Hospital ID# ___________ Unit ID# ___________ Date (mm/dd/yyyy) ___________
| Fill out for all beds |
Fill out if patient is intubated or has tracheostomy (trached) and is mechanically ventilated
(can use for patients not mechanically ventilated) |
| Bed # |
Intub / Trach & Mech Vent |
Date of Intubation
(mm/dd/yyyy) |
Sedation Scale |
Delirium Assessment |
| RASS/ SAS/ Not Used in Unit |
Target |
Actual |
CAM-ICU/ ASE/ ICDSC/ NU |
CAM-ICU P, N, X, UTA, NK |
ASE 0–10, X, UTA, NK |
ICDSC P, N, X, UTA, NK |
| If RASS – 5 to 4, NS or X, NK |
| If SAS – 1 to 7, NS or X, NK |
| |
Y N E |
/ / |
RASS SAS NU |
|
|
C A I NU |
|
|
|
| |
Y N E |
/ / |
RASS SAS NU |
|
|
C A I NU |
|
|
|
| |
Y N E |
/ / |
RASS SAS NU |
|
|
C A I NU |
|
|
|
| |
Y N E |
/ / |
RASS SAS NU |
|
|
C A I NU |
|
|
|
| |
Y N E |
/ / |
RASS SAS NU |
|
|
C A I NU |
|
|
|
| |
Y N E |
/ / |
RASS SAS NU |
|
|
C A I NU |
|
|
|
| |
Y N E |
/ / |
RASS SAS NU |
|
|
C A I NU |
|
|
|
| |
Y N E |
/ / |
RASS SAS NU |
|
|
C A I NU |
|
|
|
| |
Y N E |
/ / |
RASS SAS NU |
|
|
C A I NU |
|
|
|
| |
Y N E |
/ / |
RASS SAS NU |
|
|
C A I NU |
|
|
|
| |
Y N E |
/ / |
RASS SAS NU |
|
|
C A I NU |
|
|
|
Continued:
| Fill out for all beds |
Fill out if patient is intubated or has tracheostomy (trached) and is mechanically ventilated
(can use for patients not mechanically ventilated) |
| Bed # |
Intub / Trach & Mech Vent |
Highest Level of Mobility – 0 to 8
(refer to daily codes) |
Perceived Barrier to Achieving a Higher Level of Mobility – 0 to 15
(refer to daily codes) |
PT |
OT |
Events (Up to Three Events)
0 to 25
(refer to daily codes) |
Event 1
Required |
Event 2
Only if Needed |
Event 3
Only if Needed |
| |
Y N E |
|
|
Y
N
NK |
Y
N
NK |
|
|
|
| |
Y N E |
|
|
Y
N
NK |
Y
N
NK |
|
|
|
| |
Y N E |
|
|
Y
N
NK |
Y
N
NK |
|
|
|
| |
Y N E |
|
|
Y
N
NK |
Y
N
NK |
|
|
|
| |
Y N E |
|
|
Y
N
NK |
Y
N
NK |
|
|
|
| |
Y N E |
|
|
Y
N
NK |
Y
N
NK |
|
|
|
| |
Y N E |
|
|
Y
N
NK |
Y
N
NK |
|
|
|
| |
Y N E |
|
|
Y
N
NK |
Y
N
NK |
|
|
|
| |
Y N E |
|
|
Y
N
NK |
Y
N
NK |
|
|
|
| |
Y N E |
|
|
Y
N
NK |
Y
N
NK |
|
|
|
| |
Y N E |
|
|
Y
N
NK |
Y
N
NK |
|
|
|
ASE = Attention Screening Exam; CAM-ICU = Confusion Assessment Method for the ICU; ICDSC = Intensive Care Delirium Screening Checklist; E = Empty; Intub = Intubation; Mech Vent = Mechanical Ventilation; N = Negative/No; NK = Not Known; NU = Not Used in this Unit; OT = Occupational Therapy; PT = Physical Therapy; P = Positive; RASS = Richmond Agitation and Sedation Scale; SAS = Riker Sedation-Agitation Scale; Trach = Tracheostomy; UTA = Unable to Assess; X = Not Performed; Y = Yes.
