenge with catheter removal?
- Physician Resistance
- Nursing Resistance
- Real or perceived need for accurate I and O
- Unit culture which does not make catheter removal a priority
Slide 5
What is the Culture?
- Culture is made up of the values, beliefs, underlying assumptions, attitudes and behaviors shared by a group of people
- Culture is the behavior that results when a group arrives at a set of - generally unspoken and unwritten - rules for working together
Slide 6
Clinical Culture
- The set of attitudes and behaviors in a clinical area or patient care unit
- Strongly influenced by leadership, experience, history and tradition
Slide 7
The Culture of Safety and Assessment of Harm
- Believe that failure to follow guidelines may cause harm
- Built in alerts
- Consequences for failure to implement
Slide 8
The Case of the Catheter
Image: Feet of a patient in a hospital bed with a catheter tube here.
Slide 9

Safety and Urinary Catheters
| Seat Belt | Yes | No |
|---|---|---|
| Believe in it | X | |
| Built in safety alerts | X | |
| Consequences | X |
| Urinary Catheter | Yes | No |
|---|---|---|
| Believe in it | ? | |
| Built in safety alerts | X | |
| Consequences | ? |
Slide 10

Clear Lessons and Culture
Image: Screen shot of top of American Journal of Infection Control article on reducing HAIs.
Slide 11
FIndings
- Fostering change – overcoming barrier
- Communication- standardized processes and metrics
- Local focused implementation – implementation at unit level
- Frontline staff engagement
- Organizational learning
- Support, resources and accountability
- Feedback and reinforcement
Slide 12
Stakeholder Assessment
Who are the Key Drivers?
- Intensivists
- Nurse Manager
- MD Director
- Nurses
Image: Cartoon of a yellow schoolbus with the words ICU Bus in the front.
Slide 13
The ICU Culture
How important is reduction in urinary catheter use?
- Medical Director
- Nurse Manager
- Nurses
- Intensivists
- Others
Slide 14

Three Levels of Organizational Culture
“…values reflect desired behavior but are not reflected in observed behavior.” (Schein, 2010, pp. 24, 27)
Image: Pyramid with the top level saying Behaviors, middle level Beliefs & Values, and Underlying Assumptions. The three levels point to the table on the right of it.
| Desired Behavior: Round to assess catheter appropriateness |
Observed Behavior: Do not participate in rounds |
| Value: Teamwork |
Value: Autonomy |
| Assumption: Safety is a system property |
Assumption: Safety is a result of individual competency |
Slide 15
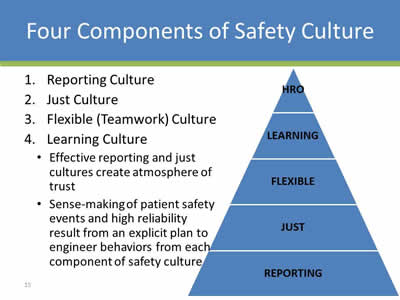
Four Components of Safety Culture
- Reporting Culture
- Just Culture
- Flexible (Teamwork) Culture
- Learning Culture:
- Effective reporting and just cultures create atmosphere of trust
- Sense-making of patient safety events and high reliability result from an explicit plan to engineer behaviors from each component of safety culture
Image: Pyramid with the following layers from top to bottom: HRO, Learning, Flexible, Just, and Reporting.
Slide 16
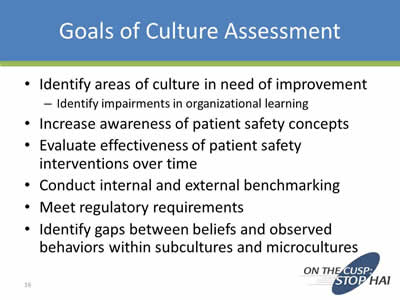
Goals of Culture Assessment
- Identify areas of culture in need of improvement:
- Identify impairments in organizational learning
- Increase awareness of patient safety concepts
- Evaluate effectiveness of patient safety interventions over time
- Conduct internal and external benchmarking
- Meet regulatory requirements
- Identify gaps between beliefs and observed behaviors within subcultures and microcultures
Slide 17

