- Thirty years ago, the Heckler Report found that:
- Cardiovascular disease (CVD) is a major cause of death in Hispanics, although the rate is lower than in Whites. To date, national epidemiologic data on CVD mortality in Hispanics are limited.
- There appears to be a strong inverse relationship between socioeconomic status (SES) and hypertension in Hispanics, similar to that found for Blacks and Whites.
- Diabetes mellitus is a major problem in Hispanics, especially in Mexican Americans and Puerto Ricans living in the United States.
- The generally higher prevalence of obesity, noninsulin-dependent diabetes, hypertension, high LDL cholesterol and low HDL cholesterol levels in Hispanics might be expected to increase their CVD risk. Those Mexican Americans with lowest SES and level of acculturation have significantly worse CVD risk factor profiles than those in higher SES groups.
Cardiovascular Care for Hispanics
| Measure | Most Recent Disparity | Disparity Change |
|---|---|---|
| Adults who received a blood pressure measurement in the last 2 years and can state whether their blood pressure was normal or high | Worse | No Change |
| Adult admissions for hypertension | Worse | No Change |
| Adult admissions for angina without cardiac procedure | Worse | No Change |
| Adult admissions for congestive heart failure | Same | Narrowing |
| Hospital patients with heart failure and left ventricular systolic dysfunction who were prescribed angiotensin-converting enzyme inhibitor or angiotensin receptor blocker at discharge | Better | No Change |
| Hospital patients with heart attack given percutaneous coronary intervention within 90 minutes of arrival | Worse | No Change |
| Hospital patients with heart attack given fibrinolytic medication within 30 minutes of arrival | Same | No Change |
- Trends: Most measures of cardiovascular care for Hispanics were improving.
- Groups With Disparities:
- Hispanics were less likely than Whites to have their blood pressure checked and to receive timely percutaneous coronary intervention when hospitalized with a heart attack. These disparities did not change over time.
- Hispanics had higher rates of admission than Whites for hypertension and for angina and these disparities did not change over time.
- Hispanics and Whites had similar rates of admission for congestive heart failure. This represents the elimination of a previously observed disparity.
- Hispanics and Whites had similar rates of receipt of fibrinolytic medication for heart attack.
- Hispanics hospitalized with heart failure were more likely to be prescribed angiotensin-converting enzyme inhibitor or angiotensin receptor blocker at discharge and this disparity did not change over time.
Blood Pressure Measurement
Adults who received a blood pressure measurement in the last 2 years and can state whether their blood pressure was normal or high, by race/ethnicity and by age among Hispanics, 1998-2012
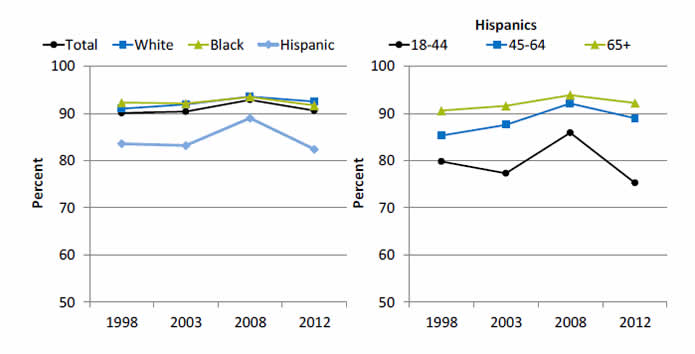
Left Graph:
| Race/Ethnicity | 1998 | 2003 | 2008 | 2012 |
|---|---|---|---|---|
| Total | 90.1 | 90.4 | 92.9 | 90.6 |
| White | 91.0 | 91.9 | 93.6 | 92.5 |
| Black | 92.3 | 92.1 | 93.5 | 91.7 |
| Hispanic | 83.6 | 83.2 | 89.0 | 82.4 |
Right Graph (Hispanics):
| Age | 1998 | 2003 | 2008 | 2012 |
|---|---|---|---|---|
| 18-44 | 79.8 | 77.3 | 85.9 | 75.3 |
| 45-64 | 85.3 | 87.6 | 92.1 | 89.0 |
| 65+ | 90.6 | 91.6 | 93.9 | 92.2 |
Source: Centers for Disease Control and Prevention, National Center for Health Statistics, National Health Interview Survey, 1998-2012.
Denominator Adult civilian noninstitutionalized population.
Note: Measure is age adjusted.
- Importance: Early detection and treatment of high blood pressure can prevent heart failure, kidney failure, and stroke. Because high blood pressure typically causes no symptoms, screening is essential.
- Trends: From 1998 to 2012, the percentage of adults who received a blood pressure measurement in the last 2 years and can state whether their blood pressure was normal or high did not change overall or for any ethnic group.
- Groups With Disparities:
- In all years, Hispanic adults were less likely to receive a blood pressure measurement compared with Whites.
- In all years, Hispanics ages 18-44 were less likely to receive a blood pressure measurement compared with Hispanics age 65 and over.