Daily Codes
| Highest Level of Mobility |
Perceived Barrier to Acheiving a Higher Level of Mobility |
Events |
- Nothing: passively rolled or exercised by staff, but not actively moving (includes raising head of bed to upright position without patient participation in movement, chest physical therapy, and splinting).
- Transfer bed to chair without standing: hoist, passive lift, or slide to the chair without standing.
- Sitting in bed/exercises in bed: any activity in bed, including active rolling, bridging, active exercises, active movement from supine to sitting position, use of cycle ergometer, use of tilt table, not moving out of bed or over the edge of the bed.
- Sitting at edge of bed: actively sitting over the side of the bed with some trunk control (may be assisted).
- Standing: weight bearing through feet in standing position with or without assistance; may include use of a standing lifter.
- Transfer from bed to chair with standing: able to step or shuffle through standing to chair; this involves actively transferring weight from one leg to another to move to chair.
- Marching in place: able to walk in place by lifting alternate feet (must be able to step at least four times, two for each foot) with or without assistance.
- Walking: walking away from the bed/chair by at least four steps (two for each foot) assisted by a person/people or gait aid, or unassisted.
- Unknown: it is unknown regarding what activity, if any, occurred.
|
- Not applicable — patient at highest possible level of mobility.
- Bed rest orders.
- Patient on comfort/palliative care measures.
- Patient sedated (Richmond Agitation Sedation Scale [RASS] -4 or -5; or Riker Sedation-Agitation Scale [SAS] 1 or 2) and on infusion of benzodiazepine, narcotic, propofol, or other sedative.
- Patient sedated (RASS -4 or -5; or SAS 1 or 2), but NOT on infusion of benzodiazepine, narcotic, propofol, or other sedative.
- Medically inappropriate (orthopedic reason, i.e., fracture of long bone, spine, or pelvis).
- Medically inappropriate (circulatory or respiratory reason) as delineated in the medical screening algorithm.
- Medically inappropriate (new deep vein thrombosis, or DVT) as delineated in the medical screening algorithm.
- Medically inappropriate (femoral sheath) as delineated in the medical screening algorithm.
- Medically inappropriate (for any other reason, i.e., unstable, active gastrointestinal bleeding).
- Patient unavailable throughout the day.
- Staffing (registered nurse, physical therapist, respiratory therapist) unavailable throughout the day.
- Patient declined mobilization throughout the day.
- Patient is too weak to progress to higher level of mobility.
- Other barrier not listed above.
- Unknown barrier.
|
- None.
- Endotracheal tube dislodgement.
- Tracheostomy dislodgement.
- Nasal feeding tube dislodgement.
- Oral feeding tube dislodgement.
- Percutaneous feeding tube dislodgement.
- Central venous catheter dislodgment (not femoral site), including peripherally inserted central catheter line.
- Central venous catheter dislodgement (femoral site).
- Arterial catheter dislodgement (not femoral site).
- Arterial catheter dislodgement (femoral site).
- Dialysis catheter dislodgement (not femoral site), including tunneled or nontunneled.
- Dialysis catheter dislodgement (femoral site).
- Pulmonary artery catheter dislodgement (not femoral).
- Pulmonary artery catheter dislodgement (femoral site).
- Chest tube dislodgement.
- Wound or dressing disruption or new bleeding at site.
- Cardiac device dislodgement (i.e., temporary pacemaker wire, ventricular assist device, intra-aortic balloon pump.
- Hypotension (change in mean arterial pressure (MAP) to <55 mmHg, or if intervention required [i.e., fluid bolus or new/increased vasopressor dose]).
- Hypertension (change in MAP to >140 mmHg, or if intervention required).
- Desaturation (02 sat <85% or if intervention required [i.e., increase in Fi02]).
- Cardiac arrest requiring cardiopulmonary resuscitation.
- New arrhythmia (excludes sinus tachycardia, premature ventricular contractions (PVC), or pre-existing arrhythmia that did not worsen during mobilization).
- Fall WITH staff assisting in lowering patient.
- Fall WITHOUT staff assisting in lowering patient.
- Death.
- Other.
|
Instructions for Daily Early Mobility Data Collection Tool
Please complete this form once a day, every day. If possible, complete it around the same time each day, hopefully during patient rounds.
