Preventing CAUTI: Engaging Clinicians and Senior Leadership to Implement Change
Slide presentation
Slide 1
Preventing CAUTI: Engaging Clinicians and Senior Leadership to Implement Change
Sanjay Saint, MD, MPH
M. Todd Greene, MPH, PhD
University of Michigan Medical School
Ann Arbor VA Medical Center
Images: Photos of the 2 presenters, the University of Michigan Health System logo, and the On the CUSP: Stop HAI logo.
Slide 2
Learning Objectives
- Describe the methods to engage clinicians in CAUTI prevention
- Describe methods to engage leadership in CAUTI prevention
- Employ the CAUTI cost calculator
- Identify future directions for implementing change
Slide 3
Healthcare-Associated Infection
- At least 20% of episodes are preventable; perhaps up to 70% (Harbath et al. J Hosp Infect 2003; Umscheid et al. ICHE 2011 )
- Preventive practices are variably used
- Infections due to devices are especially common and preventable
- Implementing change within hospitals and within specific units is often challenging
Slide 4
“The hospital is the most complex human organization ever devised…”
–Peter Drucker
Slide 5
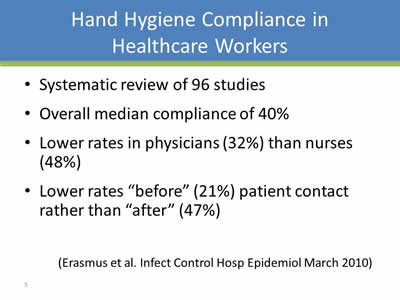
Hand Hygiene Compliance in Healthcare Workers
- Systematic review of 96 studies
- Overall median compliance of 40%
- Lower rates in physicians (32%) than nurses (48%)
- Lower rates “before” (21%) patient contact rather than “after” (47%)
(Erasmus et al. Infect Control Hosp Epidemiol March 2010)
Slide 6
Given this Gap Between What Should Be Done and What Is Done…
- Focus on “implementation science”
- “The scientific study of methods to promote the systematic uptake of research findings into routine practice”
(Eccles & Mittman. Implemetation Science. Feb 2006)
Slide 7
Image: The word Implementation in large type pointing down to the words Technical and Socio-adaptive.
Slide 8
Catheter-Associated Urinary Tract Infection (CAUTI)
- UTI is a common cause of hospital-acquired infection
- Most due to urinary catheters
- Up to 25% of inpatients are catheterized
- Leads to increased morbidity and healthcare costs
Slide 9
The Indwelling Urinary Catheter: A “1-Point” Restraint?
Satisfaction survey of 100 catheterized VA patients:
- 42% found the indwelling catheter to be uncomfortable
- 48% stated that it was painful
- 61% noted that it restricted their ADLs
- 2 patients provided unsolicited comments that their catheter “hurt like hell”
(Saint et al. JAGS 1999)
Slide 10
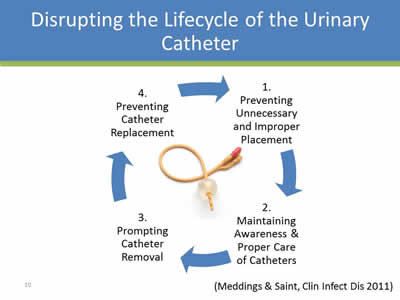
Disrupting the Lifecycle of the Urinary Catheter
Circular flowchart with the following steps, with Step 4 pointing to Step 1 and so forth.
- Preventing Unnecessary and Improper Placement
- Maintaining Awareness & Proper Care of Catheters
- Prompting Catheter Removal
- Preventing Catheter
(Meddings & Saint, Clin Infect Dis 2011)
Slide 11
A Systems (and Technical) Solution: Timely Removal of Indwelling Catheters
- 14 studies have evaluated urinary catheter reminders and stop-orders (written, computerized, nurse-initiated):
- Significant reduction in catheter use (~2.5 days)
- Significant reduction in infection (~50%)
- No evidence of harm (ie, re-insertion)
(Meddings J et al. Clin Infect Dis 2010)
Slide 12
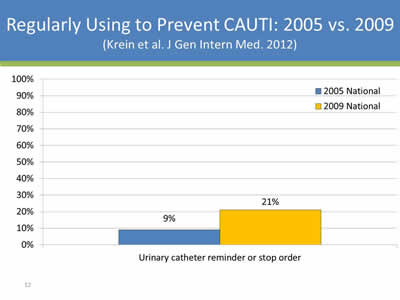
Regularly Using to Prevent CAUTI: 2005 vs. 2009
(Krein et al. J Gen Intern Med. 2012)
Image: Bar chart showing that in 2005 9%, and in 2009 21% of urinary catheters had a reminder or stop order.