Admissions for Congestive Heart Failure
Adult admissions for congestive heart failure per 100,000 population, by race/ethnicity, 2002-2012
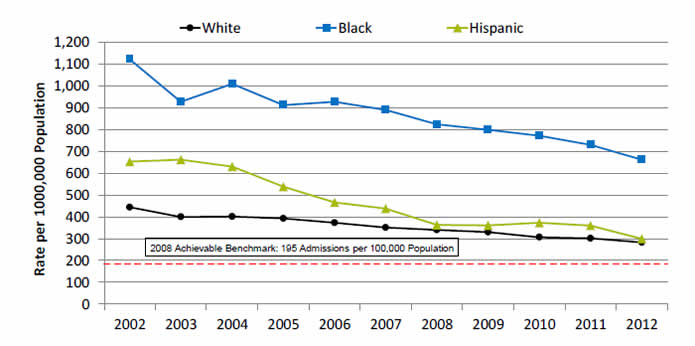
| Year | White | Black | Hispanic |
|---|---|---|---|
| 2002 | 444.1 | 1121.8 | 653.0 |
| 2003 | 399.5 | 927.8 | 662.2 |
| 2004 | 400.9 | 1009.3 | 629.9 |
| 2005 | 392.8 | 912.4 | 538.0 |
| 2006 | 373.0 | 927.5 | 465.9 |
| 2007 | 350.8 | 890.2 | 437.1 |
| 2008 | 339.9 | 824.6 | 362.8 |
| 2009 | 329.7 | 799.2 | 360.2 |
| 2010 | 306.3 | 771.4 | 372.7 |
| 2011 | 301.1 | 730.5 | 359.2 |
| 2012 | 283.2 | 662.2 | 298.9 |
2008 Achievable Benchmark: 195 Admissions per 100,000 Population.
Source: Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project, State Inpatient Databases, 2002‐2012 disparities analysis files and AHRQ Quality Indicators, modified version 4.4.
Denominator U.S. resident population age 18 and over.
Note: For this measure, lower rates are better. White and Black are non-Hispanic. Hispanic includes all races.
- Importance: Racial disparities in care for congestive heart failure have been observed.
- Trends: From 2002 to 2012, the rate of admission for congestive heart failure among adults decreased significantly for all ethnic groups.
- Groups With Disparities:
- In all years, compared with White patients, rates of admission for congestive heart failure were higher among Black patients.
- From 2002 to 2007, rates of admission for congestive heart failure were higher among Hispanic patients compared with White patients; in more recent years, this disparity was eliminated.
- Achievable Benchmark:
- The 2008 top 4 State achievable benchmark for adult congestive heart failure admissions was 195 admissions per 100,000 population. The top 4 States that contributed to the achievable benchmark are Colorado, Oregon, Utah, and Vermont.
- At current rates of improvement, Hispanic patients could achieve the benchmark in 3 years and White patients could achieve it in 6 years. Black patients would need 12 years to achieve the benchmark.
Heart Attack Patients Given Timely Fibrinolytic Medication
Hospital patients with heart attack given fibrinolytic medication within 30 minutes of arrival, by race/ethnicity, 2005-2012
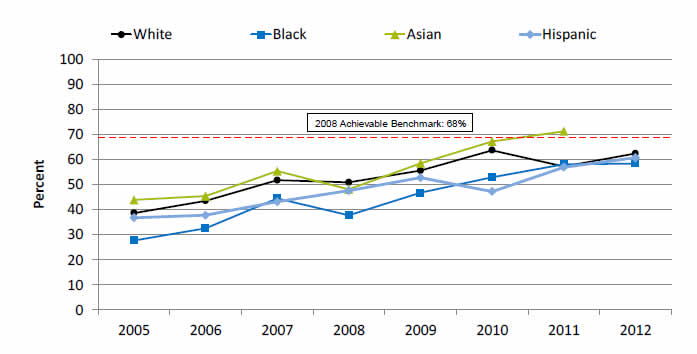
| Race/Ethnicity | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 |
|---|---|---|---|---|---|---|---|---|
| White | 38.7 | 43.6 | 51.8 | 51.0 | 55.7 | 63.8 | 57.3 | 62.5 |
| Black | 27.7 | 32.6 | 44.5 | 37.8 | 46.8 | 53 | 58.2 | 58.5 |
| Hispanic | 36.8 | 37.8 | 43.2 | 47.6 | 52.8 | 47.3 | 57 | 60.8 |
| Asian | 43.9 | 45.5 | 55.5 | 48.2 | 58.6 | 67.3 | 71.4 |
2008 Achievable Benchmark: 68%.
Source: Centers for Medicare & Medicaid Services, Medicare Quality Improvement Organization Program, 2005-2012.
Denominator Discharged hospital patients with a principal diagnosis of acute myocardial infarction and documented receipt of thrombolytic therapy during the hospital stay.
Note: Data for Asians in 2012 were statistically unreliable.
- Importance: Some heart attacks are caused by blood clots. Early actions, such as fibrinolytic medication, may open blockages caused by blood clots, reduce heart muscle damage, and save lives. To be effective, these actions need to be performed quickly after the start of a heart attack.
