Low Tidal Volume Ventilation: Introduction, Evidence, and Implementation: Slide Presentation
AHRQ Safety Program for Mechanically Ventilated Patients
Slide 1: AHRQ Safety Program for Mechanically Ventilated Patients
Low Tidal Volume Ventilation: Introduction, Evidence, and Implementation
Slide 2: Learning Objectives
After this session, you will be able to—
- Explain why we should use low tidal volume ventilation (LTVV).
- Outline the historical background and scientific evidence supporting the use of LTVV.
- Implement recommended standards for LTVV.
Slide 3: What is Low Tidal Volume Ventilation?
- Low tidal volume ventilation is a lung protective strategy that seeks to prevent ventilator-associated lung injury.
- LTVV is an approach that targets much lower tidal volume than what has been traditionally used.
- LTVV also focuses on the avoidance of zero positive end-expiratory pressure (ZEEP).
Slide 4: What are the goals of LTVV?
- Target tidal volume of 6–8 mL/kg of predicted body weight (PBW) for patients without ARDS and 4–6 mL/kg PBW for patients with ARDS:
- Predicted body weight based on height/sex.
- Not ideal body weight.
- Not actual body weight
- Avoid the use of ZEEP:
- Use positive end-expiratory pressure (PEEP) settings ≥ 5 cm H20.
Slide 5: Why Should We Use LTVV?
- Significant benefit when outcomes are compared using lower volumes (6 cc/kg) versus traditional tidal volumes (12 cc/kg).1
- Additional studies and meta-analysis showed large tidal ventilation and the resulting high pressures were harmful.
1. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network. N Engl J Med 2000 342(18):1301-8. PMID: 10793162.
Slide 6: Why Should We Use LTVV?
Low tidal volume ventilation protects lungs by—
- Preventing "volutrauma" (overdistension of some alveoli areas and underdistension in other areas).
- Preventing barotrauma.
- Preventing development of acute respiratory distress syndrome (ARDS).
- Suppressing activation of chemical inflammatory mediators.
- Improving outcomes.
Slide 7: AHRQ Safety Program for Mechanically Ventilated Patients
History Review
Slide 8: Early History
- 1776: Dr. John Hunter developed a double bellows system that pushed and pulled air in and out of lung; used on dogs with tubes going into trachea.
- 1837: Efforts like Hunter’s lost favor as chest compressions became preferred method for moving air (not same as CPR).
- Both positive and negative pressure systems continued to be developed.
- 1850: French Academy of Sciences reported that positive pressure caused what we now know as barotrauma, which may result in pneumothorax, rupture of alveoli, and emphysema.
Slide 9: The Iron Lung
Negative pressure ventilation became the most common approach, ultimately resulting in the iron lung.
Image: Photograph of room full of many iron lungs and nurses assisting the patients in them.
Slide 10: Positive Pressure Vents Still Progressed
Johann Dräger developed the portable Pulmotor in 1907.
By 1909, the Pulmotor was a top seller for his company.
Image: Photograph of doctor using a portable pulmotor on a patient lying on the ground.
Slide 11: Endotracheal Intubation
- Uncommon and considered inappropriate outside of the operating room (OR).
- Polio epidemics in the 1950s outstripped the supply of iron lungs, returning attention to the use of positive-pressure ventilation (PPV) in other settings.
- Soon the transition to endotracheal tubes in conjunction with PPV outside the OR accelerated.
Slide 12: 1950s
- Despite progress, ventilators were still crude.
- Difficult to precisely control volume and pressure.
- Two primary modes were used:
- Volume regulated.
- Pressure limited.
Slide 13: Ventilator Progress
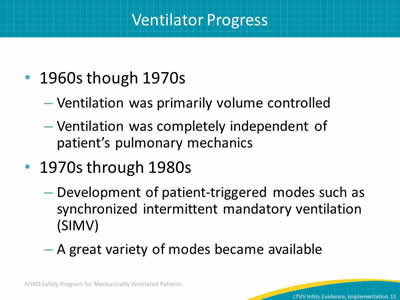
- 1960s though 1970s:
- Ventilation was primarily volume controlled.
