Implementing Your Surgical Site Infection Prevention Bundle: Slide Presentation
AHRQ Safety Program for Surgery
Slide 1: AHRQ Safety Program for Surgery—Implementation
Implementing Your Surgical Site Infection Prevention Bundle
Slide 2: Learning Objectives
After this session, you will be able to–
- Develop an implementation plan for your surgical site infection (SSI) prevention bundle.
- Identify and address local barriers to implementing your SSI prevention bundle.
- Use the Barrier Identification and Mitigation (BIM) tool.
Slide 3: SSI Bundle Characteristics1,2,3
- A collection of evidence-based practices.
- Tailored to your environment.
- Five to seven elements.
- Dynamic and evolving.
Slide 4: No Single SSI Prevention Bundle
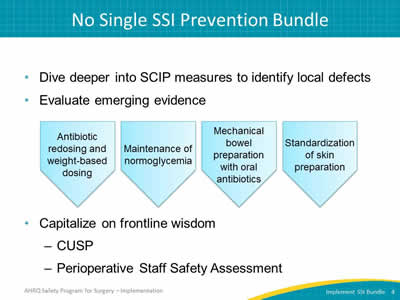
- Dive deeper into SCIP measures to identify local defects.
- Evaluate emerging evidence.
Image: Examples of emerging evidence are presented in five-sided shapes:
- Antibiotic redosing and weight-based dosing.
- Maintenance of normoglycemia.
- Mechanical bowel preparation with oral antibiotics.
- Standardization of skin preparation.
- Capitalize on frontline wisdom:
- CUSP.
- Perioperative Staff Safety Assessment.
Slide 5: Three Ways To Identify Defects
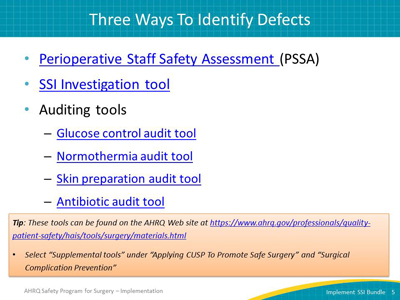
- Perioperative Staff Safety Assessment (PSSA) (Word, 1.57 MB)
- SSI Investigation tool (Word, 1.8 MB)
- Auditing tools:
- Glucose control audit tool (Word, 1.67 MB)
- Normothermia audit tool (Word, 1.59 MB)
- Skin preparation audit tool (Word, 1.57 MB)
- Antibiotic audit tool (Word, 1.6 MB)
Tip: These tools can be found on the AHRQ Web site at https://www.ahrq.gov/professionals/quality-patient-safety/hais/tools/surgery/materials.html.
- Select “Supplemental tools” under “Applying CUSP To Promote Safe Surgery” and “Surgical Complication Prevention.”
Slide 6: AHRQ Safety Program for Surgery—Implementation
Translating Evidence Into Bedside Practice
Slide 7: Translating Evidence Into Practice4
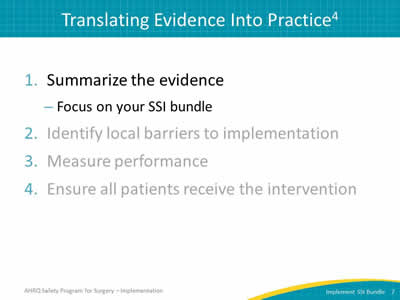
- Summarize the evidence:
- Focus on your SSI bundle.
- Identify local barriers to implementation.
- Measure performance.
- Ensure all patients receive the intervention.
Slide 8: Translating Evidence Into Practice4
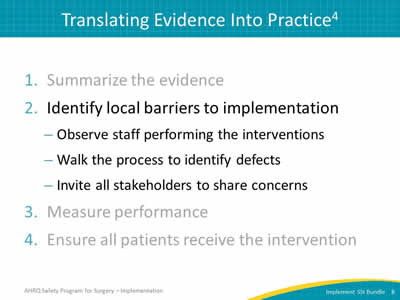
- Summarize the evidence.
- Identify local barriers to implementation:
- Observe staff performing the interventions.
- Walk the process to identify defects.
- Invite all stakeholders to share concerns.
