Measure Descriptions for Low Tidal Volume Ventilation: Facilitator Guide
AHRQ Safety Program for Mechanically Ventilated Patients
Slide 1: Measure Descriptions for Low Tidal Volume Ventilation
Say:
In this module, you will learn about the data measures and definitions you will use to evaluate low tidal volume ventilation, or LTVV, process and outcome measures in your unit.
Slide 2: Learning Objectives
Say:
After this session, you will be able to collect and enter LTVV data using the LTVV Data Collection Tool, understand the definitions of the data elements, and locate necessary data elements.
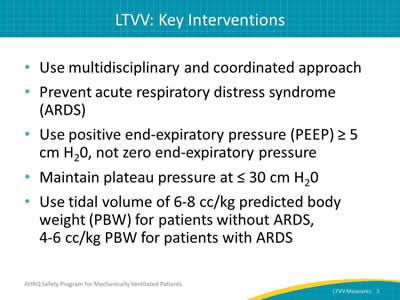
Slide 3: LTVV: Key Interventions
Ask:
What are the key interventions involved in implementing a daily LTVV protocol?
Say:
The first intervention is to use a multidisciplinary and coordinated approach to ensure the use of appropriate tidal volume for your patients. The second key intervention is to prevent acute respiratory distress syndrome (ARDS) through the use of LTVV. The next intervention is to implement positive end-expiratory pressure (PEEP) greater than or equal to 5 cm H20, rather than zero end-expiratory pressure. Fourth, aim to maintain plateau pressure at less than or equal to 30 cm/ H20. Finally, use a tidal volume of 6-8 cc/kg whenever possible and when clinically indicated.
Slide 4: Data Collection
Say:
Collecting the data for LTVV can require a significant time commitment as well as manpower. However, these data can not only be used to drive quality improvement efforts, but can also be used for quality improvement process development. Having these data at your disposal will provide quantifiable measures of care practices, which assists in guiding conversations about improving patient safety. This information can also be used to help justify the necessary human, financial, and equipment resources.
Slide 5: LTVV Data Collection Tool
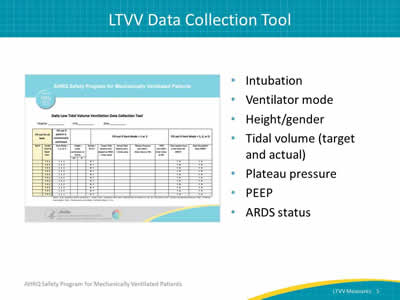
Say:
The LTVV Collection Tool is a resource you can use to collect information on your LTVV ventilation measures. It includes information about when the patient was intubated, which ventilator mode is being used, the height and gender of the patient, the target and actual tidal volume, the plateau pressure and PEEP at the time of observation, and if the patient has a diagnosis or a risk factor for ARDS. Try to complete this tool at approximately the same time each day and preferably during patient rounds.
Slide 6: Data Collection: Intubation and Ventilator Mode
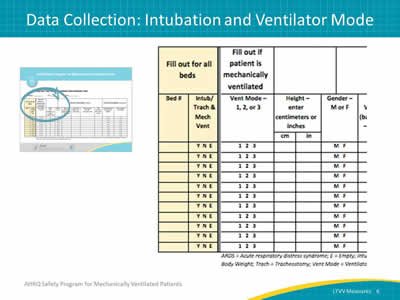
Say:
The first half of the data collection tool focuses on intubation and ventilator mode.
Slide 7: Let’s Begin…
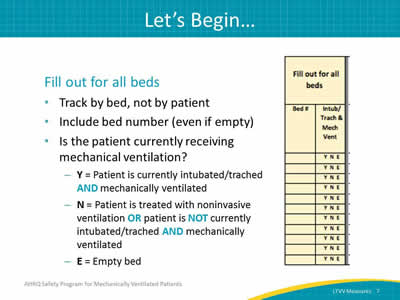
Say:
The low tidal volume measures are tracked by bed, not by a specific patient. It is most useful to track all beds in the unit, whether they are filled or not. Mechanical ventilation is defined as receiving ventilator support via an endotracheal tube or tracheostomy tube (trached). Begin by filling out the bed number, and whether the patient in bed was intubated or trached AND on mechanical ventilation at the time of observation. The codes you will use are listed on the collection tool itself. Use the Y code if the patient is intubated or trached AND on mechanical ventilation. If the patient is being treated with noninvasive ventilation or the patient is NOT currently intubated or trached AND mechanically ventilated, use the N code. If the bed is empty, use the E code. If the patient is not currently intubated/trached AND on mechanical ventilation, go no further. Stop and do not enter any more information regarding that bed for the day.
Slide 8: Ventilator Modes—Volume-Cycled Modes
Say:
The next field is the ventilator mode. Select the ventilator mode for all patients receiving mechanical ventilation. Depending on which mode of ventilation is present at the time of observation, circle 1, 2, or 3 accordingly. Circle number 1 if the ventilator is set to one of the following volume cycled modes: assist control, synchronized intermittent mandatory ventilation, volume support, pressure regulated volume controlled, or continuous mandatory ventilation.