Slide 13
Image: The words Implementing Change in large type pointing down to the words "At Home" and "Across the State of Michigan".
Slide 14
Hospital Outcomes Program of Excellence (HOPE)
(http://va-hope.org)
- Systems redesign grant to Ann Arbor VAMC
- Behavioral lab for interventions to improve quality and efficiency of care
- CAUTI prevention one of many initiatives: nurse-initiated reminder
- Focus: enhancing nurse-physician communication
Slide 15
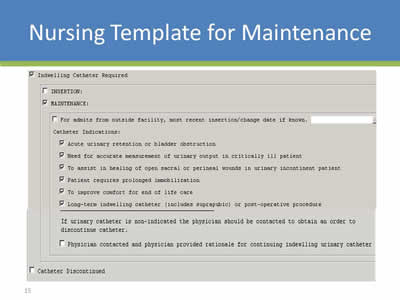
Nursing Template for Maintenance
Image: Screen shot of an indwelling urinary catheter maintenance nursing template which includes indications for continued urinary catheter use.
Slide 16
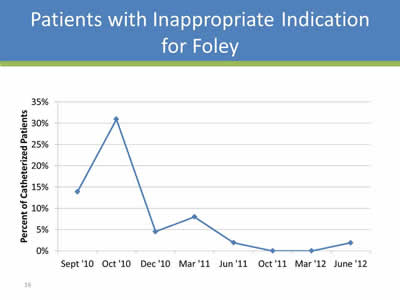
Patients with Inappropriate Indication for Foley
Image: Graph showing decrease in use of inappropriate catheters over time (Sept. 2010-June 2012)- 15-30% before initiative to almost 0 after the initiative.
Slide 17
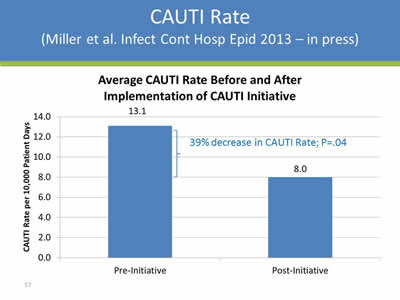
CAUTI Rate
(Miller et al. Infect Cont Hosp Epid 2013 – in press)
Image: Bar chart showing CAUTI rate of 13.1 CAUTI per 10,000 patient days before the initiative and 8.0 CAUTI per 10,000 patient days after the initiative. It is a 39% decrease in CAUTI rate, P = 0.04.
Slide 18
Image: The words Implementing Change in large type pointing down to the words "At Home" and "Across the State of Michigan", the words "At Home" are grayed out.
Slide 19
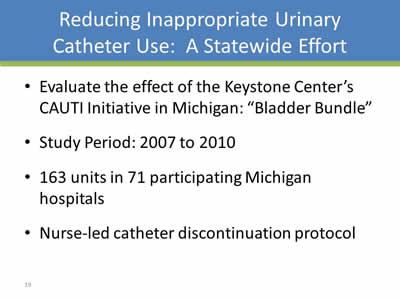
Reducing Inappropriate Urinary Catheter Use: A Statewide Effort
- Evaluate the effect of the Keystone Center’s CAUTI Initiative in Michigan: “Bladder Bundle”
- Study Period: 2007 to 2010
- 163 units in 71 participating Michigan hospitals
- Nurse-led catheter discontinuation protocol
Slide 20
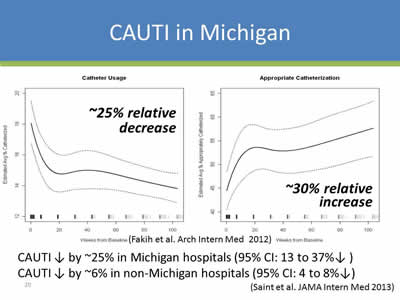
CAUTI in Michigan
Image: Graphs showing Foley Use in Michigan: 2007-2010. Approximately 25% relative decrease in catheter usage and approximately 30% relative increase in appropriate catheterization.