Core Aspects of Safety Culture
Image: This image is of a converging radial that outlines six domains of safety culture. The central red circle is labeled culture of safety. Surrounding this red circle are six boxes with arrows pointing to the circle. These boxes are labeled: (1) communication patterns and language, (2) feedback, reward, and corrective action practices, (3) formal and informal leader actions and expectations, (4) teamwork processes (e.g., back-up behavior), (5) resource allocation practices, and (6) error-detection and corrective system. This image is based on definitions of culture proposed by Dr. Edgar Schein, MIT Sloan School of Management. Source: Armstrong Institute for Patient Safety and Quality
Slide 18
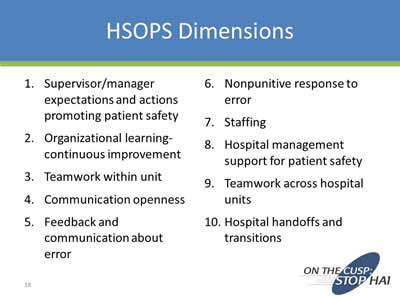
HSOPS DImensions
- Supervisor/manager expectations and actions promoting patient safety
- Organizational learning-continuous improvement
- Teamwork within unit
- Communication openness
- Feedback and communication about error
- Nonpunitive response to error
- Staffing
- Hospital management support for patient safety
- Teamwork across hospital units
- Hospital handoffs and transitions
Slide 19
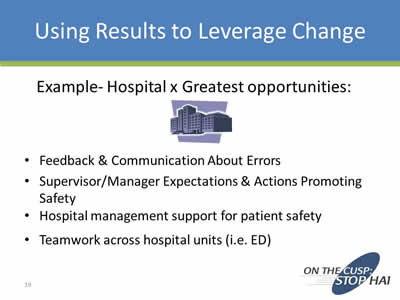
Using Results to Leverage Change
Example- Hospital x Greatest opportunities:
- Feedback & Communication About Errors
- Supervisor/Manager Expectations & Actions Promoting Safety
- Hospital management support for patient safety
- Teamwork across hospital units (i.e. ED)
Slide 20

Connect the Dots to the Urinary Catheter
Is management engaged?
Do we give routine feedback on appropriateness?
Are evidence based guidelines implemented, shared and incorporated into practice?
What strategies can we develop that can improve or enhance this?
Slide 21
Leverage the Power and the Wisdom of the Front Line
What Can We Do?
Images: Photo of nurse tending to a patient, and a photo of a doctor.
Slide 22
Case Scenario #1: Teamwork across Hospital Units
Nurse ED gives report to Nurse Med on the medical floor. “Patient A is an 87-year-old woman with cellulitis in her right lower extremity. She arrived from her long-term care facility with fever, inflammation, swelling of the leg. She is alert, but confused. We started a peripheral IV and antibiotics. She’s also complained of some nausea and vomited once. We gave her an antiemetic. You’re ready for her now? Wonderful. I’ll send her up with the transport tech.”
Nurse Med calls back to the ED 20 minutes later and asks for Nurse ED. “Patient A arrived with drenched linens after she urinated on herself. And then, she kept trying to get out of bed, telling us she had to go to the bathroom. Why didn’t you put a catheter in her? You told me she was confused. She’s going to fall trying to get up.”
Slide 23
Scenario #2: Hospital Management Support for Patient Safety
The surgical unit is not discontinuing urinary catheters despite the fact that a nurse driven removal protocol is in place. When discussing the issue with the front line staff, they report that the chief of surgery has created a road block despite the fact that the protocol was vetted with stakeholders and approved by the medical executive committee.
The Nurse manager does not “want to make waves” and has not made the nurses accountable for following the new protocol.
You approach the Chief of Surgery but he is non engaged and somewhat hostile. He tells you that in his department they do not practice “ Cookie Cutter” medicine.
Thoughts?
Slide 24
Tools
- Separate the People from the Problem:
- Disentangle the relationship from the substance
- Focus on Interests, not Positions
- Work together to find creative and fair solutions
Image: Cover of the book Getting to Yes by Roger Fisher and William Ury.
Slide 25
Back to the Surgeon
Why is the surgeon opposed to the new protocol?
Is there a rational reason?
How might we engage him?
What is the common interest here- patient safety?
What about the nurse manager?
Slide 26
A Sense of Urgency
“Plans and actions should always focus on others' hearts as much or more than their minds. Behaving with passion, conviction, optimism, urgency, and a steely determination will trump an analytically brilliant memo every time.”
Image: Cover of the book "A Sense of Urgency" by John P. Kotter.
Slide 27
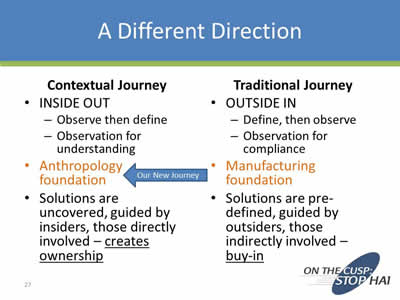
A Different Direction
Contextual Journey
- Inside Out:
- Observe then define
- Observation for understanding
- Anthropology foundation (arrow pointing to words saying Our New Journey from Manufacturing foundation)
- Solutions are uncovered, guided by insiders, those directly involved – creates ownership
Traditional Journey
Traditional Journey
- Outside In:
- Define, then observe
- Observation for compliance
- Manufacturing foundation
- Solutions are pre-defined, guided by outsiders, those indirectly involved – buy-in
Slide 28
Polling Question #3
What strategies for catheter removal have you implemented in your organization?
- Nurse driven protocols
- Automatic reminder or stop orders
- Daily rounding
- None of the above
Slide 29
CAUTI ICU Team: A Success Story
Melanie Bunger RN - Nights
Julie Davis RN- Days
Stephanie Donovan RN, MSNEd
Nina Mazzola, Manager Infection Control
Aunne Shepler RN - Nights
Pat Smothers, PCT - Days
Jenny Tuttle RN, MSNEd, Lead
Lisa Hymson, Infection Control Lisa Vasquez RN - Days
Image: Sign of the Tucson Medical Center.
Slide 30
Hospital Information
- 611 bed – Major teaching hospital
- Unit 450 – 16 bed ICU:
- Neuro/Neurosurgical
- Medical
- Pulmonary
- Vascular surgery
- General surgery
Slide 31

