Program Overview: Slide Presentation
AHRQ Safety Program for Surgery
Slide 1: AHRQ Safety Program for Surgery—Onboarding
Program Overview
Slide 2: Mead Quotation
"Never doubt that a small group of thoughtful, committed citizens can change the world; indeed, it is the only thing that ever has."
—Margaret Mead
Slide 3: Learning Objectives
After this session, you will be able to–
- Distinguish this safety program from that of other national improvement projects.
- Describe the connection between surgical safety teamwork and safety culture work as structured in the Comprehensive Unit-based Safety Program (CUSP).
- List the steps for developing a local surgical site infection (SSI) prevention bundle.
Slide 4: Why Is This Work Important?1
- 1 in 25 people will undergo surgery.
- 7 million complications follow inpatient surgeries:
- Complications impact 25% of inpatient surgeries.
- 1 million deaths follow surgery:
- Between 0.5 and 5% of surgical patients do not survive.
- Surgery is linked to 50% of all hospital adverse events.
- Most hospital adverse events are AVOIDABLE.
Slide 5: Surgical Care Improvement Project (SCIP)2
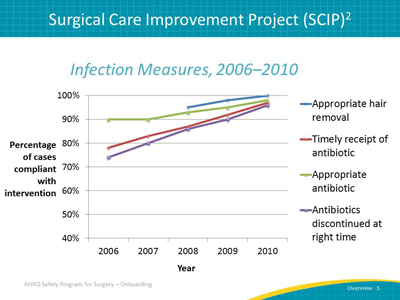
Image: Infection Measures, 2006-2010. CMS Surgical Care Improvement Project Infection Measures. Line graph showing how the compliance with the CMS Surgical Care Improvement Project (SCIP) measures have improved between 2006 and 2010.
Measures included are listed:
- Appropriate hair removal.
- Timely receipt of antibiotic.
- Appropriate antibiotic.
- Antibiotics discontinued at right time.
Courtesy of CMS National Impact Assessment of Medicare Quality Measures. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/QualityMeasures/Downloads/NationalImpactAssessmentofQualityMeasuresFINAL.PDF. March 2012; 42.
Slide 6: What is the AHRQ Safety Program for Surgery?
- National improvement effort for hospitals of all sizes and any surgical procedure type.
- Designed to reduce SSIs and other surgical complications for any procedure type.
Slide 7: What is the AHRQ Safety Program for Surgery?
- Program will teach you to embed adaptive work (CUSP) in your technical work (surgical care).
- Unlike other SSI prevention projects, you will develop your own SSI prevention “bundle”:
- There is no one “right” bundle for SSI prevention.
- Tap the wisdom of your frontline staff to identify local defects.
Slide 8: Safety Program Leverages National Leaders

Images: Logos for partner organizations:
- Agency for Healthcare Research and Quality.
- Johns Hopkins Medicine.
- Armstrong Institute for Patient Safety and Quality.
- American College of Surgeons National Surgical Quality Improvement Program.
- World Health Organization.
- University of Pennsylvania.
Slide 9: Shared Program Goals
- To achieve significant reductions in surgical site infection and surgical complication rates.
- To achieve significant improvements in safety culture.
Slide 10: Key Concepts: Technical and Adaptive Work
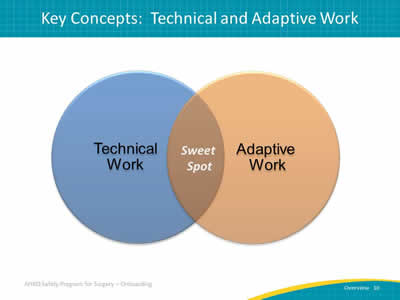
Image: Overlapping circles form a Venn Diagram. One circle is labeled "Technical Work" and another circle labeled "Adaptive Work." In the center where the two circles overlap, is the "Sweet Spot."
Image Source: Armstrong Institute for Patient Safety and Quality
Slide 11: Key Concepts: Technical and Adaptive Work
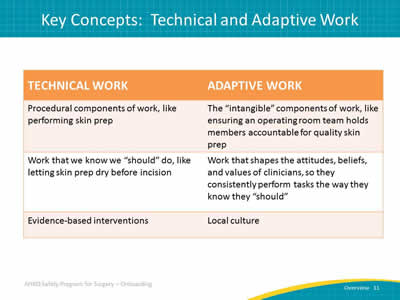
Image: Table defining and comparing technical and adaptive work.
