Patient and Family Involvement in Care of Mechanically Ventilated Patients: Slide Presentation
AHRQ Safety Program for Mechanically Ventilated Patients
Slide 1: AHRQ Safety Program for Mechanically Ventilated Patients
Patient and Family Involvement in Care of Mechanically Ventilated Patients
Slide 2: Learning Objectives
After this session, you will be able to—
- Describe the importance of family involvement in the critical care setting.
- Understand the benefits of shared decisionmaking.
- Identify key components of patient-centered care.
- Apply the understanding of basic human needs to improve patient centered care.
Slide 3: Family Involvement

Family Involvement
Slide 4: Why Are You Doing This?
Imagine your mother, father, loved one in a critical care setting. What would you want for them? For you as a family member?
Image: Photograph of a patient in bed with care provider's hand on her shoulder; faces are not shown.
Slide 5: Family Stress in the Intensive Care Unit1
- Family members of patients in the intensive care unit (ICU) may experience fear, anxiety, depression, and post-traumatic stress.
- Nurses and physicians do not always accurately predict the needs of patients’ families.
- Individualized instruction, with proactive assessment of family needs in a manner that promotes the inclusion of patients’ family members in bedside care, may help fulfill the needs of patients’ families and optimize family members’ adaptation to critical illness.
1. Davidson JE. Family-centered care: Meeting the needs of patients’ families and helping families adapt to critical illness. Crit Care Nurse 2009 Jun;29(3):28-34. PMID: 19487778.
Slide 6: What Could Have Improved the Experience?

- What if the nurse had invited you to help?
- What if you built a relationship where you were a trusted member of the health care team?
Image: Photograph of a patient surrounded by smiling caregivers and loved ones in a hospital room.
Slide 7: Development of Family Involvement Menu2-4
- The Family Involvement Menu was developed using results from nurse exercises and family surveys.
- Nursing staff were educated on the availability and intended use of the menu.
- The Family Involvement Menu was displayed on a reusable white board in each patient room to encourage its use.
2. Wyskiel RM, Weeks, K, Marsteller, JA. Inviting families to participate in care: A family involvement menu. Jt Comm J Qual Improv 2015 Jan;41(1):43-6. PMID: 25976723.
3. Mahoney, D. Nurturing a collaborative culture. Partners Oct-Nov 2014. Gordon and Betty Moore Foundation. https://www.moore.org/docs/default-source/default-document-library/nurturing-a-collaborative-culture.pdf?sfvrsn=2. Accessed Aug 26, 2015.
4. Wyskiel RM, Chang BH, Alday AA, et al. Towards expanding the acute care team: learning how to involve families in care processes. Fam Syst Health 2015 Sep;33(3):242-9. PMID: 26148096.
Slide 8: Family Involvement Menu
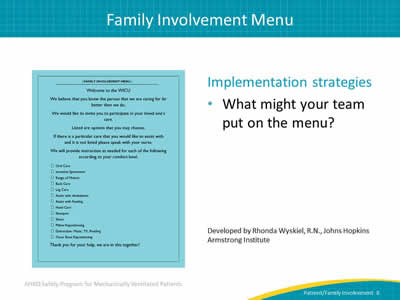
Implementation strategies:
- What might your team put on the menu?
Image: Screen capture of the Family Involvement Menu.
Developed by Rhonda Wyskiel, R.N., Johns Hopkins Armstrong Institute.
Slide 9: Themes of Family Involvement5
- Enacting care:
- Participating in providing care structured around the patient and family member allows family to feel more involved, giving them a focus and purpose.
- Connecting with sick relative:
- Providing care not only helps family members access the patient's world and contribute to their comfort and well-being, it also lets patients feel a personal connection with family members.
- Partnering with nurses:
- The initiative of families providing some care improves communication with the nurses. Communication is an essential element in meeting families’ needs and is therefore of particular importance in a family-centered care initiative.
5. Mitchell M, Chaboyer W. Family centered care—a way to connect patients, families and nurses in critical care: a qualitative study using telephone interviews. Intensive Crit Care Nurs 2010 Jun;26(3):154-60. PMID: 20430621.
Slide 10: Shared Decision Making
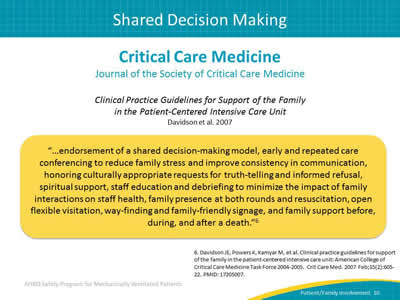
Critical Care Medicine
Journal of the Society of Critical Care Medicine
Clinical Practice Guidelines for Support of the Family in the Patient-Centered Intensive Care Unit, Davidson, et al. 2007.