- Ventilation was completely independent of patient’s pulmonary mechanics.
- 1970s through 1980s:
- Development of patient-triggered modes such as synchronized intermittent mandatory ventilation (SIMV).
- A great variety of modes became available.
Slide 14: AHRQ Safety Program for Mechanically Ventilated Patients

Supporting Research
Slide 15: Common Ventilator Modes
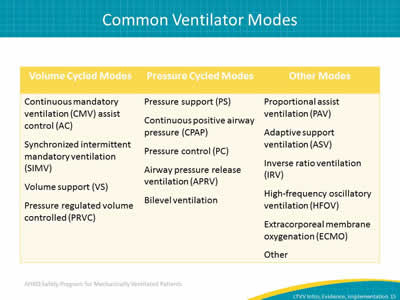
Image: Table showing the most common modes for mechanical ventilation.
Slide 16: The Basis for Traditional Ventilation Strategies
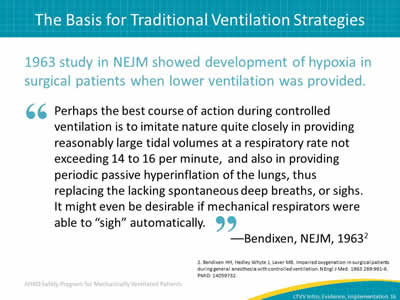
1963 study in NEJM showed development of hypoxia in surgical patients when lower ventilation was provided.
"Perhaps the best course of action during controlled ventilation is to imitate nature quite closely in providing reasonably large tidal volumes at a respiratory rate not exceeding 14 to 16 per minute, and also in providing periodic passive hyperinflation of the lungs, thus replacing the lacking spontaneous deep breaths, or sighs. It might even be desirable if mechanical respirators were able to 'sigh' automatically."
—Bendixon, NEJM, 19632
2. Bendixen HH, Hedley Whyte J, Laver MB. Impaired oxygenation in surgical patients during general anesthesia with controlled ventilation. N Engl J Med 1963 269:991-6. PMID: 14059732.
Slide 17: Traditional Ventilation Strategies
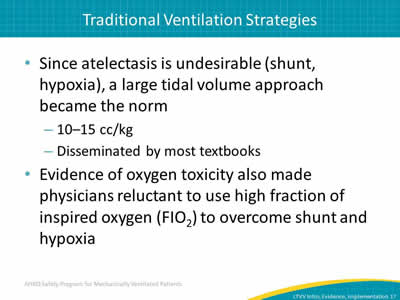
- Since atelectasis is undesirable (shunt, hypoxia), a large tidal volume approach became the norm:
- 10–15 cc/kg.
- Disseminated by most textbooks.
- Evidence of oxygen toxicity also made physicians reluctant to use high fraction of inspired oxygen (FIO2) to overcome shunt and hypoxia.
Slide 18: The Problem With Large Tidal Volumes (Vt)
Acute lung injury (ALI):
- Involves a breakdown in lung architecture and capillary leak.
- Leads to stiff lungs with areas of over- and underinflation.
Large Vt:
- Results in overdistension of some areas resulting in "volutrauma," which is considered a major cause of ventilator-associated lung injury.
- Leads to inflammatory responses that further damage the lung(s).
Slide 19: The Problem With Large Tidal Volumes (Vt)
It’s clear that commonly used tidal volumes were injurious to the lung.
- Can also lead to barotrauma:
- Rupture of alveoli.
- Pneumothorax.
- Some airspaces collapse, then reopen cyclically.
- Shear stresses as alveoli close and "pop" open.
Researchers proposed using lower tidal volumes and allowing mild to moderate respiratory acidosis to improve outcomes.