Technical work
- Procedural components of work, like performing skin prep.
- Work that we know we ‘should’ do, like letting skin prep dry before incision.
- Work that lends itself to checklists or protocols.
Adaptive work
- The ‘intangible’ components of work, like ensuring an operating room team holds each other accountable for quality skin prep.
- Work that shapes the attitudes, beliefs, and values of clinicians, so they consistently perform tasks the way they know they “should.”
- Culture change is not a checklist.
Image Source: Armstrong Institute for Patient Safety and Quality.
Slide 12: Comprehensive Unit-based Safety Program (CUSP)
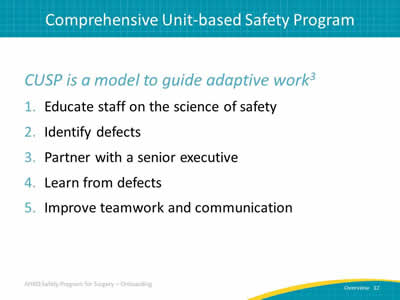
CUSP is a model to guide adaptive work3
- Educate staff on the science of safety.
- Identify defects.
- Partner with a senior executive.
- Learn from defects.
- Implement teamwork tools and communication.
Slide 13: How is Safety Program for Surgery Different?
- Informed by science and backed with evidence.
- Led by clinicians and supported by management.
- Guided by national and local measures.
- National implementation tailored to local context.
Slide 14: Building on Previous State Level Success
Michigan Keystone ICU program
- Reductions in central line-associated blood stream infections (CLABSI).3,4
- Reductions in ventilator-associated pneumonias (VAP).5
- Improvements in safety climate in intensive care units (ICUs).6
Slide 15: ... And National-Level Highlights
National On the CUSP: Stop BSI program7
- A national initiative to implement a proven culture change model, CUSP, and interventions to prevent CLABSI.
- A total of 1,071 ICU’s in 45 States.
- A 43% reduction in CLABSI rates.
- The number of ICU’s that achieved CLABSI rate of zero, more than doubled.
Slide 16: Positive Impact of CUSP on Michigan ICU Safety Culture
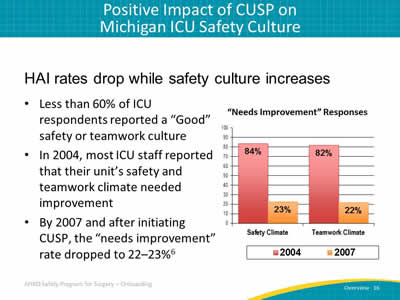
HAI rates drop while safety culture increases.
- Less than 60% of ICU respondents reported a “Good” safety or teamwork culture.
- In 2004, most ICU staff reported that their unit’s safety and teamwork climate needed improvement.
- By 2007 and after initiating CUSP, the “needs improvement” rate dropped to 22-23%.
Image: Bar graph shows positive impact of CUSP in Michigan ICUs. Percent responses to the question of whether the safety climate or teamwork climate needs improvement for the years 2004 and 2007 are shown. Statewide in 2004, 84% of respondents indicated that the safety climate needed improvement while 82% indicated that the teamwork climate needed improvement. In 2007, 23% of respondents indicated that the safety climate needed improvement while 22% indicated that teamwork needed improvement.
References: Sexton JB, Berenholtz SM, Goeschel CA, et al. Assessing and improving safety climate in a large cohort of intensive care units. Crit Care Medicine 2011 May;39(5):934-9. PMID: 21297460.
Slide 17: The Improvement Model Works in Surgery
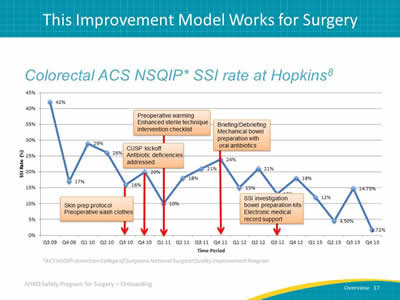
Colorectal NSQIP SSI Rate at Hopkins8
Image: Line chart shows gradual decrease in colorectal SSI rate from 42% to 12 % over 4 years.
- Quarter 3/2010: implementation of skin preparation protocol; preoperative wash clothes.
- Quarter 4/2010: Implementation of CUSP kick off; antibiotic deficiencies addressed.
- Quarter 1/2011: Implementation of preoperative warming; enhanced sterile technique; intervention checklist.
