Preventing CAUTI: What to Do When It’s Time for Plan B
Slide Presentation
Slide 1

Preventing CAUTI: What to Do When it’s Time for Plan B
Sanjay Saint, MD, PhD
George Dock Collegiate Professor of Internal Medicine
Division of General Medicine
University of Michigan Health Systems
Associate Chief of Medicine, Ann Arbor VA Medical Center
Sarah Krein, PhD, RN
Research Associate Professor, Division of General Medicine
Department of Internal Medicine
University of Michigan, Ann Arbor
Kathlyn Fletcher, MD, PhD
Associate Professor of Medicine
Medical College of Wisconsin and the Milwaukee VAMC
Associate Program Director, MCW Internal Medicine Residency
Images: Photos of the 3 presenters. Logos for the VA Medical System, Medical College of Wisconsin, and University of Michigan Health System are shown on bottom of slide.
Slide 2
Learning Objectives
- Define basic principles of CAUTI prevention
- Describe approaches to consider if CAUTI rates are not where you want them to be
- State how the GPS can support units with ongoing CAUTI problems
- Apply mindfulness to CAUTI prevention
Slide 3
Catheter-Associated Urinary Tract Infection (CAUTI)
- UTI is a common cause of hospital-acquired infection
- Most due to urinary catheters
- Up to 20 percent of inpatients are catheterized
Leads to increased morbidity and health care costs
www.catheterout.org
Slide 4
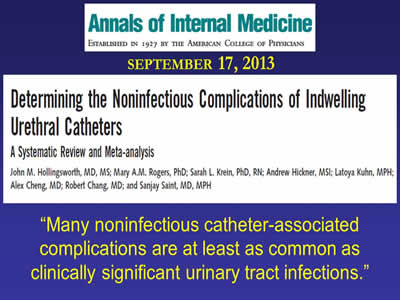
“Many noninfectious catheter-associated complications are at least as common as clinically significant urinary tract infections.”
Image: Annals of Internal Medicine, September 17, 2013. Article titled "Determining the Noninfectious Complications of Indwelling Urethral Catheters".
Slide 5
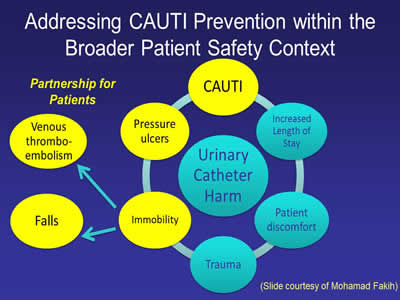
Addressing CAUTI Prevention within the Broader Patient Safety Context
Image: Diagram showing interaction between different factors that can cause urinary catheter harm.
(Slide courtesy of Mohamad Fakih)
Slide 6
How can we reduce catheter use and prevent CAUTI?
Slide 7
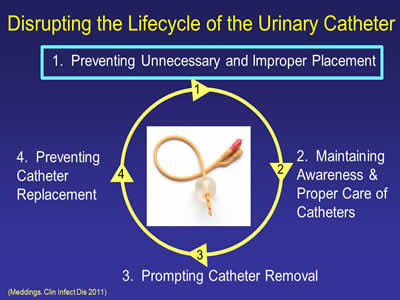
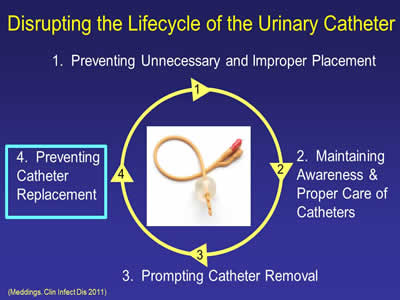
Disrupting the Lifecycle of the Urinary Catheter
- Preventing Unnecessary and Improper Placement
- Maintaining Awareness & Proper Care of Catheters
- Prompting Catheter Removal
- Preventing Catheter Replacement
(Meddings. Clin Infect Dis 2011)
Image: In center of steps is a photo of a urinary catheter.