CAUTI ↓ by ~25% in Michigan hospitals (95% CI: 13 to 37%↓ )
CAUTI ↓ by ~6% in non-Michigan hospitals (95% CI: 4 to 8%↓)
(Saint et al. JAMA Intern Med 2013)
Slide 21
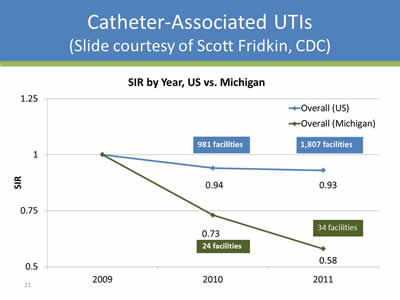
Catheter-Associated UTIs
(Slide courtesy of Scott Fridkin, CDC)
Image: Graph of SIR for CAUTI for US and Michigan for 2009 (1;1), 2010 (0.94;0.73), and 2011 (0.93;0.58).
Slide 22
A key ingredient for success is figuring out how to engage the clinicians in the hospital.
Slide 23
Learning Objectives
- Describe the methods to engage clinicians in CAUTI prevention
- Describe methods to engage leadership in CAUTI prevention
- Employ the CAUTI cost calculator
- Identify future directions for implementing change
Slide 24
Start with a Plan
- Form a CAUTI prevention team that consists of various key people, with one person identified as the team leader
- Develop a CAUTI policy for the institution; the basics should be covered (e.g., condom catheters, bladder scanners)
- Pick a unit where to begin, usually where there are the most number of catheters
Slide 25
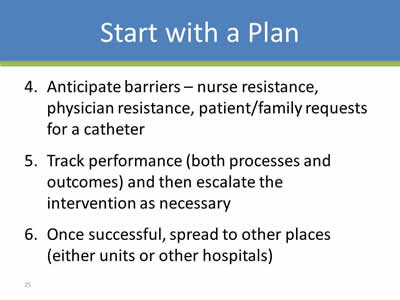
Start with a Plan
- Anticipate barriers – nurse resistance, physician resistance, patient/family requests for a catheter
- Track performance (both processes and outcomes) and then escalate the intervention as necessary
- Once successful, spread to other places (either units or other hospitals)
Slide 26
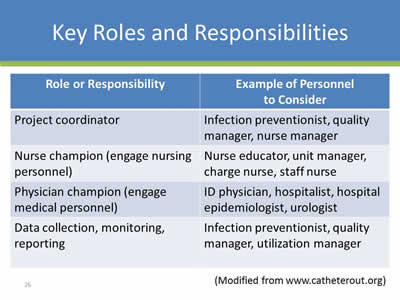
Key Roles and Responsibilities
| Role or Responsibility | Example of Personnel to Consider |
|---|---|
| Project coordinator | Infection preventionist, quality manager, nurse manager |
| Nurse champion (engage nursing personnel) | Nurse educator, unit manager, charge nurse, staff nurse |
| Physician champion (engage medical personnel) | ID physician, hospitalist, hospital epidemiologist, urologist |
| Data collection, monitoring, reporting | Infection preventionist, quality manager, utilization manager |
Modified from www.catheterout.org)
Slide 27
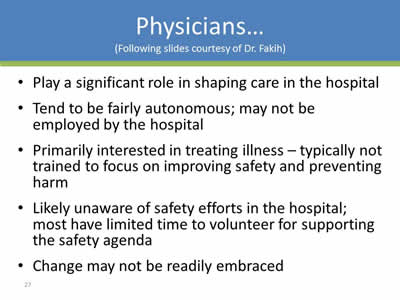
Physicians…
(Following slides courtesy of Dr. Fakih)
- Play a significant role in shaping care in the hospital
- Tend to be fairly autonomous; may not be employed by the hospital
- Primarily interested in treating illness – typically not trained to focus on improving safety and preventing harm
- Likely unaware of safety efforts in the hospital; most have limited time to volunteer for supporting the safety agenda
- Change may not be readily embraced
Slide 28
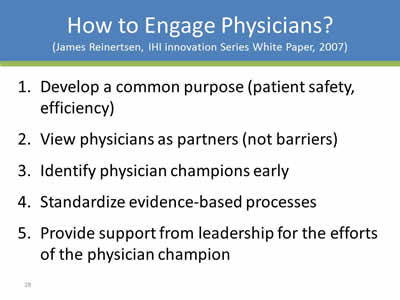
How to Engage Physicians?
(James Reinertsen, IHI innovation Series White Paper, 2007)
- Develop a common purpose (patient safety, efficiency)
- View physicians as partners (not barriers)
- Identify physician champions early
- Standardize evidence-based processes
- Provide support from leadership for the efforts of the physician champion
Slide 29

Overcoming Resistance: Finding a Member of the Tribe
- A chief of staff (and a surgeon): “...surgeons are very tribal so what you need to do if you have something that you think is a best practice at your hospital…you need to get…either the chair of surgery or some reasonable surgeon…If you come in and you’re an internist …into a group of surgeons …the first thing we’re going to do is we’re going to say, ‘Look, you’re not one of us’…the way to get buy-in from surgeons is you got to have a surgeon on your team.”