Slide 20: ARDSNet: Probability of Survival and Discharged Home1
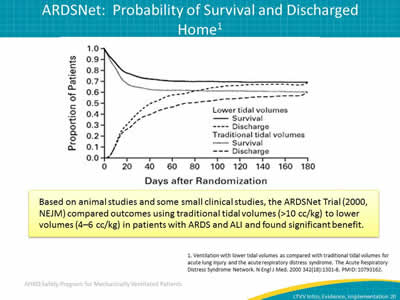
Based on animal studies and some small clinical studies, the ARDSNet Trial (2000, NEJM) compared outcomes using traditional tidal volumes (>10 cc/kg) to lower volumes (4–6 cc/kg) in patients with ARDS and ALI and found significant benefit.
Image: Graph showing the probability of survival and home discharge from ARDSNet research.
1. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network. N Engl J Med 2000 342(18):1301-8. PMID: 10793162.
Slide 21: Primary Findings1
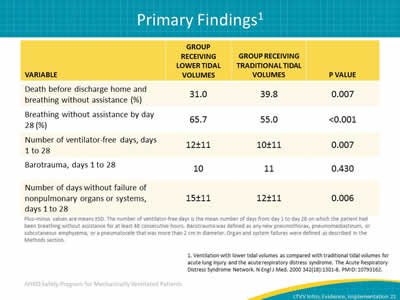
Image: The ARDSNET Trial showed statistically improved mortality, being off of the ventilator by day 28 and the number of ventilator free days when a LTVV strategy was used. They also found other organ systems besides the lungs benefited as well.
Plus–minus values are means ±SD. The number of ventilator-free days is the mean number of days from day 1 to day 28 on which the patient had been breathing without assistance for at least 48 consecutive hours. Barotrauma was defined as any new pneumothorax, pneumomediastinum, or subcutaneous emphysema, or a pneumatocele that was more than 2 cm in diameter. Organ and system failures were defined as described in the Methods section.
1. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network. N Engl J Med 2000 342(18):1301-8. PMID: 10793162.
Slide 22: LTVV in ARDS
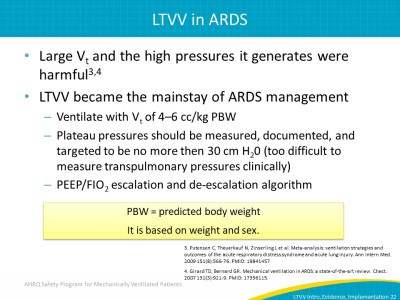
- Large Vt and the high pressures it generates were harmful3,4
- LTVV became the mainstay of ARDS management:
- Ventilate with Vt of 4–6 cc/kg PBW.
- Plateau pressures should be measured, documented and targeted to be no more then 30 cm H20 (too difficult to measure transpulmonary pressures clinically).
- PEEP/FIO2 escalation and de-escalation algorithm.
PBW = predicted body weight.
It is based on weight and sex.
3. Putensen C, Theuerkauf N, Zinserling J, et al. Meta-analysis: ventilation strategies and outcomes of the acute respiratory distress syndrome and acute lung injury. Ann Intern Med 2009 151(8):566-76. PMID: 19841457.
4. Girard TD, Bernard GR. Mechanical ventilation in ARDS: a state-of-the-art review. Chest 2007 131(3):921-9. PMID: 17356115.
Slide 23: Beyond ARDS? Emerging Evidence5
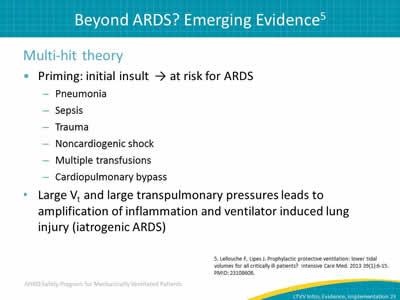
Multi-hit theory:
- Priming: initial insult → at risk for ARDS:
- Pneumonia.
- Sepsis.
- Trauma.
- Noncardiogenic shock.
- Multiple transfusions.
- Cardiopulmonary bypass.
- Large Vt and large transpulmonary pressures leads to amplification of inflammation and ventilator induced lung injury (iatrogenic ARDS).
5. Lellouche F, Lipes J. Prophylactic protective ventilation: lower tidal volumes for all critically ill patients? Intensive Care Med 2013 39(1):6-15. PMID: 23108608.