- Measure performance.
- Ensure all patients receive the intervention.
Slide 9: Why Don’t Clinicians Follow the Guidelines?5
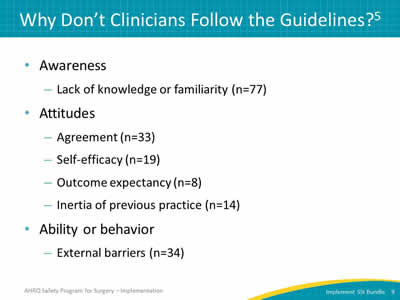
- Awareness
- Lack of knowledge or familiarity (n=77).
- Attitudes
- Agreement (n=33).
- Self-efficacy (n=19).
- Outcome expectancy (n=8).
- Inertia of previous practice (n=14).
- Ability or behavior
- External barriers (n=34).
Slide 10: Barrier Identification & Mitigation
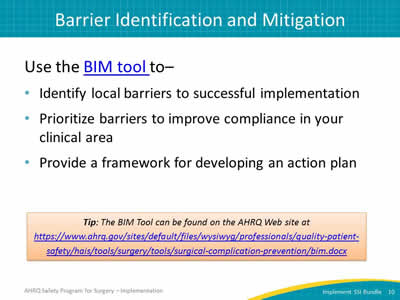
Use the BIM tool to–
- Identify local barriers to successful implementation.
- Prioritize barriers to improve compliance in your clinical area.
- Provide a framework for developing an action plan.
Tip: The BIM tool can be found on the AHRQ Web site at https://www.ahrq.gov/sites/default/files/wysiwyg/professionals/quality-patient-safety/hais/tools/surgery/tools/surgical-complication-prevention/bim.docx (Word, 1.73 MB).
Slide 11: Barrier Identification & Mitigation (BIM)
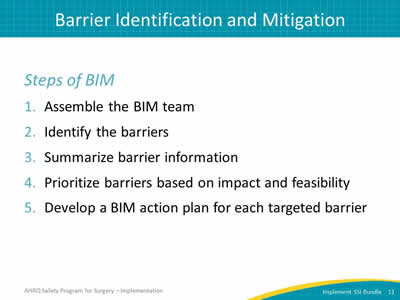
Steps of BIM
- Assemble the BIM team.
- Identify the barriers.
- Summarize barrier information.
- Prioritize barriers based on impact and feasibility.
- Develop a BIM action plan for each targeted barrier.
Slide 12: Assemble Your BIM Team
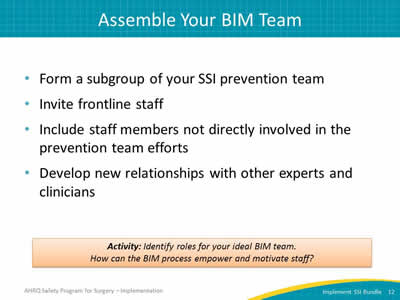
- Form a subgroup of your SSI prevention team.
- Invite frontline staff.
- Include staff members not directly involved in the prevention team efforts.
- Develop new relationships with other experts and clinicians.
Activity: Identify roles for your ideal BIM Team. How can the BIM process empower and motivate staff?
Slide 13: Identify the Barriers
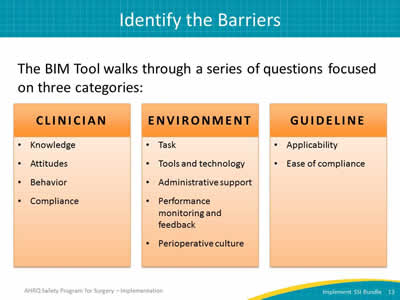
The BIM tool walks through a series of questions focused on three categories.
Image: Each category is listed in a box:
- Clinician
- Knowledge.
- Attitudes.
- Behavior.
- Compliance.
- Environment
- Task.
- Tools and technology.
- Administrative support.
- Performance monitoring and feedback.
- Perioperative culture.
- Guideline
- Applicability.
- Ease of compliance.