- Quarter 4/2011: Implementation of briefing and debriefing mechanical bowel preparation with oral antibiotics.
- Quarter 3/2012: Implementation of SSI investigation tool; bowel prep kits; Electronic medical report support.
Slide 18: Case Study: Laparoscopic Gastrointestinal Surgery Trays
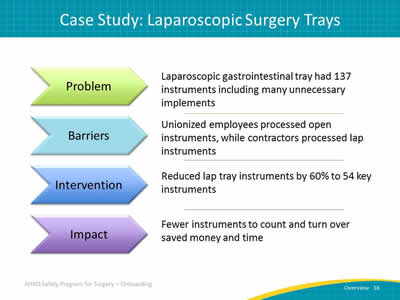
Image: Table with headings featured in arrows:
Problem
Laparoscopic gastrointestinal tray had 137 instruments including many unnecessary implements.
Barriers
Unionized employees process open instruments, while contractors process lap instruments.
Intervention
Reduced lap tray instruments by 60% to 54 key instruments.
Impact
Fewer instruments to count and turnover saves money and time.
Image Source: Armstrong Institute for Patient Safety and Quality.
Slide 19: Case Study: Antibiotic Irrigation
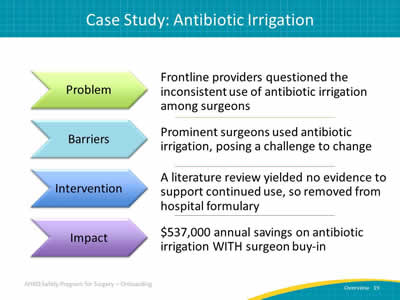
Image: Table with headings featured in arrows:
Problem
Frontline providers questioned the inconsistent use of antibiotic irrigation between surgeons.
Barriers
Prominent surgeons used antibiotic irrigation.
Intervention
A literature review yielded no evidence to support continued use, so removed from hospital formulary.
Impact
$537,000 annual savings on antibiotic irrigation WITH surgeon buy-in.
Image Source: Armstrong Institute for Patient Safety and Quality.
Slide 20: References
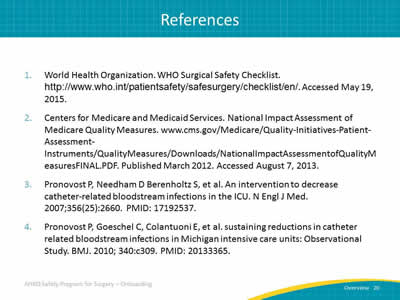
- World Health Organization. WHO Surgical Safety Checklist. http://www.who.int/patientsafety/safesurgery/checklist/en/. Accessed May 19, 2015.
- Centers for Medicare and Medicaid Services. National Impact Assessment of Medicare Quality Measures. www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/QualityMeasures/Downloads/NationalImpactAssessmentofQualityMeasuresFINAL.PDF. Published March 2012. Accessed August 7, 2013.
- Pronovost P, Needham D Berenholtz S, et al. An intervention to decrease catheter-related bloodstream infections in the ICU. N Engl J Med 2007;356(25):2660. PMID: 17192537.
- Pronovost P, Goeschel C, Colantuoni E, et al. sustaining reductions in catheter related bloodstream infections in Michigan intensive care units: Observational Study. BMJ 2010; 340:c309. PMID: 20133365.
Slide 21: References
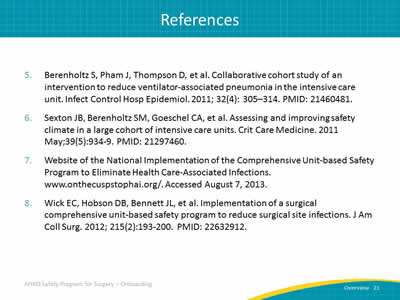
- Berenholtz S, Pham J, Thompson D, et al. Collaborative cohort study of an intervention to reduce ventilator-associated pneumonia in the intensive care unit. Infect Control Hosp Epidemiol 2011; 32(4): 305–314. PMID: 21460481.
- Sexton JB, Berenholtz SM, Goeschel CA, et al. Assessing and improving safety climate in a large cohort of intensive care units. Crit Care Medicine 2011 May;39(5):934-9. PMID: 21297460.
- Web site of the National Implementation of the Comprehensive Unit-based Safety Program to Eliminate Health Care-Associated Infections. www.onthecuspstophai.org/. Accessed August 7, 2013.