Patients are considered mechanically ventilated on a specific day if they were mechanically ventilated at the time of observation.
All of the contraindications are listed at the end of the data collection tool. Please print the data collection sheet with the contraindications on the back for ease of data collection.
**This tool may also be used for patients who are not mechanically ventilated.**
| DATA FIELD |
DIRECTIONS |
| Hospital |
Enter the name of your hospital. |
| ICU |
Enter the name of your unit. |
| Date |
Enter today’s date as MM/DD/YYYY format (e.g. 01/31/2014). |
| Bed # |
Enter all the bed numbers on the form, regardless of whether the patient is on mechanical ventilation. Include empty beds. |
| Intub/Trach & Mech Vent: Is the patient currently receiving mechanical ventilation? |
Enter for all patients. If the bed is empty, leave blank. Mechanical ventilation is defined as receiving ventilator support via an endotracheal tube or tracheostomy tube.
- Patients treated with noninvasive ventilation are counted as N.
- Circle Y if the patient is currently intubated/trached and mechanically ventilated.
- Circle N if the patient is not currently intubated/trached and mechanically ventilated.
- Circle E if there is no patient in the bed.
For any specific patient, if the patient is not currently intubated/trached AND on mechanical ventilation, STOP. Do not enter any more information regarding that bed for this date.
If you entered Y, all of the following information is required.
If you have entered N, the following information is not required. However, you may collect and enter this information if it would be of use to your unit.
If you have entered E, STOP. Do not enter any more information regarding that bed for this date.
|
| Date of Intubation |
Enter the date that the patient was intubated using an MM/DD/YYYY format (e.g., 06/01/2012).
Evaluate daily for patients receiving full vent support.
- DO NOT use dates from reintubation following self-extubation.
- If the patient is reintubated following less than 24 hours after extubation, use first intubation date.
|
Sedation Scale
| DATA FIELD |
DIRECTIONS |
| RASS/SAS/Not Used in This Unit: What sedation scale do you use on your unit? |
Evaluate daily for patients receiving mechanical ventilation.
- Circle RASS if your unit uses the Richmond Agitation Sedation Scale (RASS).
- Circle SAS if your unit uses the Riker Sedation-Agitation Scale (SAS).
- Circle NU if your unit either does not use a sedation scale or uses a scale other than RASS or SAS.*
*If you circle NU, skip to the Delirium Assessment column. DO NOT enter information into either the Target or Actual columns. |
Since you are a RASS or SAS user, please record the target and actual scores for RASS or SAS assessment closest to 10 a.m. If two scores were collected equidistant from 10 a.m., choose the earlier score.
(Evaluated daily for mechanically ventilated patients with R or S entered in the RASS/SAS/Not used in this unit column).
The Society of Critical Care Medicine’s 2013 pain/agitation/delirium (PAD) clinical practice guidelines recommend the RASS and SAS as the most valid and reliable sedation assessment tools for measuring the quality and depth of sedation in adult intensive care unit patients.
| DATA FIELD |
DIRECTIONS |
| RASS: Target/Actual: What are the target and actual RASS scores for this patient? |
RASS – Only for patients receiving mechanical ventilation and where RASS/SAS/Not Used in This Unit = RASS
Enter the score closest to 10 a.m. If two scores were collected equidistant from 10 a.m., choose the earlier score.
- Enter the target RASS sedation numeric scale value, choosing from -5 to 4.
- Enter NS if the target RASS sedation level was not set.
- Enter NK if a target RASS sedation level was set but is not known.
- Enter NK if you don’t know whether a target RASS sedation level was actually set.
- Enter the RASS actual sedation numeric scale value, choosing from -5 to 4.
- Enter X if an actual RASS sedation level was not scored.
- Enter NK if an actual RASS sedation level was scored, but is not known.
Enter NK if you don’t know whether an actual RASS sedation level was scored. |
| SAS: Target/Actual: What are the target and actual SAS scores for this patient? |
SAS - Only for patients receiving mechanical ventilation and where RASS/SAS/Not Used in This Unit = SAS
Enter the score closest to 10 a.m. If two scores were collected equidistant from 10 a.m., choose the earlier score.