Slide 14: Identify the Barriers
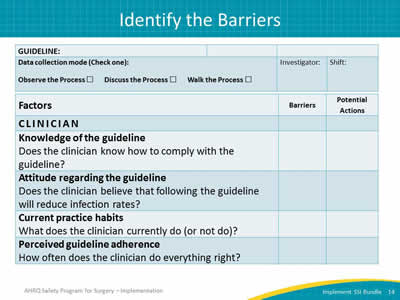
Image: The BIM tool is shown in table format.
First section of the BIM tool. The first column reads: Guideline, Data collection mode (check one):
- Observe the process.
- Discuss the process.
- Walk the process.
The next columns provide space to record the Investigator and the Shift
Second section of the BIM tool. First column reads Factors. Following columns provide space to record Barriers and Potential Actions.
Under the heading Factors is a subheading for Clinician and several categories and questions:
Knowledge of the guideline
Does the clinician know how to comply with the guideline?
Attitude regarding the guideline
Does the clinician believe that following the guideline will reduce infection rates?
Current practice habits
What does the clinician currently do (or not do)?
Perceived guideline adherence
How often does the clinician do everything right?
Slide 15: Identify the Barriers
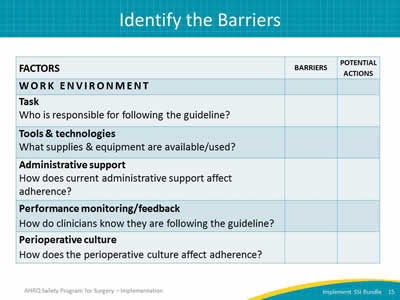
Image: The BIM tool is shown in table format.
Third section of the BIM tool. First column reads Factors. Following columns provide space to record Barriers and Potential Actions.
Under the heading Factors is a subheading for Work Environment and several categories and questions:
Task
Who is responsible for the following guideline?
Tools and technologies
What supplies and equipment are available/used?
Administrative support
How does the current administrative support affect adherence?
Performance monitoring/feedback
How do clinicians know they are following the guideline?
Perioperative culture
How does the perioperative culture affect adherence?
Slide 16: Summarize & Prioritize the Barriers
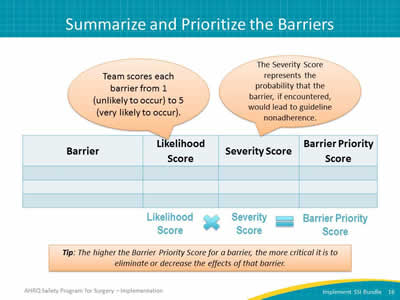
Image: Calculating the barrier priority score for each barrier uses a table with space to record following information: Barrier, Likelihood score, Severity score, and Barrier priority score.
- Likelihood Score: Team scores each barrier from 1 (unlikely to occur) to 5 (very likely to occur).
- The Severity Score represents the probability that the barrier, if encountered, would lead to guideline non-adherence.
- Likelihood Score multiplied by the Severity Score equals the Barrier Priority Score.
Tip: The higher the Barrier Priority Score for a barrier, the more critical it is to eliminate or decrease the effects of that barrier.
Slide 17: Develop a BIM Action Plan

Image: BIM Action Plan table, with space to record: selected actions, performance measures, leader, and followup date.
Slide 18: Translating Evidence Into Practice4
- Summarize the evidence.
- Identify local barriers to implementation.
- Measure performance:
- Select process or outcome measures.
- Audit and SSI investigation tools.
- Ensure all patient receive the intervention.
Slide 19: Measure Performance: Auditing Resources
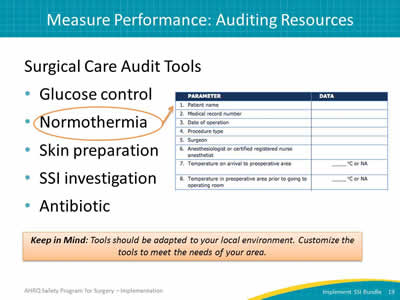
Surgical Care Audit Tools:
- Glucose control.
- Normothermia.
- Skin preparation.
- SSI investigation.
- Antibiotic.
Keep in Mind: Tools should be adapted to your local environment. Customize the tools to meet the needs of your area.
Image: Section of the Normothermia Audit Tool.
Parameter (first column):
- Patient name.