Slide 24: Beyond ARDS? Emerging Evidence5
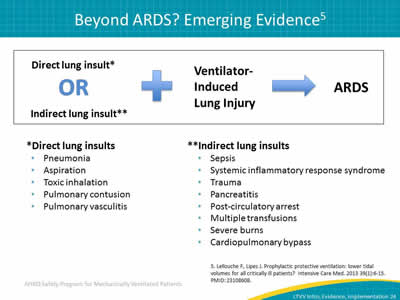
Direct lung insult* or Indirect lung insult** + ventilator-induced lung injury = ARDS
*Direct lung insults:
- Pneumonia.
- Aspiration.
- Toxic inhalation.
- Pulmonary contusion.
- Pulmonary vasculitis.
**Indirect lung insults:
- Sepsis.
- Systemic inflammatory response syndrome.
- Trauma.
- Pancreatitis.
- Post-circulatory arrest.
- Multiple transfusions.
- Severe burns.
- Cardiopulmonary bypass.
5. Lellouche F, Lipes J. Prophylactic protective ventilation: lower tidal volumes for all critically ill patients? Intensive Care Med 2013 39(1):6-15. PMID: 23108608.
Slide 25: ICU Patient Results5 (Qualitative Systematic Review)
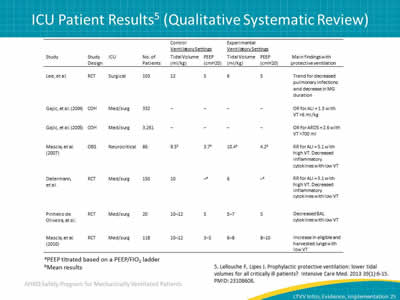
Image: Table showing results from a qualitative systematic review.
5. Lellouche F, Lipes J. Prophylactic protective ventilation: lower tidal volumes for all critically ill patients? Intensive Care Med 2013 39(1):6-15. PMID: 23108608.
Slide 26: Meta-analysis of LTVV in Patients Without Lung Injury6
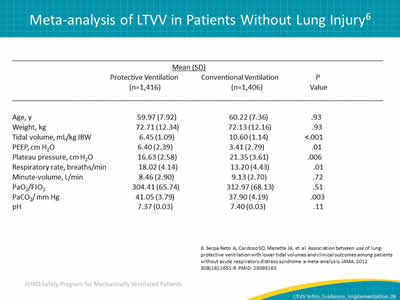
Image: Table showing results of a meta-analysis of protective vs conventional ventilation in patients without lung injury.
6. Serpa Neto A, Cardoso SO, Manetta JA, et al. Association between use of lung-protective ventilation with lower tidal volumes and clinical outcomes among patients without acute respiratory distress syndrome: a meta-analysis. JAMA 2012 308(16):1651-9. PMID: 23093163.
Slide 27: LTVV in Patients Without Lung Injury6
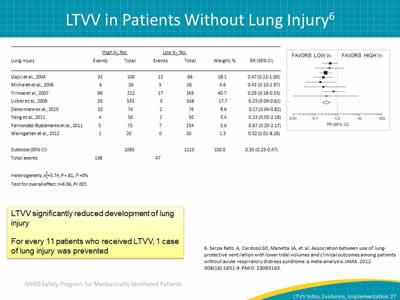
Image: Forest plot showing LTVV significantly reduced development of Lung Injury.
LTVV significantly reduced development of lung injury.
For every 11 patients who received LTVV, one case of lung injury was prevented.
6. Serpa Neto A, Cardoso SO, Manetta JA, et al. Association between use of lung-protective ventilation with lower tidal volumes and clinical outcomes among patients without acute respiratory distress syndrome: a meta-analysis. JAMA 2012 308(16):1651-9. PMID: 23093163.
Slide 28: LTVV in Patients Without Lung Injury6
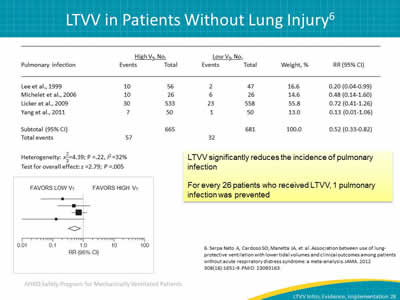
Images: Table showing LTVV significantly reduces the incidence of pulmonary infection. Forest plot showing LTVV significantly reduces the incidence of pulmonary infection.