- Wick EC, Hobson DB, Bennett JL, et al. Implementation of a surgical comprehensive unit-based safety program to reduce surgical site infections. J Am Coll Surg 2012; 215(2):193-200. PMID: 22632912.
Slide 22: AHRQ Safety Program for Surgery
Building your Surgical Safety Program Team
Who is in the room with you?
Slide 23: Learning Objectives
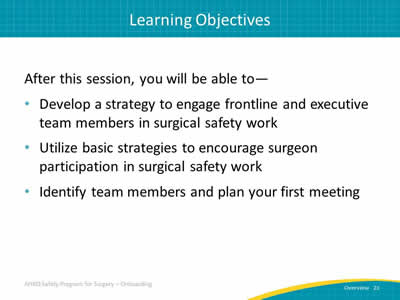
After this session, you will be able to–
- Develop a strategy to engage frontline and executive team members in surgical safety work.
- Utilize basic strategies to encourage surgeon participation in surgical safety work.
- Identify team members and plan your first meeting.
Slide 24: Perioperative Safety Team Members
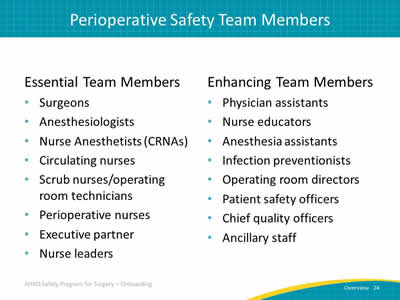
Essential Team Members
- Surgeons.
- Anesthesiologists.
- Nurse anesthesiologists (CRNAs).
- Circulating nurses.
- Scrub nurses/Operating room technicians.
- Perioperative nurses.
- Executive partner.
- Nurse leaders.
Enhancing Team Members
- Physician assistants.
- Nurse educators.
- Anesthesia assistants.
- Infection preventionists.
- Operating room directors.
- Patient safety officers.
- Chief quality officers.
- Ancillary staff.
Slide 25: Your Surgical Safety Team
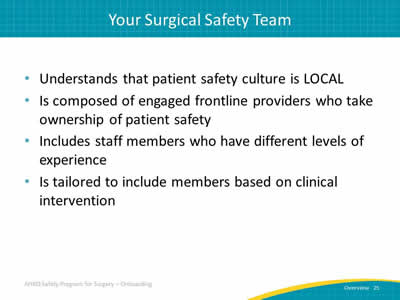
- Understands that patient safety culture is LOCAL.
- Composed of engaged frontline providers who take ownership of patient safety.
- Includes staff members who have different levels of experience.
- Tailored to include members based on clinical intervention.
Slide 26: Surgical Safety Team Logistics
- Meets regularly:
- Weekly ideal.
- Monthly at a minimum.
- Has adequate resources including protected time:
- 2 to 4 hours per week for a team leader, surgeon, anesthesia, nurse, and infection preventionist.
Slide 27: Surgical Safety Team Group Processes

Image: Information is presented in a flower arrangement of circles. Effective Group Processes makes up center circle, surrounded by ‘petals’ labeled with each category. The effective group processes of surgical safety teams include:
- Role clarity.
- Effective team communication.
- Conflict resolution.
- Education and engagement.
- Senior leadership buy-in support.
- Norms.
Slide 28: Role of Senior Executive Partner
- Helps the team prioritize improvement efforts.
- Helps the team navigate organizational bureaucracy.
- Ensures the safety team has necessary resources to fix problems.
- “Comes out of the office” to meet monthly with members of health care team in their clinical area.
Slide 29: Finding a Senior Executive Partner
- Contact hospital management to determine which senior executive will best fit the perioperative area and the following criteria:
- Director level or above.
- Available to attend rounds for at least 1 hour per month.
- Approachable about and comfortable with sensitive topics.
- Set up a meeting to introduce the project, provide a tour of the perioperative area, and share unit-level information.
Slide 30: Role of Surgeon Leader
- Serves as role model for surgical safety activities.
- Meets with safety team at least monthly.
- Participates in monthly senior executive partnership meetings.
- Communicates with physician group as needed.
- Assists with implementation of interventions.
Slide 31: Engaging Surgeons on the Surgical Safety Team

Image: Information presented in orange squares for visual interest. When engaging surgeons on a surgical safety team, it is important to:
- Identify surgeon leaders.
- Explain the role.