- Medical record number.
- Date of operation.
- Procedure type.
- Surgeon.
- Anesthesiologist or CRNA.
- Pre-op temperature on arrival to pre-op area .
- Temperature in pre-op area prior to going to OR.
Second column allows space to record results.
Slide 20: Practical Applications
“Identifying the contributing defects for patients who develop a surgical site infection is feasible. It unites staff members with a common goal, puts a face to the numbers, and most importantly, is EASY to do.”
—SSI prevention team member
Slide 21: Translating Evidence Into Practice4
- Summarize the evidence.
- Identify local barriers to implementation.
- Measure performance.
- Ensure all patients receive the intervention:
- Engage, educate, execute, and evaluate.
- Educate staff on the science of improving patient safety.
Slide 22: AHRQ Safety Program for Surgery—Implementation
Leading Change With the 4 Es
Slide 23: Implementation: Starting With 4 Es
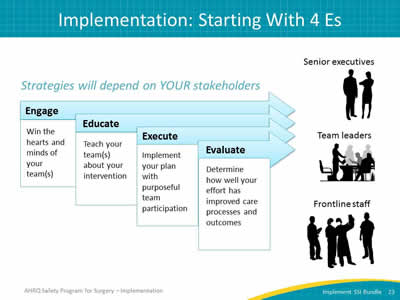
Strategies will depend on YOUR stakeholders.
Engage
Win the hearts and minds of your team(s).
Educate
Teach your team(s) about your intervention.
Execute
Implement your plan with purposeful team participation.
Evaluate
Determine how well your effort has improved care processes and outcomes.
Images: Stacked arrows labeled with Engage, Educate, Execute, and Evaluate:
- Senior executives. Two silhouettes: one male and one female.
- Team leaders. Silhouettes of people in an office setting.
- Frontline staff. Silhouettes of medical professionals.
Slide 24: Key Partnerships
To support the 4 Es, choose partners:
Essential Team Members
- Surgeons.
- Anesthesiologists.
- CRNAs.
- Circulating nurses.
- Scrub nurses.
- Operating room technicians.
- Perioperative nurses.
- Executive partner.
- Nurse leaders.
Supporting Team Members
- Physician assistants.
- Nurse educators.
- Anesthesia assistants.
- Infection preventionists.
- Operating room directors.
- Patient safety officers.
- Chief quality officers.
- Ancillary staff.
Slide 25: Engage
- Post baseline infection rates and number of patients impacted by surgical site infections.
- Share a story about a patient who acquired a surgical site infection.
- Highlight a staff member who ensured patients received evidence-based care.
- Stress that most surgical site infections are preventable.
Slide 26: Fostering Engagement

Intrinsic motivation
Internal, psychological rewards that derive from the work itself.
Extrinsic motivation
External rewards or incentives attached to the work.
Activity: List several examples of both intrinsic and extrinsic motivators.
Image: Arm outstretched and holding a stick with carrots hanging from the stick.
Slide 27: Celebrate Your Heroes
Image: Celebratory bulletin board: Photograph of rows of certificates celebrating good catches and specific team members.
Slide 28: Educate
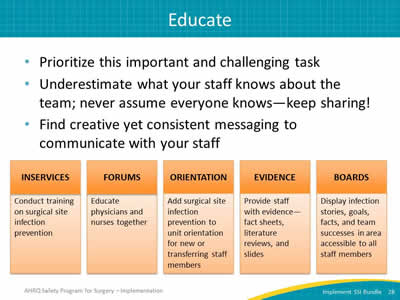
- Prioritize this important and challenging task.
- Underestimate what your staff knows about the team; never assume everyone knows–keep sharing!
- Find creative yet consistent messaging to communicate with your staff.
Image: Education Examples. Five categories of education opportunities listed and described in boxes: inservices, forums, orientation, evidence, and boards.
- Inservices: Conduct training on surgical site infection prevention.
- Forums: Educate physicians and nurses together.
- Orientation: Add surgical site infection prevention to unit orientation for new or transferring staff members.
- Evidence: Provide staff with evidence–fact sheets, literature reviews, and slides.
- Boards: Display infection stories, goals, facts, and team successes in area accessible to all staff members.