"…endorsement of a shared decision-making model, early and repeated care conferencing to reduce family stress and improve consistency in communication, honoring culturally appropriate requests for truth-telling and informed refusal, spiritual support, staff education and debriefing to minimize the impact of family interactions on staff health, family presence at both rounds and resuscitation, open flexible visitation, way-finding and family-friendly signage, and family support before, during, and after a death."6
6. Davidson JE, Powers K, Kamyar M, et al. Clinical practice guidelines for support of the family in the patient-centered intensive care unit: American College of Critical Care Medicine Task Force 2004-2005. Crit Care Med 2007 Feb;35(2):605-22. PMID: 17205007.
Slide 11: Remember Your Own Experience
Think back to your initial thought of your mother, father, or loved one in a critical care setting and what you would want for them and for yourself, as a family member.
Remember, promoting family involvement in your ICU can help promote the change we want to see in patient-centered care.
Image: Photograph of man thinking with hand supporting his chin.
Slide 12: Patient-Centered Care

Patient-Centered Care
Slide 13: Empathy Is Important
"I have learned that people will forget what you said, people will forget what you did, but people will never forget how you made them feel."
—Maya Angelou
Image: Photograph of Maya Angelou smiling with her hands clasped.
Slide 14: Patient-Centered Care (PCC)
- A multidimensional approach for improving care.7
- Dimensions include:8-10
- Respecting patient needs, values, and preferences.
- Focusing on the whole person.
- Offering emotional support and alleviating physical discomfort.
- Communicating adequately, sharing information, providing education.
- Strengthening the patient-provider relationship, including family and friends coordinating care across settings.
- Patient engagement and empowerment.
7. Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. Washington, DC: The National Academies Press; 2001.
8. Gerteis M, ed. Through the patient’s eyes: Understanding and promoting patient-centered care. San Francisco, CA: Jossey-Bass; 1993.
9. Davis K, Schoenbaum SC, Audet AM. A 2020 Vision of patient-centered primary care. J Gen Intern Med 2005 Oct;20(10):953-7. PMID: 16191145.
10. Silow-Carroll S, Alteras T, Stepnick L. Patient-centered care for underserved populations: definition and best practices. Prepared by the Economic and Social Research Institute for the W.K. Kellogg Foundation. Washington, DC. January 2006.
Slide 15: What Do You Have in Place Currently?
- What are current PCC practices?
- What PCC practices or behaviors have you witnessed or participated in?
- Any practices/behaviors as either active or passive engagement?
Slide 16: Health System–Level Applications for PCC11
- Patient and family engagement/advisory groups.
- Tailoring of health care documents with consideration for health literacy, language, and cultural competency.
- Visiting hours.
- Services quality.
- Attention to patient-centered outcomes such as quality-of-life measures and patient experience.
- Provision of information on performance measures to consumers.
11. Asha S, Mary CB, Cooper LA. Patient centeredness, cultural competence and healthcare quality. J Natl Med Assoc 2008 Nov;100(11):1275-85. PMID: 19024223.
Slide 17: From the Patient’s Perspective…
…receiving acute care services is a challenging life experience.12-16
- Patients are acutely ill, vulnerable, anxious, and sometimes in pain.
- There are unfamiliar surroundings, and new health care team to interact with and trust.
- There are multiple medical interventions, some with substantial physical discomfort and risk.
- Patients receive directions and information from many people.
Image: Photograph of a female caregiver pushing man in a wheelchair.
12. Levinson W, Shojania KG. Bad experiences in the hospital: the stories keep coming. BMJ Qual Saf 2011 Nov;20(11):911-13. PMID: 21964611.
13. Coulter A, Cleary PD. Patients’ experiences with hospital care in five countries. Health Aff (Millwood) 2001 May-Jun;20(3):244-52. PMID: 11585173.
14. Francis JJ, Pankratz VS, Huddleston JM. Patient satisfaction associated with correct identification of physician's photographs. Mayo Clin Proc 2001 Jun;76(6):604-8. PMID: 11393499.
15. Arora V, Gangireddy S, Mehrotra A, et al. Ability of hospitalized patients to identify their in-hospital physicians. Arch Intern Med 2009 Jan 26;169(2):199-205. PMID: 19171817.
16. Villette M. For want of a four-cent pull chain. BMJ Qual Saf 2011 Nov;20(11):986-90. PMID: 21921089.
Slide 18: Meeting Basic Needs
Patients are very vulnerable in the acute care setting.
Both physical and emotional support are needed. Basic needs include pain control, warmth, food, and sleep.
- Pain control remains a main concern for patients.
- Sleep deprivation can increase morbidity and influence recovery.
- Sleep disturbance in the critical care setting has been associated with prolonged length of stay, increased mechanical ventilation duration, emotional distress, and delirium.
Slide 19: Respect and Dignity17
What does it mean in the critical care setting?
- Treatment with respect and dignity is a foundational aspect of patient- and family-centered care.
- Better understanding of what it encompasses within the critical care setting is needed.
Image: Photograph of a patient in critical care setting.
17. Aboumatar H, Forbes L, Branyon E, et al. Understanding treatment with respect and dignity in the intensive care unit. Narrat Inq Bioeth 2015 5(1A):55A-67A. PMID: 25772730.