- Listen to surgeon concerns.
- Develop plans to address concerns.
- Reward surgeon leaders.
- Develop a vehicle for communication.
- Formalize communication plan.
Image Source: Armstrong Institute for Patient Safety and Quality.
Slide 32: Practical Tips for Scheduling Meetings
- Incorporate surgical safety team meetings into ongoing educational activities to ease scheduling challenges:
- Regularly scheduled nurse training.
- Grand rounds for physicians.
- Grand rounds that include nurses.
- Offer incentives for participating.
Slide 33: Surgical Roles and Responsibilities Tool
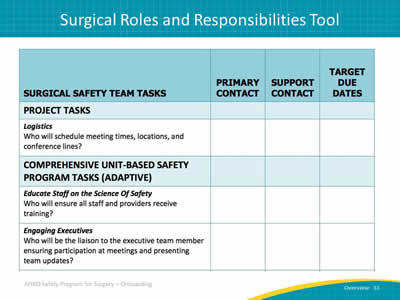
Image: Sample Team Roles and Responsibilities tool that lists project tasks (such as project calls, logistics, etc.) and columns for Primary contact, Supporting roles, and Target due dates. Tool features a list of tasks with three categories: project tasks, CUSP tasks, and SSI prevention tasks.
Also includes two adaptive CUSP tasks.
Educate Staff on the Science of Safety: Who will ensure all staff and providers receive training?
Engaging Executives: Who will be liaison to the executive team member ensuring participation at meetings and presenting team updates?
Slide 34: Surgical Roles and Responsibilities Tool
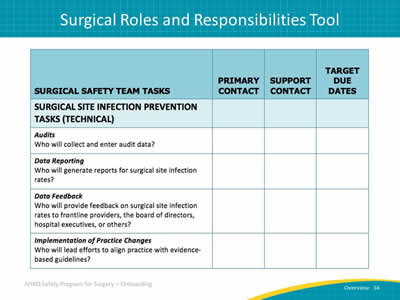
Image: Sample Team Roles and Responsibilities tool that lists project tasks (such as project calls, logistics, etc.) and columns for Primary contact, Supporting roles, and Target due dates. Tool features a list of tasks with three categories: project tasks, CUSP tasks, and SSI prevention tasks.
Technical examples shown here.
Audits: Who will collect and enter audit data?
Data Reporting: Who will generate reports for surgical site infection rates?
Data Feedback: Who will provide feedback on surgical site infection rates to frontline providers, the board of directors, hospital executives, or others?
Implementation of Practice Changes: Who will lead efforts to align practice with evidence-based guidelines?
Slide 35: Next Steps
- Recruit a team lead, nurse lead, surgeon lead, and executive partner along with other team members.
- List team member names and contact information and post in a central location.
- Schedule your meetings for 6 to 12 months.
- Complete the Surgical Safety Team Roles and Responsibilities tool during your first meeting.
Slide 36: AHRQ Safety Program for Surgery

An Introduction To Building And Measuring Safety Culture
The “adaptive” glue that helps bond safe teams.
Slide 37: Learning Objectives
After this session, you will be able to–
- Define safety culture.
- Describe why a safety culture is important for improvement efforts.
- Explain the safety culture measurement process.
Slide 38: What is Safety Culture?
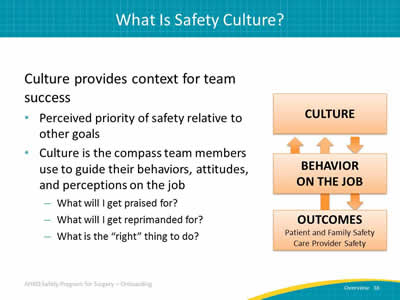
Culture provides the context for team success.
- Perceived priority of safety relative to other goals.
- Culture is the compass team members use to guide their behaviors, attitudes, and perceptions on the job:
- What will I get praised for?
- What will I get reprimanded for?
- What is the “right” thing to do?
Image: Top box (1) is labeled "Culture." Middle box (2) is labeled "Behavior on the Job" and Lower box (3) is labeled "Outcomes." The "Outcomes" box includes two examples: patient and family safety and provider safety. Arrows connect all boxes to show cycle between culture, behavior on the job and outcome. Culture drives behavior on the job, which contributes to safety outcomes. Those outcomes in turn contribute to behavior on the job and the culture.