Slide 29: Execute: The Principles of Safe Design6
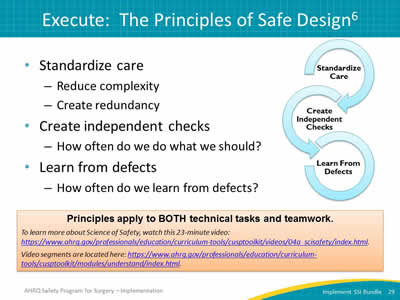
- Standardize care:
- Reduce complexity.
- Create redundancy.
- Create independent checks:
- How often do we do what we should?
- Learn from defects:
- How often do we learn from defects?
Image: Interlocking circles labeled with the three steps of the science of safety:
- Standardize care.
- Create independent checks.
- Learn from defects.
Principles apply to BOTH technical tasks and teamwork. To learn more about Science of Safety, watch this 23-minute video: https://www.ahrq.gov/hai/cusp/videos/04a-science-safety/index.html.
Video segments are located at: https://www.ahrq.gov/hai/cusp/modules/understand/index.html.
Slide 30: Briefings and Debriefings
- Reduce communication breakdowns and OR delays.7
- Reduce procedure and miscommunication-related disruptions and nursing time spent in core.8
- Improve communication and teamwork, as feasible given current workload.9
- Reduce rate of complications, surgical site infection, and mortality.10
Slide 31: Briefings and Debriefings
It is essential to adapt tools to the local environment.
Original briefing process:
- Too long and cumbersome.
- Same form used in all operating room departments, such as–
- Neurosurgery.
- Orthopedics.
- General surgery.
- Did not include followup on comments.
Image: Briefing tool: Original briefing form used in all Hopkins operating room departments.
Slide 32: Real-Time Identification of Defects11
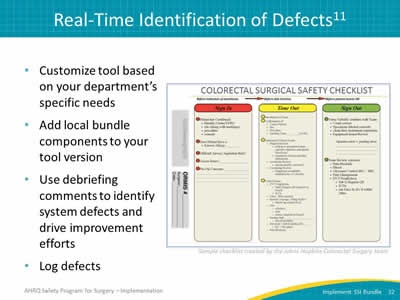
- Customize tool based on your department’s specific needs.
- Add local bundle components to your tool version.
- Use debriefing comments to identify system defects and drive improvement efforts.
- Log defects.
Image: Revised briefing tool customized for the colorectal department based on the chosen bundled interventions.
Slide 33: Debriefing Defect Logbook
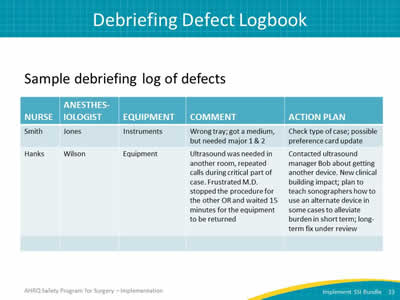
Sample debriefing log of defects.
Image: Table shows two examples shared with the following column headings: Nurse, Anesthesiologist, Equipment, Comment, and Action Plan.
First example of an instrument defect: Wrong tray; got a medium, but needed major 1 & 2. Action: Check type of case; possible preference card update
Second example of an equipment defect: Ultrasound was needed in another room, repeated calls during critical part of case. Frustrated MD stopped the procedure for the other OR and waited 15 minutes for the equipment to be returned. Action: Contacted ultrasound manager Bob about getting another device. New clinical building impact; Plan to teach sonographers how to use an alternate device in some cases to alleviate burden in short-term; long-term fix under review,
Slide 34: Example of Defects Addressed: Instruments
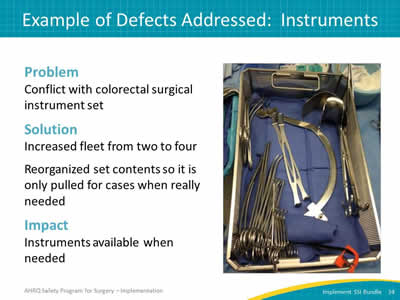
Problem
Conflict with colorectal surgical instrument set.