(Saint et al. Joint Comm Journal Qual Safety 2009)
Slide 30

The Physician Champion & Physician Supporters
Image: Figure showing different types of physicians that could be a CAUTI physician champion.
Slide 31
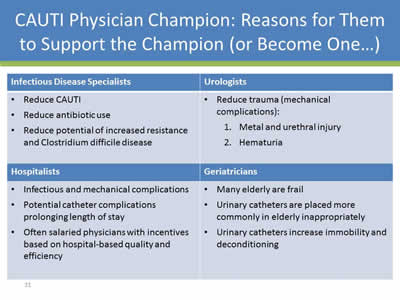
CAUTI Physician Champion: Reasons for Them to Support the Champion (or Become One…)
Infectious Disease Specialists
- Reduce CAUTI
- Reduce antibiotic use
- Reduce potential of increased resistance and Clostridium difficile disease
Hospitalists
- Infectious and mechanical complications
- Potential catheter complications prolonging length of stay
- Often salaried physicians with incentives based on hospital-based quality and efficiency
Urologists
- Reduce trauma (mechanical complications):
- Metal and urethral injury
- Hematuria
Geriatricians
- Many elderly are frail
- Urinary catheters are placed more commonly in elderly inappropriately
- Urinary catheters increase immobility and deconditioning
Slide 32
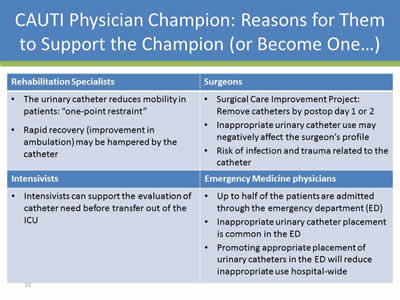
CAUTI Physician Champion: Reasons for Them to Support the Champion (or Become One…)
Rehabilitation Specialists
- The urinary catheter reduces mobility in patients: "one-point restraint"
- Rapid recovery (improvement in ambulation) may be hampered by the catheter
Intensivists
- Intensivists can support the evaluation of catheter need before transfer out of the ICU
Surgeons
- Surgical Care Improvement Project: Remove catheters by postop day 1 or 2
- Inappropriate urinary catheter use may negatively affect the surgeon’s profile
- Risk of infection and trauma related to the catheter
Emergency Medicine physicians
- Up to half of the patients are admitted through the emergency department (ED)
- Inappropriate urinary catheter placement is common in the ED
- Promoting appropriate placement of urinary catheters in the ED will reduce inappropriate use hospital-wide
Slide 33
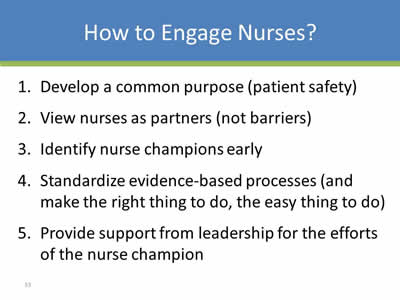
How to Engage Nurses?
- Develop a common purpose (patient safety)
- View nurses as partners (not barriers)
- Identify nurse champions early
- Standardize evidence-based processes (and make the right thing to do, the easy thing to do)
- Provide support from leadership for the efforts of the nurse champion
Slide 34
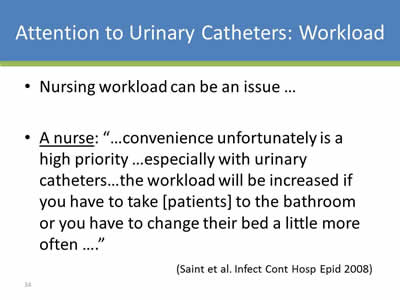
Attention to Urinary Catheters: Workload
- Nursing workload can be an issue …
- A nurse: “…convenience unfortunately is a high priority …especially with urinary catheters…the workload will be increased if you have to take [patients] to the bathroom or you have to change their bed a little more often ….”
(Saint et al. Infect Cont Hosp Epid 2008)
Slide 35
Overcoming Barriers
- Nurse buy-in is key to success
- A physician administrator: “Because the nurses on the geriatrics unit wanted to have their patients regain mobility…they viewed mobility as very important …versus the other units where the nurses didn’t necessarily feel that was a real goal..”
- A nurse champion is critically important!