LTVV significantly reduces the incidence of pulmonary infection.
For every 26 patients who received LTVV, on pulmonary infection was prevented.
6. Serpa Neto A, Cardoso SO, Manetta JA, et al. Association between use of lung-protective ventilation with lower tidal volumes and clinical outcomes among patients without acute respiratory distress syndrome: a meta-analysis. JAMA 2012 308(16):1651-9. PMID: 23093163.
Slide 29: LTVV in Patients Without Lung Injury6
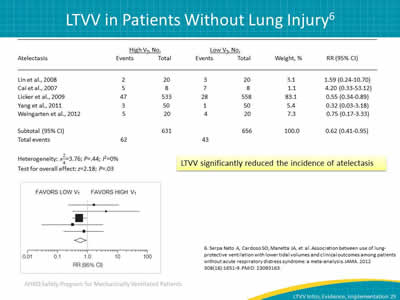
Images: Table showing LTVV significantly reduced the incidence of atelectasis. Forest plot showing LTVV significantly reduced the incidence of atelectasis.
LTVV significantly reduced the incidence of atelectasis.
6. Serpa Neto A, Cardoso SO, Manetta JA, et al. Association between use of lung-protective ventilation with lower tidal volumes and clinical outcomes among patients without acute respiratory distress syndrome: a meta-analysis. JAMA 2012 308(16):1651-9. PMID: 23093163.
Slide 30: LTVV in Patients Without Lung Injury6
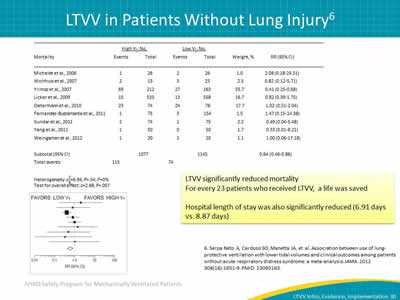
Image: Table showing the mortality events associated with high vs. low tidal volumes. Forest plot showing LTVV significantly reduced Mortality.
LTVV significantly reduced mortality.
For every 23 patients who received LTVV, a life was saved.
Hospital length of stay was also significantly reduced (6.91 days vs. 8.87 days).
6. Serpa Neto A, Cardoso SO, Manetta JA, et al. Association between use of lung-protective ventilation with lower tidal volumes and clinical outcomes among patients without acute respiratory distress syndrome: a meta-analysis. JAMA 2012 308(16):1651-9. PMID: 23093163.
Slide 31: Focusing on ICU Patients Only
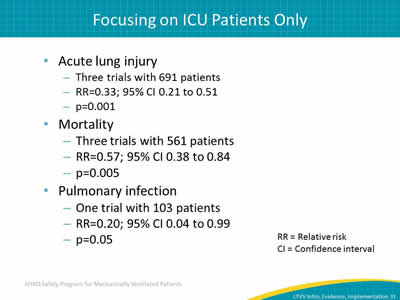
- Acute lung injury:
- Three trials with 691 patients.
- RR = 0.33; 95% CI 0.21 to 0.51.
- p = 0.001.
- Mortality:
- Three trials with 561 patients. RR = 0.57; 95% CI 0.38 to 0.84.
- p = 0.005.
- Pulmonary infection:
- One trial with 103 patients.
- RR = 0.20; 95% CI 0.04 to 0.99.
- p = 0.05.
RR = Relative risk.
CI = Confidence interval
Slide 32: Quality Gap
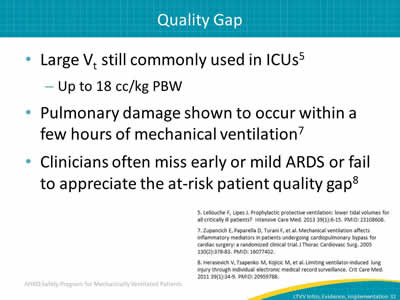
- Large Vt still commonly used in ICUs:5
- Up to 18 cc/kg PBW.
