Science of Safety and Identifying Defects in Care of Mechanically Ventilated Patients: Facilitator Guide
AHRQ Safety Program for Mechanically Ventilated Patients
Slide 1: Science of Safety and Identifying Defects in Care of Mechanically Ventilated Patients
Say:
Today, we will give you an overview of the Science of Safety and identifying defects.
Slide 2: Learning Objectives
Say:
After this session, you will be able to understand and apply the Science of Safety, identify how system factors and design affect patient outcomes, list the principles of safe design and how they apply to both technical work and team work, and recognize the importance of learning from defects within the context of safe design.
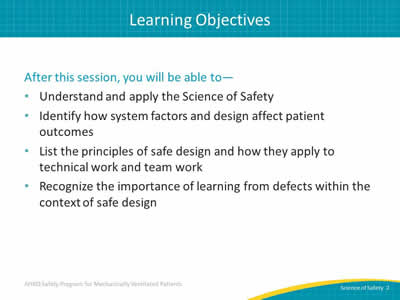
Slide 3: Comprehensive Unit-based Safety Program (CUSP)
Say:
The first step of CUSP involves educating staff on the Science of Safety.
Ask:
Why is this component so critical to the CUSP mission?
Say:
A "system" is a set of parts interacting to achieve a common goal. All too often we assume that patient harm occurs because of inexperience, lack of supervision, or bad luck, when in fact care is delivered in imperfect systems. Clinical area teams must understand the system in which they work to enable change in their clinical setting.
Once these systems are understood, staff will be able to effectively identify system failures that can impact patient safety and apply design approaches that can be used to improve patient safety and quality.
Slide 4: When It Comes to Patient Safety…
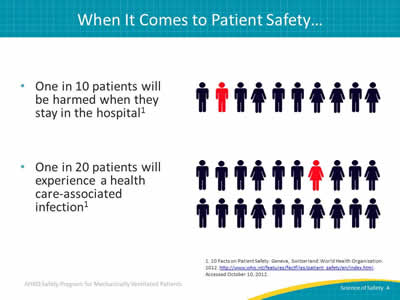
Say:
According to the World Health Organization, we know that 1 in every 10 patients will be harmed during a hospital stay. One in 20 patients will experience a healthcare-associated infection.
Slide 5: Errors Happen Because…
Say:
Errors happen because people are fallible. Often we overlook this fact of human nature, expecting perfection from health care providers. By accepting that people are not perfect, we are taking the first step toward realizing that medical errors, in large part, do not belong to individual providers, but rather are a product of how our health care systems are designed. When we focus on systems rather than individuals, we realize that we can redesign care and delivery processes to improve care and minimize the occurrence of errors and adverse events.
Slide 6: System Factors Impact Safety

Say:
Each level of the health care delivery system matters.
Ask:
What levels can you identify within your health care delivery system?
Say:
The following are all factors that impact safety in the health care system:
- Institutional factors, such as the economic and regulatory state of your organization.
- Hospital factors, such as financial resources and organizational structures.
- Departmental factors, such as staffing levels and managerial support.
- Work environment factors, such as shift patterns and equipment maintenance.
- Team factors, such as team structure and quality of verbal communication.
- Individual provider factors, such as knowledge, skills, and motivations.
- Task factors, such as clarity of structure and accuracy of test results.
- Patient characteristic factors, such as the complexity of their condition, personality, and communication abilities.
Look at each of these system factors and consider how each can carry a defect that leads to patient harms.
Slide 7: Apply System Lenses
Say:
A good way to engage staff is to ask them to apply the systems lenses they are developing to their own work area. Consider asking some of these questions in meetings and during other teachable opportunities.
What are safety events in the clinical area?
What systems may have led to the events?
How can the principles of safe design be applied to prevent future events?
How can staff and others in the clinical area improve communication?
How can these concepts be applied in your unit?
Slide 8: Health Care Is a Science
Say:
When we treat medicine and health care delivery as a science rather than an art, providers can focus on health care delivery processes using evidence-based practices. In order to do this effectively, providers must develop or improve the ability to learn from mistakes and implement procedures that reduce the risk of the future occurrence of errors.
Errors also occur because systems frequently are not designed to catch mistakes before they reach the patient. When we design processes using standardization, such as checklists, and create independent checks for key processes, we improve our ability to reduce the risks of adverse events resulting in harm.