Slide 8
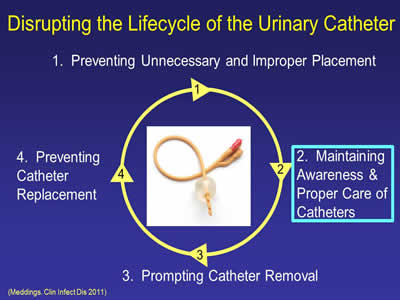
Disrupting the Lifecycle of the Urinary Catheter
- Preventing Unnecessary and Improper Placement
- Maintaining Awareness & Proper Care of Catheters
- Prompting Catheter Removal
- Preventing Catheter Replacement
(Meddings. Clin Infect Dis 2011)
Image: In center of steps is a photo of a urinary catheter.
Slide 9
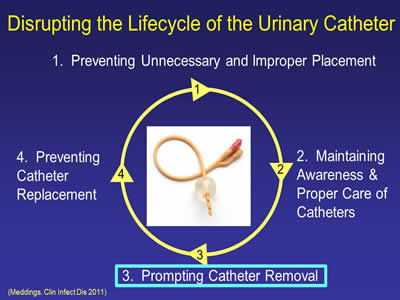
Disrupting the Lifecycle of the Urinary Catheter
- Preventing Unnecessary and Improper Placement
- Maintaining Awareness & Proper Care of Catheters
- Prompting Catheter Removal
- Preventing Catheter Replacement
(Meddings. Clin Infect Dis 2011)
Image: In center of steps is a photo of a urinary catheter.
Slide 10
Disrupting the Lifecycle of the Urinary Catheter
- Preventing Unnecessary and Improper Placement
- Maintaining Awareness & Proper Care of Catheters
- Prompting Catheter Removal
- Preventing Catheter Replacement
(Meddings. Clin Infect Dis 2011)
Image: In center of steps is a photo of a urinary catheter.
Slide 11
What About the ICU?
Slide 12
Just because a patient is in the ICU does NOT mean that the patient needs a Foley…
The Key Question is this:
Are hourly assessments of urine output required?
Slide 13

What if you need further help in preventing CAUTI?
Sarah Krein, PhD, RN
Image: Photo of Sarah Krein.
Slide 14
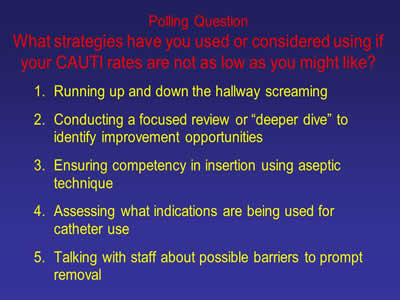
Polling Question: What strategies have you used or considered using if your CAUTI rates are not as low as you might like?
- Running up and down the hallway screaming
- Conducting a focused review or “deeper dive” to identify improvement opportunities
- Ensuring competency in insertion using aseptic technique
- Assessing what indications are being used for catheter use
- Talking with staff about possible barriers to prompt removal
Slide 15
Additional Approaches
- Tier 1 & Tier
- CAUTI GPS
- Applying Mindfulness to CAUTI
Slide 16
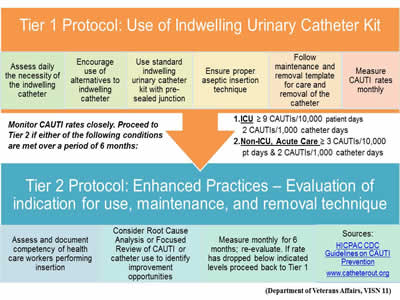
Image: Screen shot of a flowchart showing Tier 1 and Tier 2 protocols for using an indwelling urinary catheter kit and enhanced practices.