- Pulmonary damage shown to occur within a few hours of mechanical ventilation.7
- Clinicians often miss early or mild ARDS or fail to appreciate the at-risk patient quality gap.8
5. Lellouche F, Lipes J. Prophylactic protective ventilation: lower tidal volumes for all critically ill patients? Intensive Care Med 2013 39(1):6-15. PMID: 23108608.
7. Zupancich E, Paparella D, Turani F, et al. Mechanical ventilation affects inflammatory mediators in patients undergoing cardiopulmonary bypass for cardiac surgery: a randomized clinical trial. J Thorac Cardiovasc Surg 2005 130(2):378-83. PMID: 16077402.
8. Herasevich V, Tsapenko M, Kojicic M, et al. Limiting ventilator-induced lung injury through individual electronic medical record surveillance. Crit Care Med 2011 39(1):34-9. PMID: 20959788.
Slide 33: AHRQ Safety Program for Mechanically Ventilated Patients
Low Tidal Volume Implementation
Slide 34: Preemption
- Why wait?
- Why not initiate LTVV on all patients to minimize risk?
- Too late once ARDS/ALI criteria are met.
- A few hours of mechanical ventilation with large Vt may start the cascade.
Image: Photograph of train leaving station.
Slide 35: Low Tidal Volume Implementation9
- A 2013 study reviewed patients undergoing relatively major abdominal surgery and receiving mechanical ventilation for between 4 and 5 hours.
- Patients who received a low tidal volume strategy using PEEP settings had statistically significant improvements in a variety of parameters when compared to standard tidal ventilations:
- Postoperative complications.
- Pulmonary complications.
- Length of stay.
9. Furtier E, Constantin JM, Paugam-Burtz C, et al. A trial of intraoperative low-tidal-volume ventilation in abdominal surgery. N Eng J Med 2013 Aug 1;369(5):428-37. PMID: 23902482.
Slide 36: Low Tidal Volume Implementation
- Patients at risk of ARDS should be ventilated with a Vt of 6–8 ml/kg PBW.
- Tidal volumes of this size eliminate most hypercarbia.
Slide 37: Use PBW Rather Than ABW
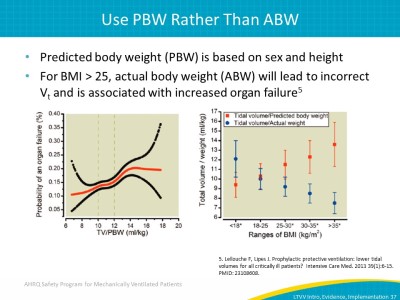
- Predicted body weight (PBW) is based on sex and height.
- For BMI > 25, actual body weight (ABW) will lead to incorrect Vt and is associated with increased organ failure.5
Images: Graph showing the probability of an organ failure. Box plot showing the probability of an organ failure.
5. Lellouche F, Lipes J. Prophylactic protective ventilation: lower tidal volumes for all critically ill patients? Intensive Care Med 2013 39(1):6-15. PMID: 23108608.
Slide 38: What about Positive End-Expiratory Pressure?
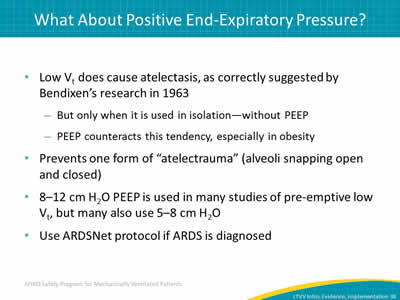
- Low Vt does cause atelectasis, as correctly suggested by Bendixen’s research in 1963:
- But only when it is used in isolation—without PEEP.
- PEEP counteracts this tendency, especially in obesity.
- Prevents one form of "atelectrauma" (alveoli snapping open and closed).
- 8–12 cm H2O PEEP is used in many studies of pre-emptive low Vt, but many also use 5–8 cm H2O.
- Use ARDSNet protocol if ARDS is diagnosed.
Slide 39: What about PEEP?
