Science of Safety and Identifying Defects in Care of Mechanically Ventilated Patients: Slide Presentation
AHRQ Safety Program for Mechanically Ventilated Patients
Slide 1: AHRQ Safety Program for Mechanically Ventilated Patients
Science of Safety and Identifying Defects in Care of Mechanically Ventilated Patients
Slide 2: Learning Objectives
After this session, you will be able to—
- Understand and apply the Science of Safety.
- Identify how system factors and design affect patient outcomes.
- List the principles of safe design and how they apply to technical work and team work.
- Recognize the importance of learning from defects within the context of safe design.
Slide 3: Comprehensive Unit-based Safety Program (CUSP)
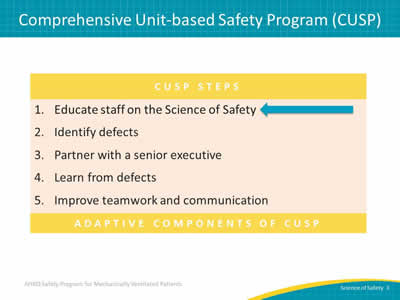
Image: Chart shows the CUSP Steps:
- Educate staff on the Science of Safety.
- Identify defects.
- Partner with a senior executive.
- Learn from defects.
- Improve teamwork and communication.
Adaptive components of CUSP.
Slide 4: When It Comes to Patient Safety…
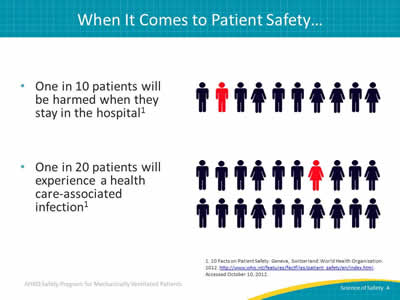
One in 10 patients will be harmed when they stay in the hospital1
One in 20 patients will experience a health care-associated infection1
Images: One in 10: Line of 10 figures representing both men and women with one highlighted in red. One in 20: Line of 20 figures representing both men and women with one highlighted in red.
1. 10 Facts on Patient Safety. Geneva, Switzerland: World Health Organization. 2012. http://www.who.int/features/factfiles/patient_safety/en/index.html. Accessed October 10, 2012.
Slide 5: Errors Happen Because…
- People are fallible:
- We expect providers to be perfect.
- We focus on individuals as opposed to systems:
- Most errors do not belong to individual doctors and nurses.
- Health care systems are rarely designed to catch mistakes before they happen.
Slide 6: System Factors Impact Safety2

Image: A series of small circles around a larger circle captioned Safety shows that many system factors impact safety: institutional, hospital, departmental, work environment, teams, individual providers, tasks, and patient characteristics.
2. Vincent C, Taylor-Adams S, Stanhope N. Framework for analyzing risk and safety in clinical medicine. BMJ 1998 Apr 11;316(7138):1154-7. PMID: 9552960.
Slide 7: Apply System Lenses
Engage staff by asking them to apply systems lenses with the following questions:
- What are safety events in the clinical area?
- What systems may have led to these events?
- How can the principles of safe design be applied to prevent future events?
- How can staff and others in the clinical area improve communication?
- How can these concepts be applied in your unit?
Slide 8: Health Care Is a Science
- Health care delivery should be viewed as a science, not an art:
- Focus on evidence-based practices when evaluating the delivery process.
- Processes should be designed using standardization:
- Checklists.
- Independent checks for key processes.
Image: Clipboard with checklist and a stethoscope laying on top.
Slide 9: The Science of Safety2,3
Four primary concepts of the Science of Safety:
- Safety is the property of the system—every system is perfectly designed to achieve its end results.
- Standardization, independent checks, and learning from defects are the principles of safe design.
- Principles of safe design apply to both technical and team work.
- Teams with diverse and independent input make wise decisions.
2. Vincent C, Taylor-Adams S, Stanhope N. Framework for analyzing risk and safety in clinical medicine. BMJ 1998 Apr 11;316(7138):1154-7. PMID: 9552960.