(Department of Veterans Affairs, VISN 11)
Slide 17
Additional Approaches
- Tier 1 & Tier
- CAUTI GPS
- Applying Mindfulness to CAUTI
Slide 18
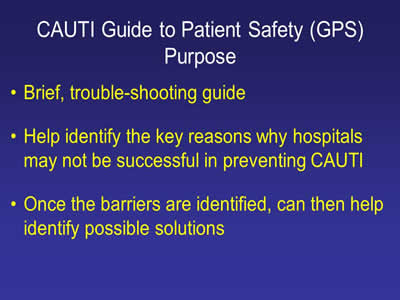
CAUTI Guide to Patient Safety (GPS) Purpose
- Brief, trouble-shooting guide
- Help identify the key reasons why hospitals may not be successful in preventing CAUTI
- Once the barriers are identified, can then help identify possible solutions
Slide 19
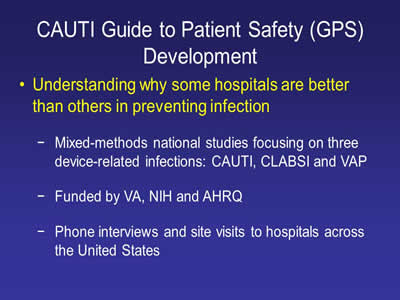
CAUTI Guide to Patient Safety (GPS) Development
- Understanding why some hospitals are better than others in preventing infection:
- Mixed-methods national studies focusing on three device-related infections: CAUTI, CLABSI and VAP
- Funded by VA, NIH and AHRQ
- Phone interviews and site visits to hospitals across the United States
Slide 20

Images: Photos of various things like a yellow taxi, Maine license plate, small airplane,and the Golden Gate Bridge.
Slide 21
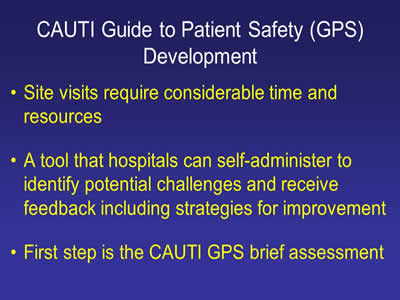
CAUTI Guide to Patient Safety (GPS) Development
- Site visits require considerable time and resources
- A tool that hospitals can self-administer to identify potential challenges and receive feedback including strategies for improvement
- First step is the CAUTI GPS brief assessment
Slide 22
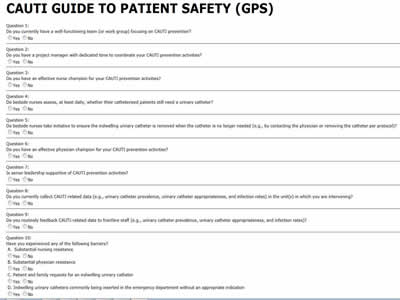
CAUTI Guide to Patient Safety (GPS)
Image: Screen shot of a CAUTI questionnaire.
Slide 23

CAUTI Guide to Patient Safety (GPS) Development
- Online tool
- Each question linked to trouble-shooting tips
www.catheterout.org
Slide 24
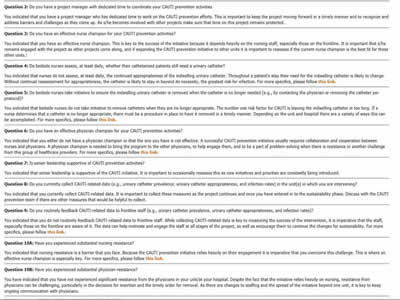
Image: Screen shot of CAUTI questionnaire.
Slide 25
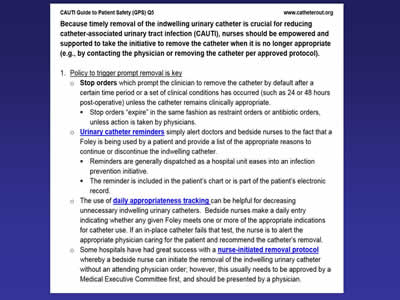
Image: Screen shot of the CAUTI Guide to Patient Safety.
Slide 26
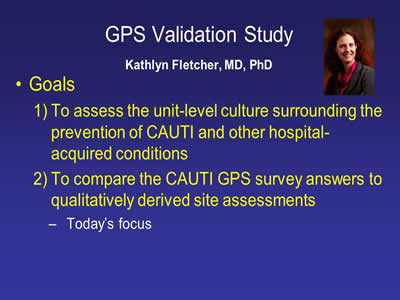
GPS Validation Study
Kathlyn Fletcher, MD, PhD
- Goals:
- To assess the unit-level culture surrounding the prevention of CAUTI and other hospital-acquired conditions
- To compare the CAUTI GPS survey answers to qualitatively derived site assessments:
- Today’s focus
Image: Photo of Kathlyn Fletcher, MD.