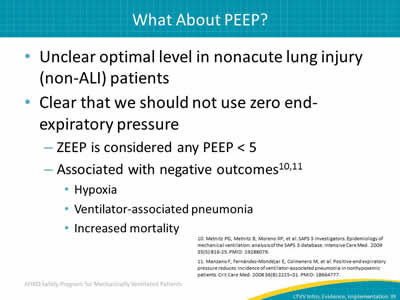
- Unclear optimal level in nonacute lung injury (non-ALI) patients.
- Clear that we should not use zero end-expiratory pressure:
- ZEEP is considered any PEEP <5.
- Associated with negative outcomes:10,11
- Hypoxia.
- Ventilator-associated pneumonia.
- Increased mortality.
10. Metnitz PG, Metnitz B, Moreno RP, et al. SAPS 3 Investigators. Epidemiology of mechanical ventilation: analysis of the SAPS 3 database. Intensive Care Med 2009 35(5):816-25. PMID: 19288079.
11. Manzano F, Fernández-Mondéjar E, Colmenero M, et al. Positive-end expiratory pressure reduces incidence of ventilator-associated pneumonia in nonhypoxemic patients. Crit Care Med 2008 36(8):2225–31. PMID: 18664777.
Slide 40: Respiratory Rate
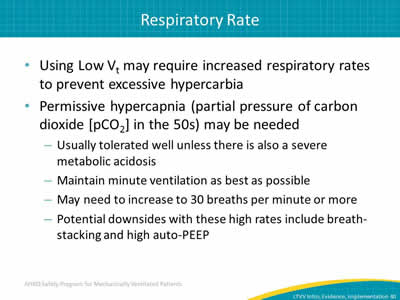
- Using Low Vt may require increased respiratory rates to prevent excessive hypercarbia.
- Permissive hypercapnia (partial pressure of carbon dioxide [pCO2] in the 50s) may be needed:
- Usually tolerated well unless there is also a severe metabolic acidosis.
- Maintain minute ventilation as best as possible.
- May need to increase to 30 breaths per minute or more.
- Potential downsides with these high rates include breath-stacking and high auto-PEEP.
Slide 41: Plateau Pressure
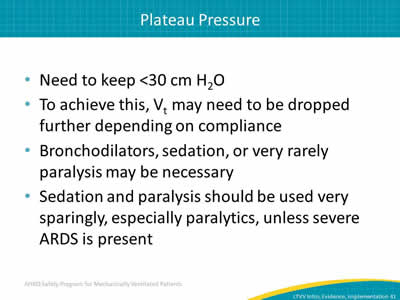
- Need to keep <30 cm H2O.
- To achieve this, Vt may need to be dropped further depending on compliance.
- Bronchodilators, sedation, or very rarely paralysis may be necessary.
- Sedation and paralysis should be used very sparingly, especially paralytics, unless severe ARDS present.
Slide 42: Barriers to Low Vt Implementation
- Translation of evidence into practice is difficult.
- Only 46% of eligible ARDS patients received LTVV 8 years after ARDSNet trial.12
- Application to non-ALI patients is not well known, but likely much lower nationally.
12. Umoh NJ, Fan E, Mendez-Tellez PA, et al. Patient and intensive care unit organizational factors associated with low tidal volume ventilation in acute lung injury. Crit Care Med 2008 36(5):1463-8. PMID: 18434907.
Slide 43: Address Variability in Practice
- Do you have a standardized protocol?
- If a provider orders settings outside of LTVV strategy parameters, is a change to the order required?
- How is the order modified?
- Do your providers comply with protocols?
Slide 44: Steps to Implementing a LTVV Strategy
- Educate staff on LTVV strategy.
- Identify inconsistencies in prescriber engagement or agreement.
- Garner buy-in from all providers:
- Address and work with dissenters.
- Develop standard protocol.
- Employ default strategy that encourages LTVV.
Slide 45: Protocol
- Standardize protocol:
- Electronic health record.
- Paper.
- Assign custodian of process:
- Respiratory therapist.
- Physician.
- Include tools to support or reinforce expectation.