3. Pronovost PJ, Holzmueller CG, Martinez E, et al. A practical tool to learn from defects in patient care. Jt Comm J Qual Patient Saf 2006 Feb;32(2):102-8. PMID: 16568924.
Slide 10: Understand the Science of Safety Video
Find the Understand the Science of Safety video (23 min) at www.ahrq.gov/professionals/education/curriculum-tools/cusptoolkit/videos/04a_scisafety/index.html
Image: Line of snapshots from video featuring frontline medical staff.
Slide 11: Safety Is a Property of the System
- Safety Is a Property of the System
http://www.ahrq.gov/professionals/education/curriculum-tools/cusptoolkit/videos/04b_safeproperty/index.html
Slide 12: Three Principles of Safe Design
- Standardize When You Can
http://www.ahrq.gov/professionals/education/curriculum-tools/cusptoolkit/videos/04c_standardize/index.html - Create Independent Checks
http://www.ahrq.gov/professionals/education/curriculum-tools/cusptoolkit/videos/04d_indchecks/index.html - Learn From Defects
http://www.ahrq.gov/professionals/education/curriculum-tools/cusptoolkit/videos/04e_learndefects/index.html
Slide 13: Principles of Safe Design Apply to Technical Work and Teamwork
- Principles of Safe Design Apply to Technical and Teamwork
http://www.ahrq.gov/professionals/education/curriculum-tools/cusptoolkit/videos/04f_techtmwork/index.html
Slide 14: Teams Make Wise Decisions When There Is Diverse and Independent Input
- Teams Make Wise Decisions With Diverse and Independent Input
http://www.ahrq.gov/professionals/education/curriculum-tools/cusptoolkit/videos/04g_diverseinput/index.html
Slide 15: Identify Defects
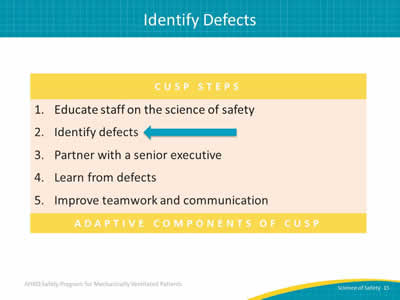
Image: Chart shows the CUSP Steps:
- Educate staff on the Science of Safety.
- Identify defects.
- Partner with a senior executive.
- Learn from defects.
- Improve teamwork and communication.
Adaptive components of CUSP.
Slide 16: Where To Find Defects

- Adverse event reporting systems.
- Sentinel events.
- Claims data.
- Infection rates.
- Complications.
- Staff Safety Assessments.
Image: Close-up photograph of two hands holding and using an iPad to review data charts.
Slide 17: Staff Safety Assessment
- Is proactive, not reactive.
- Leverages the knowledge of frontline staff to identify potential safety risks.
- Seeks to identify threats in the clinical area by asking:
- How do you think the next patient in your clinical area will be harmed?
- Should be completed twice a year.
- Is followed up with the Learn From Defects tool.
Tip: The Staff Safety Assessment (SSA), the Learn from Defects (LFD) tool, and other CUSP tools can be found at http://www.ahrq.gov/professionals/education/curriculum-tools/cusptoolkit/index.html.
Slide 18: Questions
Image: Multicolored hanging tags with question marks.
Slide 19: References
1. 10 Facts on Patient Safety. Geneva, Switzerland: World Health Organization. 2012. http://www.who.int/features/factfiles/patient_safety/en/index.html. Accessed October 10, 2012.
2. Vincent C, Taylor-Adams S, Stanhope N. Framework for analyzing risk and safety in clinical medicine. BMJ 1998 Apr 11;316(7138):1154-7. PMID: 9552960.
3. Pronovost PJ, Holzmueller CG, Martinez E, et al. A practical tool to learn from defects in patient care. Jt Comm J Qual Patient Saf 2006 Feb;32(2):102-8. PMID: 16568924.