Slide 27
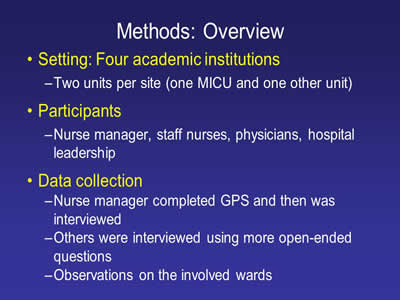
Methods: Overview
- Setting: Four academic institutions:
- Two units per site (one MICU and one other unit)
- Participants:
- Nurse manager, staff nurses, physicians, hospital leadership
- Data collection:
- Nurse manager completed GPS and then was interviewed
- Others were interviewed using more open-ended questions
- Observations on the involved wards
Slide 28
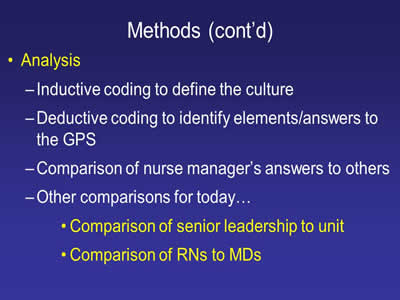
Methods (cont'd)
- Analysis:
- Inductive coding to define the culture
- Deductive coding to identify elements/answers to the GPS
- Comparison of nurse manager’s answers to others
- Other comparisons for today…
- Comparison of senior leadership to unit
- Comparison of RNs to MDs
Slide 29
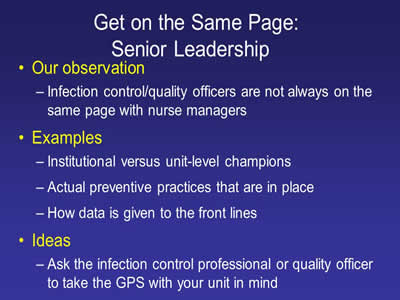
Get on the Same Page: Senior Leadership
- Our observation:
- Infection control/quality officers are not always on the same page with nurse managers
- Examples:
- Institutional versus unit-level champions
- Actual preventive practices that are in place
- How data is given to the front lines
- Ideas:
- Ask the infection control professional or quality officer to take the GPS with your unit in mind
Slide 30

Get on the Same Page: Nurses and Doctors
- Our observation:
- Doctors often have no idea about formal CAUTI prevention practices on their units
- Examples:
- Doctors have no idea what the nurses do with respect to CAUTI prevention
- MDs often aren’t aware of the existence of champions
- Ideas:
- Have MDs take the GPS
- Aggressively educate them based on gaps
Slide 31
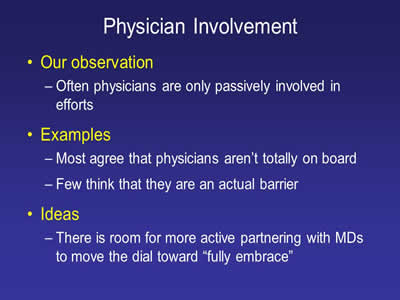
Physician Involvement
- Our observation:
- Often physicians are only passively involved in efforts
- Examples:
- Most agree that physicians aren’t totally on board
- Few think that they are an actual barrier
- Ideas:
- There is room for more active partnering with MDs to move the dial toward “fully embrace”
Slide 32
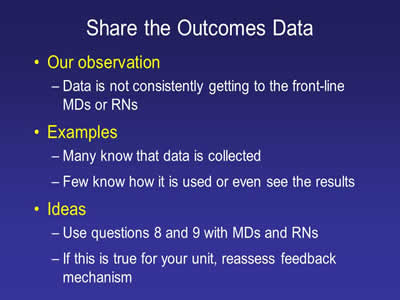
Share the Outcomes Data
- Our observation:
- Data is not consistently getting to the front-line MDs or RNs
- Examples:
- Many know that data is collected
- Few know how it is used or even see the results
- Ideas:
- Use questions 8 and 9 with MDs and RNs
- If this is true for your unit, reassess feedback mechanism
Slide 33
Other Resources...