Slide 39: Core Aspects of a Safety Culture1

Image: The core aspects of safety culture. This image is of a converging radial that outlines six domains of safety culture. The central red circle is labeled "Culture of Safety". Surrounding this red circle are six boxes with arrows pointing to the circle.
These boxes are labeled:
- Communication patterns and language.
- Feedback, reward, and corrective action practices.
- Formal and informal leader actions and expectations.
- Teamwork processes (e.g., back-up behavior).
- Resource allocation practices.
- Error-detection and corrective system.
Based on definitions of culture proposed by Dr. Edgar Schein, MIT Sloan School of Management.
Image Source: Armstrong Institute for Patient Safety and Quality.
Slide 40: Why Safety Culture Matters
Safety Culture is Related to Outcomes2-8
- Patient outcomes:
- Patient care experience.
- Infection rates, sepsis.
- Postoperative hemorrhage, respiratory failure, accidental puncture/laceration.
- Treatment errors.
- Clinician outcomes:
- Incident reporting.
- Burnout/turnover.
Slide 41: Why Safety Culture Matters9-12
- Safety culture influences the effectiveness of other safety and quality interventions:
- Can enhance or inhibit effects of other interventions.
- Safety culture can change through intervention:
- Best evidence for culture interventions that use multiple components.
Slide 42: CUSP and Safety Culture
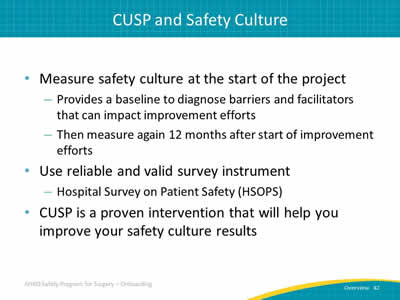
- Measure safety culture at the start of the project:
- Provides a baseline to diagnose barriers and facilitators that can impact improvement efforts.
- Then will be measured again 12 months following start of improvement efforts.
- Use reliable and valid survey instrument:
- Hospital Survey on Patient Safety (HSOPS).
- CUSP is a proven intervention that will help you improve your culture results.
Slide 43: Example: HSOPS Questions & Composite Scores
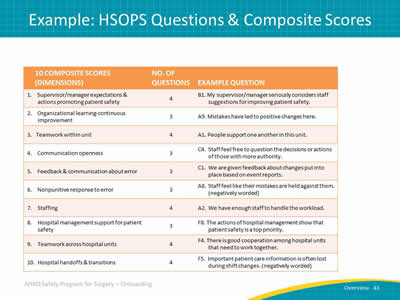
Image: Table listing HSOPS dimensions and example questions. Table shows HSOPS questions and composite scores. Column 1 shows 10 composite scores or "dimensions". Column 2 shows the number of questions for each dimension and column 3 shows example questions.
Slide 44: Example: HSOPS Questions & Composite Scores
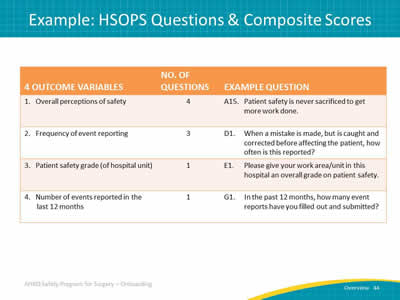
Image: Table listing HSOPS outcome variables and example questions. Table has three columns. Column 1 shows the four outcome variables in an HSOPS. Column 2 shows the number of questions associated with each variable and column 3 shows an example question to probe each outcome variable.
Slide 45: Have Existing HSOPS Data?
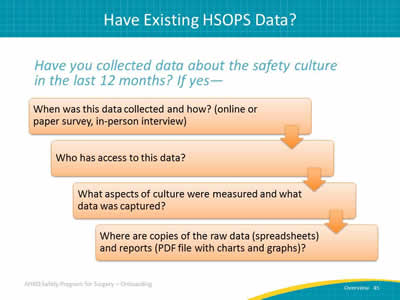
Have you collected data about the safety culture in your work in the last 12 months? If yes—
Image: Questions are presented in orange boxes for visual interest; arrows show progression through the questions/boxes:
- When was this data collected and how (online survey, paper survey, in person interviews)?
- Who has access to this data?
- What aspects of culture were measured and what data was captured?
- Where are copies of the raw data (e.g., spreadsheets) and reports (PDF file with charts and graphs)?
Slide 46: References
- Schein E. Organizational culture and leadership, 4th edition. San Francisco, CA: Jossey-Bass. 2010.