Slide 36
Identifying the “Champion”
- Successful champions tend to be intrinsically motivated and enthusiastic about the practices they promote:
“I have a certain stature in this hospital…People know that I’m very passionate about patient care so…I get positive reinforcement from them…they’re happy to see me…because …they know that I’m thinking about what’s best for the patient…”
(Damschroder et al., Qual and Safety in Healthcare 2009)
Slide 37
Learning Objectives
- Describe the methods to engage clinicians in CAUTI prevention
- Describe methods to engage leadership in CAUTI prevention
- Employ the CAUTI cost calculator
- Identify future directions for implementing change
Slide 38
Leadership Engagement Can Help
- The key senior leaders in preventing CAUTI are the CNO and CMO
- But other leaders are important…
- Unit managers/chiefs, service-line chiefs, hospital epidemiologist, infection preventionist
Slide 39
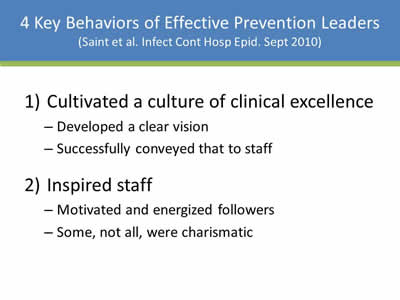
4 Key Behaviors of Effective Prevention Leaders
(Saint et al. Infect Cont Hosp Epid. Sept 2010)
- Cultivated a culture of clinical excellence:
- Developed a clear vision
- Successfully conveyed that to staff
- Inspired staff:
- Motivated and energized followers
- Some, not all, were charismatic
Slide 40
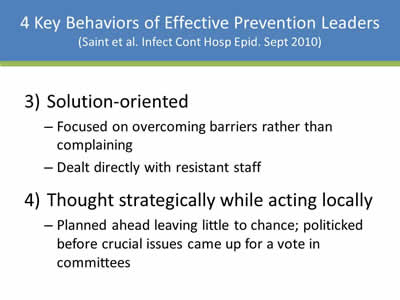
4 Key Behaviors of Effective Prevention Leaders
(Saint et al. Infect Cont Hosp Epid. Sept 2010)
- Solution-orientedL
- Focused on overcoming barriers rather than complaining
- Dealt directly with resistant staff
- Thought strategically while acting locally:
- Planned ahead leaving little to chance; politicked before crucial issues came up for a vote in committees
Slide 41
One way to engage the leaders at your hospital is by showing them that you have a good plan.
Slide 42
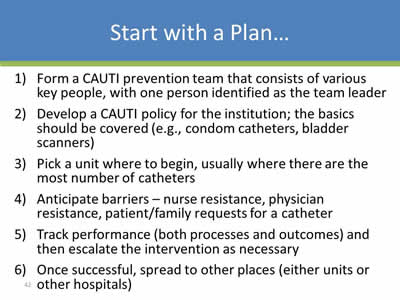
Start with a Plan…
- Form a CAUTI prevention team that consists of various key people, with one person identified as the team leader
- Develop a CAUTI policy for the institution; the basics should be covered (e.g., condom catheters, bladder scanners)
- Pick a unit where to begin, usually where there are the most number of catheters
- Anticipate barriers – nurse resistance, physician resistance, patient/family requests for a catheter
- Track performance (both processes and outcomes) and then escalate the intervention as necessary
- Once successful, spread to other places (either units or other hospitals)
Slide 43
Another way to engage the leaders at your hospital is by showing them that you have a good plan B.
Slide 44
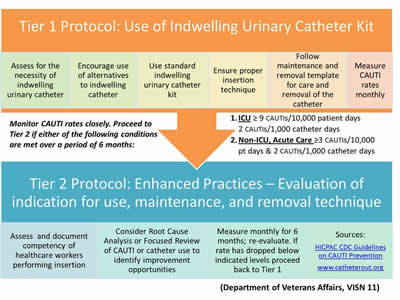
Image: Screen shot of a table depicting the two-tier protocol implemented to reduce Catheter Use and harm in a VA facility.
Slide 45
A third way to engage the leaders at your hospital is by considering sustainability at the outset.
Slide 46

Acknowledgements…
Mohamad Fakih, MD, MPH
Medical Director, Infection Prevention and Control
St. John Hospital and Medical Center
Sarah Krein, PhD, RN
Research Associate Professor, Division of General Medicine
University of Michigan, Ann Arbor
Images: Photos of the 2 presenters.