- Add system redundancies.
Slide 46: Closing Gaps in Quality
- Audit your intervention practices.
- Review LTVV data:
- LTVV Data Collection tool.
Tip: The LTVV Data Collection tool can be found at https://www.ahrq.gov/professionals/quality-patient-safety/hais/tools/mvp/modules/technical/daily-ltvv-tool.html.
Slide 47: Summary
- Low tidal volume ventilation:
- Beneficial for patients with ALI.
- Data also suggest it is beneficial in non-ALI ICU patients.
- Current recommendations.
- Target Vt 6–8 mL/Kg (or less if ARDS).
- PEEP ≥ 5 cm H2O.
Slide 48: LTVV Quick Reference for Tidal Volume
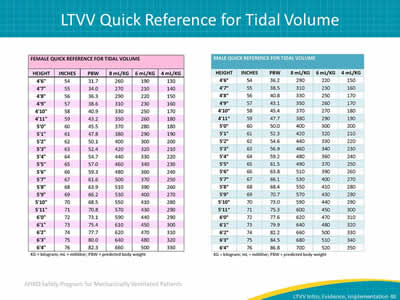
Images: Female Guide Reference for Tidal Volume and Male Guide Reference for Tidal Volume.
Slide 49: Questions?
Image: Picture of hanging multicolored tags with question marks on them.
Slide 50: References
1. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network. N Engl J Med 2000 342(18):1301-8. PMID: 10793162.
2. Bendixen HH, Hedley Whyte J, Laver MB. Impaired oxygenation in surgical patients during general anesthesia with controlled ventilation. N Engl J Med 1963 269:991-6. PMID: 14059732.
3. Putensen C, Theuerkauf N, Zinserling J, et al. Meta-analysis: ventilation strategies and outcomes of the acute respiratory distress syndrome and acute lung injury. Ann Intern Med 2009 151(8):566-76. PMID: 19841457.
4. Girard TD, Bernard GR. Mechanical ventilation in ARDS: a state-of-the-art review. Chest 2007 131(3):921-9. PMID: 17356115.
Slide 51: References
5. Lellouche F, Lipes J. Prophylactic protective ventilation: lower tidal volumes for all critically ill patients? Intensive Care Med 2013 39(1):6-15. PMID: 23108608.
6. Serpa Neto A, Cardoso SO, Manetta JA, et al. Association between use of lung-protective ventilation with lower tidal volumes and clinical outcomes among patients without acute respiratory distress syndrome: a meta-analysis. JAMA 2012 308(16):1651-9. PMID: 23093163.
7. Zupancich E, Paparella D, Turani F, et al. Mechanical ventilation affects inflammatory mediators in patients undergoing cardiopulmonary bypass for cardiac surgery: a randomized clinical trial. J Thorac Cardiovasc Surg 2005 130(2):378-83. PMID: 16077402.
8. Herasevich V, Tsapenko M, Kojicic M, et al. Limiting ventilator-induced lung injury through individual electronic medical record surveillance. Crit Care Med 2011 39(1):34-9. PMID: 20959788.
Slide 52: References
9. Furtier E, Constantin JM, Paugam-Burtz C, et al. A trial of intraoperative low-tidal-volume ventilation in abdominal surgery. N Eng J Med 2013 Aug 1;369(5):428-37. PMID: 23902482.
10. Metnitz PG, Metnitz B, Moreno RP, et al. SAPS 3 Investigators. Epidemiology of mechanical ventilation: analysis of the SAPS 3 database. Intensive Care Med 2009 35(5):816-25. PMID: 19288079.
11. Manzano F, Fernández-Mondéjar E, Colmenero M, et al. Positive-end expiratory pressure reduces incidence of ventilator-associated pneumonia in nonhypoxemic patients. Crit Care Med 2008 36(8):2225–31. PMID: 18664777.
12. Umoh NJ, Fan E, Mendez-Tellez PA, et al. Patient and intensive care unit organizational factors associated with low tidal volume ventilation in acute lung injury. Crit Care Med 2008 36(5):1463-8. PMID: 18434907.