- Trends: From 2005 to 2012, the percentage of patients who received timely fibrinolytic medication improved overall and for all racial/ethnic groups.
- Groups With Disparities: Until 2011, the percentage of patients who received timely fibrinolytic medication was significantly higher for Whites than for Blacks.
- Achievable Benchmark:
- The 2010 top 5 State achievable benchmark was 68%. The top 5 States that contributed to the achievable benchmark are Arkansas, California, Georgia, Mississippi, and Texas.
- Asian heart attack patients achieved the benchmark in 2011.
- At the current rate of improvement, the achievable benchmark could be attained overall in 2 years. In addition, White, Black, and Hispanic heart attack patients should all reach the benchmark in 2 years.
Outcomes of Cardiovascular Care for Hispanics
| Measure | Most Recent Disparity | Disparity Change |
|---|---|---|
| Deaths per 1,000 hospital admissions with acute myocardial infarction (AMI), age 18+ | Same | No Change |
| Deaths per 1,000 hospital admissions with congestive heart failure (CHF), age 18+ | Better | No Change |
| Deaths per 1,000 hospital admissions with abdominal aortic aneurysm repair, age 18+ | Same | No Change |
| Deaths per 1,000 hospital admissions with coronary artery bypass graft, age 40+ | Same | No Change |
| Deaths per 1,000 hospital admissions with percutaneous transluminal coronary angioplasty, age 40+ | Same | No Change |
- Trends: Most measures of deaths from cardiovascular care for Hispanics were improving.
- Groups With Disparities:
- Hispanics and Whites had similar death rates when hospitalized for:
- Acute myocardial infarction.
- Abdominal aortic aneurysm repair.
- Coronary artery bypass graft surgery.
- Percutaneous transluminal coronary angioplasty.
- Hispanics had lower death rates than Whites when hospitalized for congestive heart failure and there was no change in this disparity over time.
- Hispanics and Whites had similar death rates when hospitalized for:
Inpatient Deaths With Heart Attack
Inpatient deaths per 1,000 adult hospital admissions with heart attack, by race/ethnicity, 2001-2012
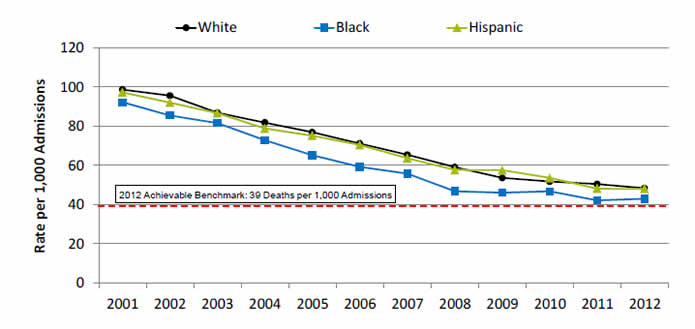
| Year | White | Black | Hispanic |
|---|---|---|---|
| 2001 | 98.7 | 92.2 | 97.2 |
| 2002 | 95.5 | 85.5 | 92.0 |
| 2003 | 86.9 | 81.6 | 86.6 |
| 2004 | 81.8 | 72.9 | 78.8 |
| 2005 | 76.9 | 65.2 | 75.2 |
| 2006 | 71.2 | 59.2 | 70.4 |
| 2007 | 65.4 | 55.8 | 63.6 |
| 2008 | 59.1 | 46.8 | 57.6 |
| 2009 | 53.7 | 46.1 | 57.5 |
| 2010 | 51.7 | 46.7 | 53.6 |
| 2011 | 50.5 | 42.1 | 48.1 |
| 2012 | 48.3 | 43.0 | 48.0 |
2012 Achievable Benchmark: 39 Deaths per 1,000 Admissions.
Source: Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project, State Inpatient Databases, 2001‐2012 disparities analysis files and AHRQ Quality Indicators, modified version 4.4.
Denominator Adults age 18 and over admitted to a non-Federal community hospital in the United States with acute myocardial infarction as principal discharge diagnosis.
Note: For this measure, lower rates are better. Rates are adjusted by age, major diagnostic category, all payer refined-diagnosis related group risk of mortality score, and transfers into the hospital.
- Importance: Racial disparities in heart attack care have been observed.
- Trends: From 2001 to 2012, the risk-adjusted inpatient mortality rate for hospital admissions with heart attack decreased significantly for all ethnic groups.
- Groups With Disparities: In 2012, Black patients had lower inpatient mortality rates for hospital admissions with heart attack than White patients.
- Achievable Benchmark:
- The 2008 top 4 State achievable benchmark for inpatient heart attack mortality was 48 deaths per 1,000 admissions. By 2012, this benchmark had been attained for all racial/ethnic groups.
- Because the 2008 benchmark was achieved by the total population, a new 2012 top 4 State achievable benchmark was set at 39 deaths per 1,000 admissions. The top 4 States that contributed to the achievable benchmark are Alaska, Arizona, Michigan, and Rhode Island.
- At current rates of improvement, all ethnic groups could reach the 2012 benchmark in approximately 2 years.