Slide 9: Ventilator Modes—Pressure-Cycled Modes
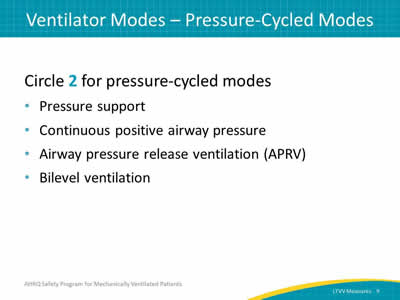
Say:
Circle 2 if the ventilator is set to one of the following pressure cycle modes: pressure support, continuous positive airway pressure, pressure control, airway pressure release ventilation (APRV), or bilevel ventilation.
Slide 10: Ventilator Modes—Other Modes
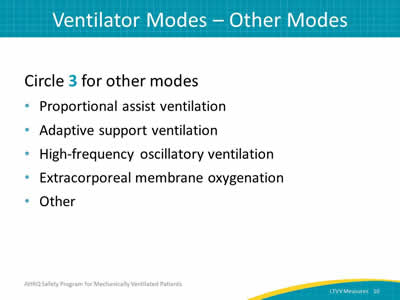
Say:
Circle 3 if the ventilator is set to one of the following other modes: proportional assist ventilation, adaptive support ventilation, high-frequency oscillatory ventilation, extracorporeal membrane oxygenation, or another mode not listed here.
Slide 11: For Vent Modes 1 and 2 Only
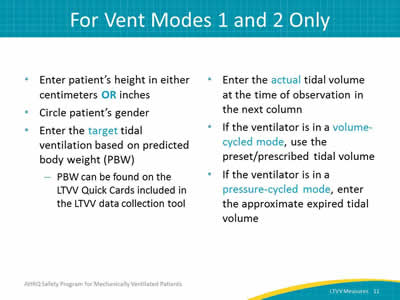
Say:
If 1 or 2 is selected for any specific patient, continue to the next column where the patient’s height is entered in either centimeters or inches. In the following column, circle the patient’s gender. In the next column, enter the target tidal ventilation based on predicted body weight. Enter the actual tidal volume ventilation at the time of observation in the next column. If the ventilator mode is in a volume cycled mode, user the preset/prescribed tidal volume. If the ventilator is in a pressure-cycled mode, enter the approximate expired tidal volume.
Slide 12: For Vent Modes 1 and 2 Only
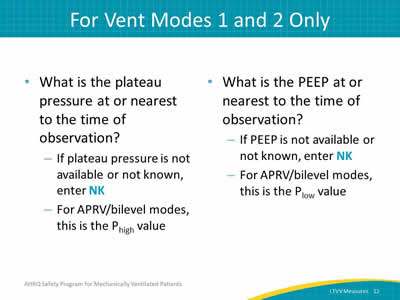
Say:
For patients receiving mechanical ventilation with ventilator mode 1 or 2, what is the plateau pressure at the time or nearest the time of observation? If it is not available or is not known, enter NK. For APRV/bilevel modes, this is the Phigh value. (As a reminder, If you entered 3 for the ventilator mode, you should NOT be collecting this information.)
The next column refers to PEEP. What is the PEEP at the time or nearest the time of observation? If it is not available or not known, enter NK. For APRV/bilevel modes, this is the Plow value.
Slide 13: Data Collection: ARDS
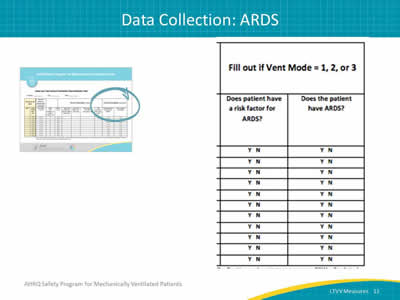
Ask:
Does the patient have a risk factor for ARDS?
Say:
Evaluate daily for patients receiving mechanical ventilation with ventilator mode at 1, 2, or 3.
Slide 14: For ALL Vent Modes (1, 2, or 3)
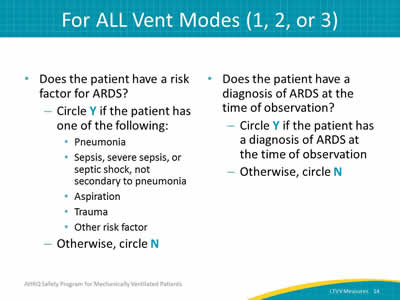
Say:
If the patient has one or more of the following, circle Y: pneumonia, sepsis, severe sepsis, or septic shock not secondary to pneumonia, aspiration, trauma, or other risk factor (such as massive transfusion or acute pancreatitis). If the patient does not have any risk factors for ARDS, circle N. If the patient has an actual ARDS diagnosis at the time of observation, circle Y in the following column, otherwise, circle N.
Slide 15: Data Measures Guide
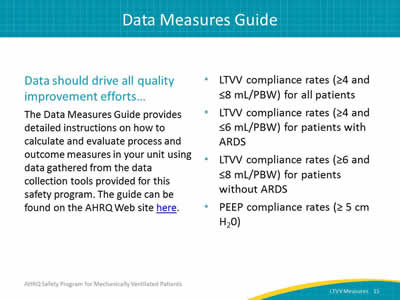
Say:
Data should drive all quality improvement projects. The Data Measures Guide provides detailed instructions on how to calculate and evaluate process and outcome measures in your unit using data gathered from the data collection tools provided for this safety program. You can use this guide to determine various compliance rates for LTVV measures, among many other things. The guide can be downloaded from the AHRQ Web site (Word File, 553 KB).
Slide 16: Questions?
Ask:
Are there any questions?