Slide 9: The Science of Safety
Say:
Science of Safety training helps providers recognize that most errors arise from the way our health care systems are organized. A systems thinking approach considers the organization of and interaction between individuals, resources, equipment, information, and other elements as we work toward a goal.
System performance can be improved by understanding the four primary concepts of the Science of Safety:
- Safety is the property of the system. This means that every system is perfectly designed to achieve its end results.
- Standardization, independent checks, and learning from defects are the principles of safe design and should be applied any time we seek to improve system performance.
- Principles of safe design apply to both technical and team work. Not only can we use those principles to improve the technical aspects of our work, such as low tidal volume ventilation strategies or procedures for supporting early mobility measures, we can also apply them to improving team communication and interaction.
- Teams with diverse and independent input have a better ability to make wise decisions.
Slide 10: Understand the Science of Safety Video
Say:
Reinforce key concepts of the Science of Safety by watching this 23-minute Understand the Science of Safety video at—
Slide 11: Safety Is a Property of the System
Say:
Staff will also benefit from reviewing the Science is a Property of the System video, a 4 minute video that can be found at—
Slide 12: Three Principles of Safe Design
Say:
The three principles of safe design are standardize when you can, create independent checks, and learn from defects. To make sure your team understands these principles, here are three short videos which explain more about these concepts.
Standardize When You Can:
http://www.ahrq.gov/professionals/education/curriculum-tools/cusptoolkit/videos/04c_standardize/index.html
Create Independent Checks:
http://www.ahrq.gov/professionals/education/curriculum-tools/cusptoolkit/videos/04d_indchecks/index.html
Learn From Defects:
http://www.ahrq.gov/professionals/education/curriculum-tools/cusptoolkit/videos/04e_learndefects/index.html
Slide 13: Principles of Safe Design Apply to Technical Work and Teamwork
Say:
We know the principles of safe design apply to both technical work and teamwork. This brief video reinforces this idea by emphasizing how these principles can improve safety efforts and can be found here:
Slide 14: Teams Make Wise Decisions When There Is Diverse and Independent Input
Say:
We also know that teams have a better ability to make wise decisions with diverse and independent input. This video demonstrates the value of having diverse and independent input through the course of your quality improvement efforts and can be found here:
Slide 15: Identify Defects
Say:
The second step of CUSP is to proactively identify defects within your organization.
Slide 16: Where To Find Defects

Say:
Some defects make themselves very apparent, but others can be harder to discover. You can find defects in many places. Adverse event reporting systems are common in hospitals. Sentinel events, as defined by the Joint Commission, or any claims data from your legal department provide high-profile defects. Infection rates from hospital epidemiology and infection prevention also present known complications.
Ask:
But, what is the most effective way to identify defects, particularly in a localized environment like the intensive care unit and also empowers your frontline providers?
Say:
Just ask them! You can use the Staff Safety Assessment to compile information on defects from the frontline staff.
Slide 17: Staff Safety Assessment
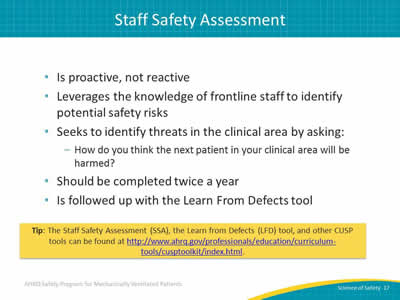
Say:
Adverse reporting systems, sentinel events, and claims data are reactive—the unfortunate event has already occurred. The Staff Safety Assessment, on the other hand, is proactive. It asks frontline providers to think ahead and taps into their wisdom to prevent patient harm from happening. By leveraging staff member knowledge, the Staff Safety Assessment allows teams to determine risks that have jeopardized or could jeopardize patient safety on a unit. The assessment seeks to identify threats in the clinical area by asking, "How do you think the next patient in your clinical area will be harmed?"
Ask:
Why is staff member knowledge so valuable?
Say:
Frontline staff members are the eyes and ears of patient safety. They can list valid improvement opportunities and focus your safety program activities through use of the Staff Safety Assessment. The Staff Safety Assessment provides insight into potential solutions and leverages that all-important frontline wisdom to guide patient safety efforts.
We recommend asking staff to complete the SSA at least every 6 months and follow up on your findings with the Learning from Defects tool.
Slide 18: Questions
Slide 19: References