Our Journey
Building a Team
- Choosing strong peers to support goal
- All shifts represented
Audit Process
- Customizing tool to evaluate for deficits
- Identifying barriers – Cracking the ICU mentality
Case Reviews - Team
- Isolating root cause
- Review processes/practices
- Identifying vented patient populations – guideline
Collaboration with other Departments
- Emergency Room
- Operating Room
- Transportation
- Radiology
Providing the staff the tools/supplies
- Assessing supplies currently available
- Product trials
Slide 32
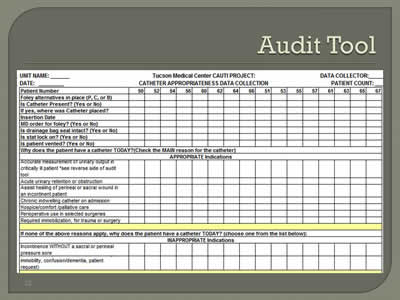
Audit Tool
Image: Screen shot of a CAUTI Project audit tool.
Slide 33
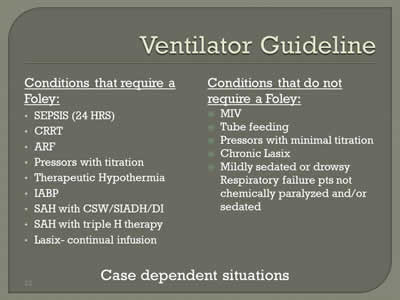
Ventilator Guideline
Conditions that require a Foley:
- Sepsis (24 Hrs)
- CRRT
- ARF
- Pressors with titration
- Therapeutic Hypothermia
- IABP
- SAH with CSW/SIADH/DI
- SAH with triple H therapy
- Lasix- continual infusion
Conditions that do not require a Foley:
- MIV
- Tube feeding
- Pressors with minimal titration
- Chronic Lasix
- Mildly sedated or drowsy Respiratory failure pts not chemically paralyzed and/or sedated
Case dependent situations
Slide 34

Providing the Tools to Succeed
- Executive Support
- Supplies:
- Scales
- External devices
- Bladder scanner
- Premium pads
- Daily Conversations
- Engaging the staff
- Challenging the status quo\
- Giving them an opportunity to give feedback
Slide 35
Rewarding the Behavior
- Infection Control – Cake the first month
- Culture “Change”
- Updates
Slide 36
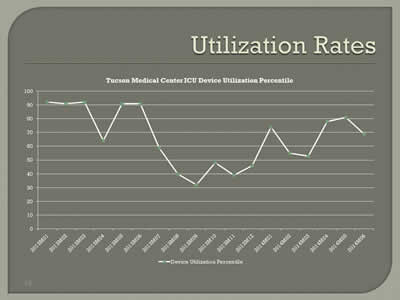
Utilization Rates
Image: Line graph showing utlization rates of ICU devices at Tucson Medical Center.
Slide 37
Lessons Learned
- We all own this: Infection Control, Nursing, Physicians …..
- Physician buy-in
- Bringing all the stakeholders
- Don’t give up – keep at it
Slide 38

Thank You!!!!
Image: Photo of Tucson Medical Center.
Slide 39
Summary and Next Steps
- What is your organizational culture?
- How can you utilize the components of the culture of safety model to assess and improve your organizational culture?
- How can you leverage HSOPS results for change?
Slide 40
Thank you!
Questions?
Slide 41
Funding
Prepared by the Health Research & Educational Trust of the American Hospital Association with contract funding provided by the Agency for Healthcare Research and Quality through the contract, “National Implementation of Comprehensive Unit-based Safety Program (CUSP) to Reduce Catheter-Associated Urinary Tract Infection (CAUTI), project number HHSA290201000025I/HHSA29032001T, Task Order #1.”