- Huang DT, Clermont G, Kong L, Weissfeld LA, Sexton JB, Rowan KM, Angus DC. Intensive care unit safety culture and outcomes: a US multicenter study. Int J Qual Health Care 2010 Jun;22(3):151-61.
- MacDavitt K, Chou SS, Stone PW. Organizational climate and health care outcomes. Jt Comm J Qual Patient Saf 2007 Nov;33(11 Suppl):45-56.
- Mardon RE, Khanna K, Sorra J, Dyer N, Famolaro T. Exploring relationships between hospital patient safety culture and adverse events. J Patient Saf 2010 Dec;6(4):226-32.
- Singer SJ, Falwell A, Gaba DM, Meterko M, Rosen A, Hartmann CW, Baker L. Identifying organizational cultures that promote patient safety. Health Care Manage Rev 2009 Oct-Dec;34(4):300-11.
Slide 47: References
- Sorra J, Khanna K, Dyer N, Mardon R, Famolaro T. Exploring Relationships Between Patient Safety Culture and Patients' Assessments of Hospital Care. J Patient Saf 2012 Jul 10. [Epub ahead of print].
- Sorra JS, Nieva VF. Hospital Survey on Patient Safety Culture. (Prepared by Westat, under Contract No. 290-96-0004). AHRQ Publication No. 04-0041. Rockville, MD: Agency for Healthcare Research and Quality. September 2004.
- Weaver SJ. A configural approach to patient safety climate: The relationship between climate profile characteristics and patient safety. Doctoral dissertation. University of Central Florida. 2011.
- Haynes AB, Weiser TG, Berry WR, Lipsitz SR, Breizat AH, Dellinger EP, Dziekan G, Herbosa T, Kibatala PL, Lapitan MC, Merry AF, Reznick RK, Taylor B, Vats A, Gawande AA; Safe Surgery Saves Lives Study Group. Changes in safety attitude and relationship to decreased postoperative morbidity and mortality following implementation of a checklist-based surgical safety intervention. BMJ Qual Saf 2011 Jan;20(1):102-7.
- Morello RT, Lowthian JA, Barker AL, McGinnes R, Dunt D, Brand C. Strategies for improving patient safety culture in hospitals: a systematic review. BMJ Qual Saf 2012 Jul 31. [Epub ahead of print]
Slide 48: References
- Van Noord I, de Bruijne MC, Twisk JW. The relationship between patient safety culture and the implementation of organizational patient safety defences at emergency departments. Int J Qual Health Care 2010 Jun;22(3):162-9.
- Weaver, S. J., Dy, S., Lubomski, L., & Wilson, R. Promoting a culture of safety. In R.M. Watcher, P.G. Shekelle, P. Pronovost (Eds.). Making healthcare safer: A critical analysis of the evidence of patient safety practices (AHRQ report # TBD). Rockville, MD. In press.
Slide 49: AHRQ Safety Program for Surgery
Next Steps
We’re in this together.
Slide 50: Preparing to Lead
- In a postmortem, an autopsy is performed to learn why a patient died. While it may be helpful to those interested in the results, it does not help the central figure in the medical drama—the patient.
- The PreMortem Exercise is used to identify potential barriers and vulnerabilities to project success before they occur. It builds intuition and sensitivity to future problems.
Slide 51: Premortem Exercise
Step 1
- Imagine that we are 2 years into the future. Despite all of the team’s efforts, the project has failed—catastrophically. Things have gone completely wrong on a number of fronts.
- Now, ask:
- What does the worst-case scenario look like?
Slide 52: Premortem Exercise
Step 2
- Generate the reasons for failure.
- Spend 10 minutes recording the reasons you believe this failure occurred.
- Now, ask:
- What could have caused our project to fail?
Slide 53: Premortem Exercise
Step 3
- Prioritize your list of potential reasons for failure.
- Address the top two or three concerns.
- Now, ask:
- What specific actions can you take to avoid or manage these concerns?
Slide 54: Premortem Exercise
Step 4
- Throughout your project, periodically review the potential problem list with your team.
- This process will raise team awareness to problems that may be emerging and allow them to anticipate solutions.
Slide 55: Premortem Summary
- Two years out, what does the worst-case scenario look like?
- What could have caused your project to fail?
- What specific actions can you take to avoid or manage these issues?
- Review and anticipate potential problems throughout the project.