Solution
Increased fleet from two to four.
Reorganized set contents so it is only pulled for cases when really needed.
Impact
Instruments available when needed.
Image: Photo of colorectal surgery set of tools.
Slide 35: Evaluate
- An equally important and challenging task.
- Essential to report progress to your team:
- Track your surgical site infection rates and detect trends.
- Post your progress in the unit and discuss during staff meetings.
- Acknowledge and celebrate your successes.
Slide 36: Key Points
- Briefings and debriefings provide a proven effective strategy to standardize care and create independent checks.
- Moving staff from compliant to engaged is key to a successful intervention.
- Briefing and debriefing tools must be customized to address your local defects and goals.
- Close the loop to solve defects at the system level.
Slide 37: This Model Works in the OR
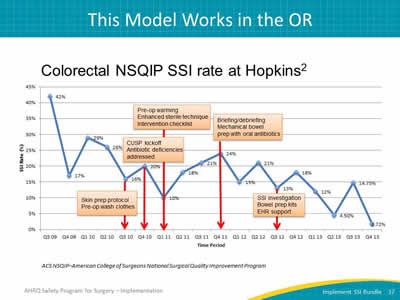
Colorectal NSQIP SSI rate at Hopkins2
Image: Chart shows significant drop in SSI rate at Johns Hopkins Hospital as reported through NSQIP from third quarter 2009 through the fourth quarter of 2013. Developed at Johns Hopkins Armstrong Institute for Patient Safety and Quality.
ACS NSQIP–American College of Surgeons National Surgical Quality Improvement Program
Slide 38: Summary
- No single SSI prevention bundle exists.
- Identify and address local defects.
- Briefings and debriefings standardize care, reduce complexity and create redundancy.
- Use 4 Es model to guide change.
Image: Stacked arrows labeled Engage, Educate, Execute, and Evaluate.
Slide 39: Recap of Learning Objectives
- Develop an implementation plan for your SSI prevention bundle.
- Identify and address local barriers to implementing your SSI prevention bundle.
- Use the BIM Tool.
Slide 40: References
- Crolla RM, van der Laan L, Veen EJ, et al. Reduction of surgical site infections after implementation of a bundle of care. PLoS One 2012; 7:e44599. PMID: 22962619.
- Wick EC, Hobson DB, Bennett JL, et al. Implementation of a surgical comprehensive unit-based safety program to reduce surgical site infections. J Am Coll Surg 2011; 215:193-200. PMID: 22632912.
- Hedrick TL, Heckman JA, Smith RL, et al. Efficacy of protocol implementation on incidence of wound infection in colorectal operations. J Am Coll Surg 2007; 205:432-8. PMID: 17765159.
- Pronovost PJ, Berenholtz SM, Needham DM. Translating evidence into practice: a model for large-scale knowledge translation. BMJ 2008; 337:963-5. PMID: 18838424.
- Cabana MD, Rand CS, Powe NR, et al. Why don’t physicians follow clinical practice guidelines? A framework for improvement. JAMA 1999 Oct 20;282(15):1458-65. PMID: 10535437.
Slide 41: References
- Pronovost PJ, Goeschel CA, Marsteller JA, et al. Framework for patient safety research and improvement. Circulation 2009; 119:330-7. PMID: 19153284.
- Nundy S, Mukherjee A, Sexton JB, et al. Impact of preoperative briefings on operating room delays: a preliminary report. Arch Surg 2008; 143(11): 1068-72. PMID: 19015465.
- Henrickson SE, Wadhera RK, Elbardissi AW, et al. Development and pilot evaluation of a preoperative briefing protocol for cardiovascular surgery. J Am Coll Surg 2009; 208:1115-23. PMID: 19476900.
- Berenholtz SM, et al. Implementing standardized operating room briefings and debriefings at a large regional medical center. Jt Comm J Qual Saf 2009; 35(8):391-7. PMID: 19719074.
- Haynes AB. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med 2009; 360:491-9. PMID: 19144931.
- Bandari J. Surfacing safety hazards using standardized operating room briefings and debriefings at a large regional medical center. Jt Comm J Qual Saf 2012; 38(4):154-60. PMID: 22533127.