Image: Screen shot of the book cover of "Preventing Hospital Infections: Real World Problems, Real World Solutions".
Slide 34
Additional Approaches
Sanjay Saint, MD, PhD
- Tier 1 & Tier 2
- CAUTI GPS
- Applying Mindfulness to CAUTI
Slide 35
A Dilemma
- Much of what we do in health care – especially in the hospital – is reflexive"
- If a patient is hypoxemic: we give oxygen
- Low BP: IV fluids
- Positive blood cultures: antibiotics
- Frequency, urgency, and dysuria: dx UTI
Slide 36
A Dilemma
- These rote responses are usually helpful
- However, this reflex-like approach can lead to problems:
- Patient sick enough to be admitted from the ED: Foley catheter
- Asymptomatic catheterized patient has a “dirty” urine: antibiotics
Slide 37
One Possible Solution: “Medical Mindfulness”
Slide 38
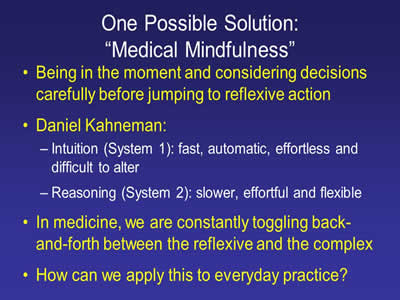
One Possible Solution: “Medical Mindfulness”
- Being in the moment and considering decisions carefully before jumping to reflexive action
- Daniel Kahneman:
- Intuition (System 1): fast, automatic, effortless and difficult to alter
- Reasoning (System 2): slower, effortful and flexible
- In medicine, we are constantly toggling back-and-forth between the reflexive and the complex
- How can we apply this to everyday practice?
Slide 39
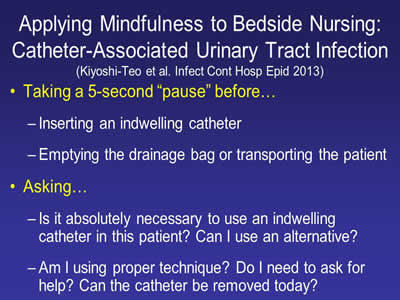
Applying Mindfulness to Bedside Nursing: Catheter-Associated Urinary Tract Infection
(Kiyoshi-Teo et al. Infect Cont Hosp Epid 2013)
- Taking a 5-second “pause” before…
- Inserting an indwelling catheter
- Emptying the drainage bag or transporting the patient
- Asking…
- Is it absolutely necessary to use an indwelling catheter in this patient? Can I use an alternative?
- Am I using proper technique? Do I need to ask for help? Can the catheter be removed today?
Slide 40
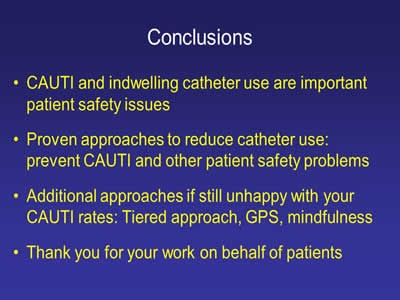
Conclusion
- CAUTI and indwelling catheter use are important patient safety issues
- Proven approaches to reduce catheter use: prevent CAUTI and other patient safety problems
- Additional approaches if still unhappy with your CAUTI rates: Tiered approach, GPS, mindfulness
- Thank you for your work on behalf of patients
Slide 41

Thank you!
www.catheter.org
Slide 42
Funding
Prepared by the Health Research & Educational Trust of the American Hospital Association with contract funding provided by the Agency for Healthcare Research and Quality through the contract, “National Implementation of Comprehensive Unit-based Safety Program (CUSP) to Reduce Catheter-Associated Urinary Tract Infection (CAUTI), project number HHSA290201000025I/HHSA29032001T, Task Order #1.”