Slide 20: Types of Treatment17
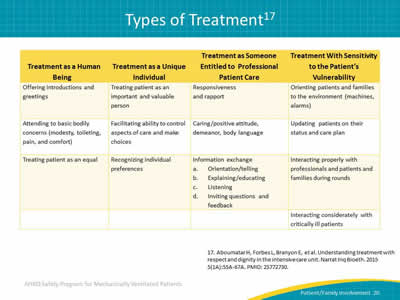
Image: A 4-column chart of types of patient treatment:
Treatment as a Human Being
- Offering introductions and greetings.
- Attending to basic bodily concerns (modesty, toileting, pain, and comfort).
- Treating patient as an equal.
Treatment as a Unique Individual
- Treating patient as an important and valuable person.
- Facilitating ability to control aspects of care and make choices.
- Recognizing individual preferences.
Treatment as Someone Entitled to Professional Patient Care
- Responsiveness and rapport.
- Caring/positive attitude, demeanor, body language.
- Information exchange:
- Orientation/telling.
- Explaining/educating.
- Listening.
- Inviting questions and feedback.
Treatment With Sensitivity to the Patient’s Vulnerability
- Orienting patients and families to the environment (machines, alarms).
- Updating patients on their status and care plan.
- Interacting properly with professionals and patients and families during rounds.
- Interacting considerately with critically ill patients.
17. Aboumatar H, Forbes L, Branyon E, et al. Understanding treatment with respect and dignity in the intensive care unit. Narrat Inq Bioeth 2015 5(1A):55A-67A. PMID: 25772730.
Slide 21: Questions?
Image: Six colored hanging tags with question marks on them.
Slide 22: References
1. Davidson JE. Family-centered care: Meeting the needs of patients’ families and helping families adapt to critical illness. Crit Care Nurse 2009 Jun;29(3):28-34. PMID: 19487778.
2. Wyskiel RM, Weeks, K, Marsteller, JA. Inviting families to participate in care: A family involvement menu. Jt Comm J Qual Improv 2015 Jan;41(1):43-6. PMID: 25976723.
3. Mahoney, D. Nurturing a collaborative culture. Partners Oct-Nov 2014. Gordon and Betty Moore Foundation. https://www.moore.org/docs/default-source/default-document-library/nurturing-a-collaborative-culture.pdf?sfvrsn=2. Accessed Aug 26, 2015.
4. Wyskiel RM, Chang BH, Alday AA, et al. Towards expanding the acute care team: learning how to involve families in care processes. Fam Syst Health 2015 Sep;33(3):242-9. PMID: 26148096.
Slide 23: References
5. Mitchell M, Chaboyer W. Family centered care—a way to connect patients, families and nurses in critical care: a qualitative study using telephone interviews. Intensive Crit Care Nurs 2010 Jun;26(3):154-60. PMID: 20430621.
6. Davidson JE, Powers K, Kamyar M, et al. Clinical practice guidelines for support of the family in the patient-centered intensive care unit: American College of Critical Care Medicine Task Force 2004-2005. Crit Care Med 2007 Feb;35(2):605-22. PMID: 17205007.
7. Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. Washington, DC: The National Academies Press; 2001.
8. Gerteis M, ed. Through the patient’s eyes: Understanding and promoting patient-centered care. San Francisco, CA: Jossey-Bass; 1993.
Slide 24: References

9. Davis K, Schoenbaum SC, Audet AM. A 2020 Vision of patient-centered primary care. J Gen Intern Med 2005 Oct;20(10):953-7. PMID: 16191145.
10. Silow-Carroll S, Alteras T, Stepnick L. Patient-centered care for underserved populations: definition and best practices. Prepared by the Economic and Social Research Institute for the W.K. Kellogg Foundation. Washington, DC. January 2006.
11. Asha S, Mary CB, Cooper LA. Patient centeredness, cultural competence and healthcare quality. J Natl Med Assoc 2008 Nov;100(11):1275-85. PMID: 19024223.
12. Levinson W, Shojania KG. Bad experiences in the hospital: the stories keep coming. BMJ Qual Saf 2011 Nov;20(11):911-13. PMID: 21964611.
13. Coulter A, Cleary PD. Patients’ experiences with hospital care in five countries. Health Aff (Millwood) 2001 May-Jun;20(3):244-52. PMID: 11585173.
Slide 25: References
14. Francis JJ, Pankratz VS, Huddleston JM. Patient satisfaction associated with correct identification of physician's photographs. Mayo Clin Proc 2001 Jun;76(6):604-8. PMID: 11393499.
15. Arora V, Gangireddy S, Mehrotra A, et al. Ability of hospitalized patients to identify their in-hospital physicians. Arch Intern Med 2009 Jan 26;169(2):199-205. PMID: 19171817.
16. Villette M. For want of a four-cent pull chain. BMJ Qual Saf 2011 Nov;20(11):986-90. PMID: 21921089.
17. Aboumatar H, Forbes L, Branyon E, et al. Understanding treatment with respect and dignity in the intensive care unit. Narrat Inq Bioeth 2015 5(1A):55A-67A. PMID: 25772730.