Slide 47
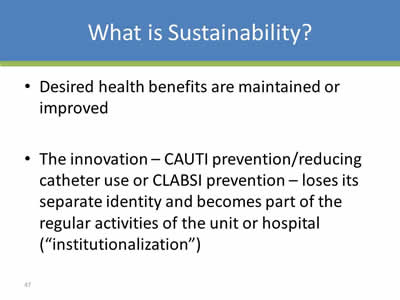
What is Sustainability?
- Desired health benefits are maintained or improved
- The innovation – CAUTI prevention/reducing catheter use or CLABSI prevention – loses its separate identity and becomes part of the regular activities of the unit or hospital (“institutionalization”)
Slide 48
Factors that Influence Sustainability
- Integration with existing programs/services (“institutionalization”)
- Program champions
- Periodic evaluation and feedback
Slide 49
1) Institutionalization
- The initiative becomes part of the “standard of care” in the hospital (or unit):
- Only place the urinary catheter based on appropriate indications
- Comply with proper insertion and maintenance
- Evaluate daily for need; remove if unnecessary
- With time, modifications of the program may occur based on new evidence (e.g., appropriate indications)
Slide 50
1) Institutionalization
- Routinization and Integration:
- Align with the organization’s goals (e.g., promoting safety)
- Regular education and competencies
- Nursing daily routine
- Use of electronic reminders/nursing templates
- Identify how this work might be synergistic with other initiatives
Slide 51
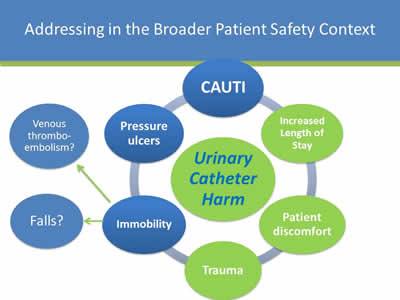
Addressing in the Broader Patient Safety Context
Image: Diagram showing the various causes of Urinary Catheter Harm.
Slide 52
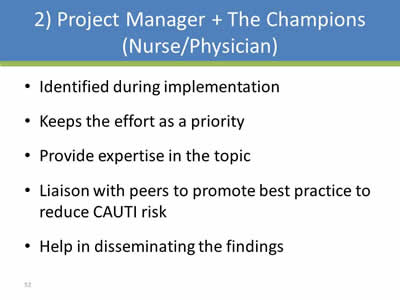
2) Project Manager + The Champions (Nurse/Physician)
- Identified during implementation
- Keeps the effort as a priority
- Provide expertise in the topic
- Liaison with peers to promote best practice to reduce CAUTI risk
- Help in disseminating the findings
Slide 53
Factors that Influence Sustainability
- Integration with existing programs/services (“institutionalization”)
- Program champions
- Periodic evaluation and feedback
Slide 54
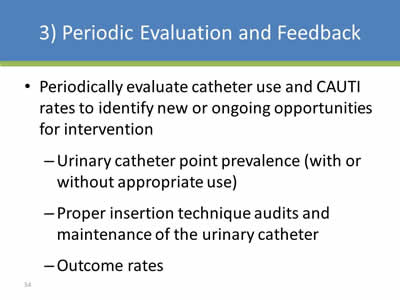
3) Periodic Evaluation and Feedback
- Periodically evaluate catheter use and CAUTI rates to identify new or ongoing opportunities for intervention:
- Urinary catheter point prevalence (with or without appropriate use)
- Proper insertion technique audits and maintenance of the urinary catheter
- Outcome rates
Slide 55
A final way to engage leaders is to discuss money with them…
Slide 56
Learning Objectives
- Describe the methods to engage clinicians in CAUTI prevention
- Describe methods to engage leadership in CAUTI prevention
- Employ the CAUTI cost calculator
- Identify future directions for implementing change
Slide 57
CAUTI Cost Calculator
- Estimates hospital’s costs due to CAUTI
- Estimates both current costs and projected costs after a hypothetical intervention to reduce catheter use
- www.catheterout.org
Slide 58
CAUTI Cost Calculator
- Time to event framework
- Event times among “n” catheterized patients
- Tbact = time to bacteriuria from catheter placement
- TSUTI = time to SUTI from bacteriuria
- TBSI = time to BSI from bacteriuria
- Tremv = time to removal from placement
Slide 59
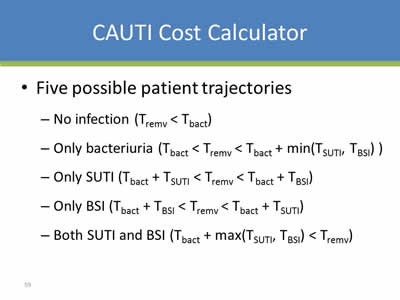
CAUTI Cost Calculator
- Five possible patient trajectories:
- No infection (Tremv < Tbact)
- Only bacteriuria (Tbact < Tremv < Tbact + min(TSUTI, TBSI) )
- Only SUTI (Tbact + TSUTI < Tremv < Tbact + TBSI)
- Only BSI (Tbact + TBSI < Tremv < Tbact + TSUTI)
- Both SUTI and BSI (Tbact + max(TSUTI, TBSI) < Tremv)
Slide 60
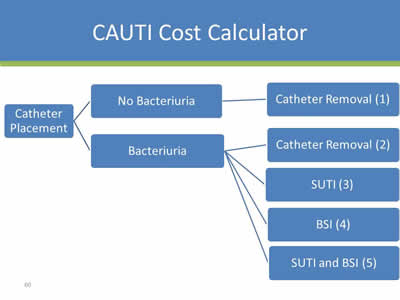
CAUTI Cost Calculator
Image: Flowchart showing outcomes of urinary catheter placement. If no bacteriuria, then catheter removal (1). If yes bacteriuria, then options include catheter removal (2), develop SUTI (3), develop BSI (4), or get both SUTI and BSI (5).