- Enter the target SAS sedation numeric scale value, choosing from 1 to 7.
- Enter NS if the target SAS sedation level was not set.
- Enter NK if a target SAS sedation level was set, but is not known.
- Enter NK if you don’t know whether a target SAS sedation level was actually set.
- Enter the actual SAS sedation numeric scale value, choosing from 1 to 7.
- Enter X if an actual SAS sedation level was not scored.
- Enter NK if an actual SAS sedation level was scored, but is not known.
- Enter NK if you don’t know whether an actual SAS sedation level was scored.
|
Delirium Assessment
The Society of Critical Care Medicine’s 2013 pain/agitation/delirium (PAD) clinical practice guidelines recommend the Confusion Assessment for the ICU (CAM-ICU) or the Intensive Care Delirium Screening Checklist (ICDSC) as the most valid and reliable delirium screening tools, and that moderate- to high-risk patients be screened at least once per nursing shift.
ASE (Attention Screening Exam) is the second step of the CAM-ICU. While it is not specifically recommended for use by the SCCM PAD Guidelines, it is a good tool to use while your unit is getting set up to do the full CAM-ICU. The results of the ASE may be abnormal due to disease, drugs, or other causes.
| DATA FIELD |
DIRECTIONS |
| RASS/SAS/Not Used in This Unit: What sedation scale do you use on your unit? |
Evaluate daily for patients receiving mechanical ventilation.
- Circle RASS if your unit uses the Richmond Agitation Sedation Scale (RASS).
- Circle SAS if your unit uses the Riker Sedation-Agitation Scale (SAS).
- Circle NU if your unit either does not use a sedation scale or uses a scale other than RASS or SAS.*
*If you circle NU, skip to the Delirium Assessment column. DO NOT enter information into either the Target or Actual columns. |
If you are a CAM-ICU, ICDSC, or ASE user, please record the most recent CAM-ICU, ICDSC, or ASE assessment closest to 10 a.m. If two scores were collected equidistant from 10 a.m., choose the earlier score. The CAM-ICU can be done while on or off sedation/analgesics, and it is up to the clinical team to interpret the results of the delirium assessment in light of the presence or absence of sedatives/analgesics.
(Evaluated daily for patients with C , A, or I entered in the CAM-ICU/ASE/ICDSC/NU).
CAM-ICU
| DATA FIELD |
DIRECTIONS |
| CAM-ICU: Is the patient positive or negative for delirium? |
(Only for patients receiving mechanical ventilation and where CAM-ICU/ASE/ICDSC/Not Used in This Unit = C)
Enter the score closest to 10 a.m. If two scores were collected equidistant from 10 a.m., choose the earlier score.
- Enter P if the patient is positive for delirium based on CAM-ICU assessment.
- Enter N if the patient is negative for delirium based on CAM-ICU assessment.
- Enter UTA if unable to assess (e.g., RASS = -4 or -5 OR SAS = 1 or 2).
- Enter X if CAM-ICU assessment was not completed.
- Enter NK if CAM-ICU was completed, but results are not known.
Enter NK if CAM-ICU if you don’t know whether the exam was performed. |
ASE - Feature 2 of the CAM-ICU
| DATA FIELD |
DIRECTIONS |
| ASE: What is the patient’s ability to pay attention? |
(Only for patients receiving mechanical ventilation and where CAM-ICU/ASE/ICDSC/Not Used in This Unit = A)
The goal of this 10- to 20-second test is to determine if a patient can follow a simple command (pay attention) for that period of time. Inattention is the cardinal feature of delirium and must be present to diagnose delirium. For centers not using the full CAM-ICU, conducting the ASE is a good barometer of the presence or absence of delirium. This test may be abnormal due to disease, drugs, or other causes.
The exam consists of the provider reading the following sequence of letters:
S A V E A H A A R T or C A S A B L A N C A or A B A D B A D D A Y
The patient is told to squeeze the provider’s hand when the letter A is stated. An error is defined as no squeeze with letter A or a squeeze on a letter other than A. The number of errors is counted. Inattention is present if the patient commits more than two errors. If the patient squeezes on every letter or doesn’t squeeze on any letter, then assign an error count of 10.