Slide 61
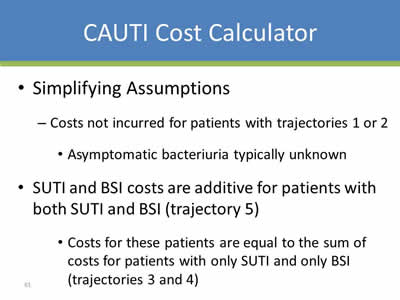
CAUTI Cost Calculator
- Simplifying Assumptions:
- Costs not incurred for patients with trajectories 1 or 2
- Asymptomatic bacteriuria typically unknown
- Costs not incurred for patients with trajectories 1 or 2
- SUTI and BSI costs are additive for patients with both SUTI and BSI (trajectory 5):
- Costs for these patients are equal to the sum of costs for patients with only SUTI and only BSI (trajectories 3 and 4)
Slide 62
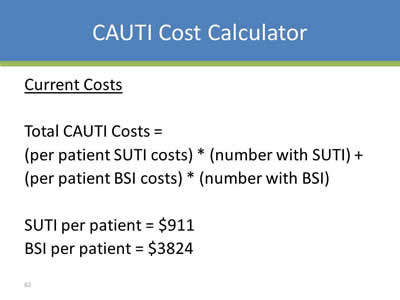
CAUTI Cost Calculator
Current Costs
Total CAUTI Costs = (per patient SUTI costs) * (number with SUTI) + (per patient BSI costs) * (number with BSI)
SUTI per patient = $911
BSI per patient = $3824
Slide 63
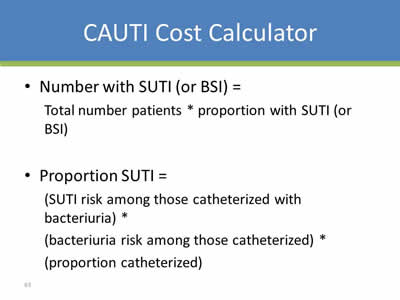
CAUTI Cost Calculator
- Number with SUTI (or BSI) = Total number patients * proportion with SUTI (or BSI)
- Proportion SUTI = (SUTI risk among those catheterized with bacteriuria) * (bacteriuria risk among those catheterized) * (proportion catheterized)
Slide 64
CAUTI Cost Calculator
- Intervention to reduce CAUTI risk through:
- Reducing placement (i.e., proportion catheterized)
- Reducing duration (i.e., mean duration of catheterization)
- Post intervention risk of bacteriuria as a function of:
- Percent decrease in mean duration due to intervention
- Pre-intervention risk of bacteriuria among catheterized
Slide 65
CAUTI Cost Calculator
- Post intervention costs characterized as function of:
- User-specified quantities
- Quantities specific to intervention (plausible range)
- Estimates from the literature
Slide 66
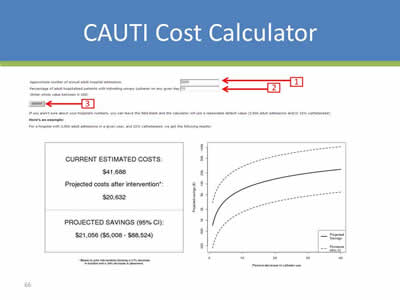
CAUTI Cost Calculator
Image: Screen shot from a CAUTI Cost Calculator website.
Slide 67
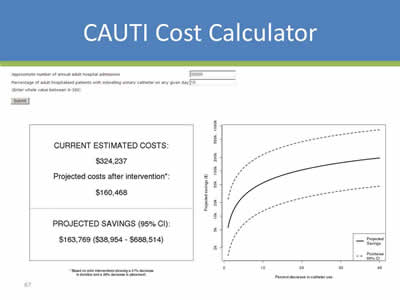
CAUTI Cost Calculator
Image: Screen shot from a CAUTI Cost Calculator website.
Slide 68
CAUTI Cost Calculator: Caveats
- Requires users to have input estimates
- Projected costs/potential savings do not consider full range of cost factors:
- Asymptomatic bacteriuria
- Cost of intervention
- Opportunity costs
Slide 69
CAUTI Cost Calculator
- Ongoing:
- Manuscript submitted to Journal Hospital Medicine
- Kennedy EH, Greene MT, Saint S. Estimating Hospital Costs of Catheter-Associated Urinary Tract Infection
- Modifying interface to display additional results:
- Intervention focused only on reducing duration
- Intervention focused only on reducing placement
- Manuscript submitted to Journal Hospital Medicine
Slide 70
Learning Objectives
- Describe the methods to engage clinicians in CAUTI prevention
- Describe methods to engage leadership in CAUTI prevention
- Employ the CAUTI cost calculator
- Identify future directions for implementing change
Slide 71
The Future...
Trouble-Shooting Guide
Slide 72
Understanding Why Some Hospitals are Better than Others in Preventing Infection
- Mixed-methods national studies focusing on 3 HAIs: CAUTI, CLABSI, and VAP
- Funded by VA, NIH, and AHRQ
- Phone interviews and site visits to hospitals across the U.S.
- Interviewees were at various levels in the organization
Slide 73
Qualitative Experience
- A total of 198 formal interviews completed at 37 U.S. hospitals between 2005 and 2013:
- Conducted via phone or in person (14 site visits)
- Currently helping investigators in Switzerland on a mixed-methods study of HAI prevention in Europe
- Key lesson:
A LOT OF WORK!
Slide 74
Piloting a New Method
- Trying to obviate the need for site visits
- Proposing a 1-page (10-item) trouble-shooting guide:
CAUTI Guide to Patient Safety (“CAUTI GPS”)
Slide 75
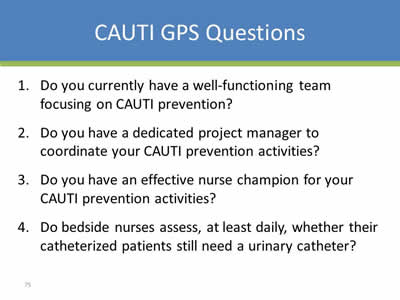
CAUTI GPS Questions
- Do you currently have a well-functioning team focusing on CAUTI prevention?
- Do you have a dedicated project manager to coordinate your CAUTI prevention activities?
- Do you have an effective nurse champion for your CAUTI prevention activities?
- Do bedside nurses assess, at least daily, whether their catheterized patients still need a urinary catheter?
Slide 76
CAUTI GPS Questions
- Do bedside nurses ensure the Foley is removed when no longer needed (e.g., by contacting the physician or removing the catheter per protocol)?
- Do you have an effective physician champion for your CAUTI prevention activities?
- Have physicians fully embraced CAUTI prevention activities?
Slide 77
CAUTI GPS Questions
- Has senior leadership fully supported CAUTI prevention activities?
- Do you currently collect CAUTI-related data (e.g., catheter prevalence and appropriateness) in the unit(s) in which you are intervening?
Slide 78
CAUTI GPS Questions
- Have you experienced any of the following barriers:
- Substantial nursing resistance?
- Substantial physician resistance?
- Patient and family requests for a Foley?
- Foleys commonly being inserted in the ED without an appropriate indication?
Slide 79
Learning Objectives
√ Describe the methods to engage clinicians in CAUTI prevention
√ Describe methods to engage leadership in CAUTI prevention
v Employ the CAUTI cost calculator
√ Identify future directions for implementing change
Slide 80
Thank you!
Questions?
Slide 81
Funding
Prepared by the Health Research & Educational Trust of the American Hospital Association with contract funding provided by the Agency for Healthcare Research and Quality through the contract, “National Implementation of Comprehensive Unit-based Safety Program (CUSP) to Reduce Catheter-Associated Urinary Tract Infection (CAUTI), project number HHSA290201000025I/HHSA29032001T, Task Order #1.”