Enter the score closest to 10 a.m. If two scores were collected equidistant from 10 a.m., choose the earlier score.
- Enter the number of errors, 0 to 10.
- Enter UTA if unable to assess (i.e., RASS = -4 or -5 OR SAS = 1 or 2).
- Enter X if the exam was not performed.
- Enter NK if the exam was performed, but the number of errors is not known.
- Enter NK if you don’t know whether the exam was performed.
The Society of Critical Care Medicine’s 2013 pain/agitation/delirium clinical practice guidelines recommend the CAM-ICU or the ICDSC as the most valid and reliable delirium screening tools, and that moderate- to high-risk patients be screened at least once per nursing shift.
If this is not yet feasible in your unit, we recommend that patients at least undergo the ASE once daily. The ASE is feature 2 of the CAM-ICU and this 10- to 20-second test of attention is the cardinal feature of a delirium diagnosis. |
Mobility
| DATA FIELD |
DIRECTIONS |
| Highest level of mobility: What was the highest level of mobility achieved by the patient in the last 24 hours? |
Evaluate every day.
Mobility codes are listed on the back of the data collection tool.
- Nothing: passively rolled or exercised by staff, but not actively moving (includes raising head of bed to upright position without patient participation in movement, chest physical therapy, and splinting).
- Transfer bed to chair without standing: hoist, passive lift, or slide to the chair without standing.
- Sitting in bed/exercises in bed: any activity in bed, including active rolling, bridging, active exercises, active movement from supine to sitting position, use of cycle ergometer, use of tilt table, not moving out of bed or over the edge of the bed.
- Sitting at edge of bed: actively sitting over the side of the bed with some trunk control (may be assisted).
- Standing: weight bearing through feet in standing position with or without assistance; may include use of a standing lifter.
- Transfer from bed to chair with standing: able to step or shuffle through standing to chair; this involves actively transferring weight from one leg to another to move to chair.
- Marching in place: able to walk in place by lifting alternate feet (must be able to step at least four times, two for each foot) with or without assistance.
- Walking: walking away from the bed/chair by at least four steps (two for each foot) assisted by a person/people or gait aid, or unassisted.
- Unknown: it is unknown regarding what activity, if any, occurred.
|
Perceived barrier to achieving a higher level of mobility:
What prevented the patient from being mobilized to a higher level? |
Enter the code associated with the answer. For example, enter 2 for "Patient on comfort/palliative care measures." If multiple codes apply to a patient, please select the lowest number.
Perceived barrier codes are listed on the back of the data collection tool.
- Not applicable – patient at highest possible level of mobility.
- Bed rest orders.
- Patient on comfort/palliative care measures.
- Patient sedated (RASS -4 or -5; or SAS 1 or 2) and on infusion of benzodiazepine, narcotic, or propofol.
- Patient sedated (RASS -4 or -5; or SAS 1 or 2), but NOT on infusion of benzodiazepine, narcotic, or propofol.
- Medically inappropriate (orthopedic reason, e.g., fracture of long bone, spine, or pelvis).
- Medically inappropriate (circulatory or respiratory reason) as delineated in the medical screening algorithm.
- Medically inappropriate (new deep vein thrombosis) as delineated in the medical screening algorithm on page 12.
- Medically inappropriate (femoral sheath) as delineated in the medical screening algorithm.
- Medically inappropriate (for any other reason; e.g., unstable, active gastrointestinal bleeding).
- Patient unavailable throughout the day.
- Staffing (registered nurse, physical therapist, respiratory therapist) unavailable throughout the day.
- Patient declined mobilization throughout the day.
- Patient too weak to progress to higher level of mobility.
- Other barrier not listed above.
- Unknown barrier.
|
| Physical Therapy: Did a physical therapist (PT) evaluate or treat the patient within the last 24 hours? |
- Circle Y if the patient was evaluated or treated by a PT in the past 24 hours.
- Circle N if the patient was NOT evaluated or treated by a PT in the past 24 hours.
- Circle NK if it is not known if the patient was evaluated or treated by a PT in the past 24 hours.
|
| Occupational Therapy: Did an occupational therapist (OT) evaluate or treat the patient within the last 24 hours? |
- Circle Y if the patient was evaluated or treated by an OT in the past 24 hours.
- Circle N if the patient was NOT evaluated or treated by an OT in the past 24 hours.
- Circle NK if it is not known if the patient was evaluated or treated by an OT in the past 24 hours.
|
| Events: Did the patient have an "event" (as defined on the back of the data collection sheet) while being mobilized within the last 24 hours? |
Enter a code in the Event 1 – Required column. If there was no event, choose 0. If multiple events occurred, you can enter up to two more events.
Event codes are listed on the back of the data collection sheet.
- None
- Endotracheal tube dislodgement.
- Tracheostomy dislodgement.
- Nasal feeding tube dislodgement.
- Oral feeding tube dislodgement.
- Percutaneous feeding tube dislodgement.
- Central venous catheter dislodgment (not femoral site), including peripherally inserted central catheter line.
- Central venous catheter dislodgement (femoral site).
- Arterial catheter dislodgement (not femoral site).
- Arterial catheter dislodgement (femoral site).
- Dialysis catheter dislodgement (not femoral site), including tunneled or nontunneled.
- Dialysis catheter dislodgement (femoral site).
- Pulmonary artery catheter dislodgement (not femoral).
- Pulmonary artery catheter dislodgement (femoral site).
- Chest tube dislodgement.
- Wound or dressing disruption or new bleeding at site.
- Cardiac device dislodgement (e.g., temporary pacemaker wire, ventricular assist device, intra-aortic balloon pump).
- Hypotension (change in mean arterial pressure to <55 mmHg, or if intervention required [e.g., fluid bolus or new/increased vasopressor dose]).
- Hypertension (change in MAP to >140 mmHg, or if intervention required).
- Desaturation (02 saturation <85% or if intervention required [e.g., increase in Fi02]).
- Cardiac arrest requiring cardiopulmonary resuscitation.
- New arrhythmia (excludes sinus tachycardia, premature ventricular contractions, or pre-existing arrhythmia that did not worsen during mobilization).
- Fall WITH staff assisting in lowering patient.
- Fall WITHOUT staff assisting in lowering patient.
- Death.
- Other
|
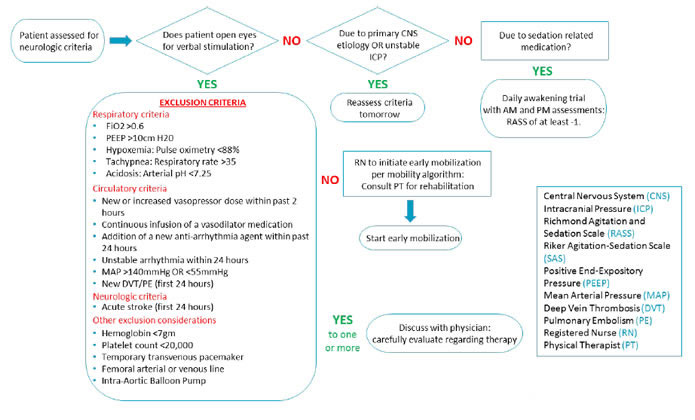
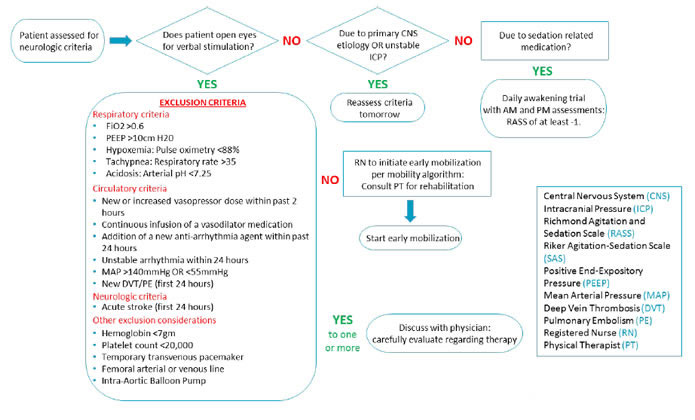
Medical Screening Algorithm
Medical screening algorithm to evaluate patient appropriateness for rehabilitation.