Module 1: Understanding Why Change Is Needed
Hospital: >50–200 beds
Pilot Units: Med/Surg, Geri/Psych
Challenge: Lack of leadership buy-in or support.
Solution: Have a physician serve on the Implementation Team.
Description: The Implementation Team includes a physician member. This individual leads the hospital’s annual root cause analysis (RCA), serves as the keeper of the evidence base, and holds a specialty/position relevant to fall prevention (e.g., physical medicine, rehabilitation, hospitalist). The physician is an equal member of the team but provides a physician’s perspective.
The team decided that any team that meets in a post-fall huddle should have a medical provider in the huddle; when a patient falls, he or she needs to be evaluated by a medical provider. The team speaks with physicians on a regular but informal basis to share information or get their opinion on actions under consideration. In addition, the team uses Lean quality improvement (QI) methods.
What You Can Do:
- Ask a physical medicine physician, rehabilitation physician, hospitalist, or other physician in your hospital to become a member of the Fall Prevention Implementation Team.
Module 1: Understanding Why Change Is Needed
Hospital: >400 beds
Pilot Units: Med/Surg, Telemetry
Challenge: Lack of leadership buy-in or support.
Solution: Get the chief executive officer (CEO) involved.
Description: During a meeting, the hospital’s CEO told a personal story about his mother, who experienced a fall in the hospital. The chief nursing officer (CNO), chief medical officer, and chief quality officer also attended the meeting. They were all engaged as the project moved forward and challenges arose.
What You Can Do:
- Determine how the administration/C-suite can be involved in the project.
Module 1: Understanding Why Change Is Needed
Hospital: ≤50 beds
Pilot Unit: Acute Rehab
Challenge: Lack of leadership buy-in or support.
Solution: Have a leadership sponsor.
Description: The Director of Quality and Risk Management served as the leadership sponsor for this initiative. She attended and participated in the in-person training. She secured the support and resources for staff to focus on this effort, including pilot testing changes sequentially over time on various units with various staff and including revisions to organizational processes and the electronic health record (EHR). She checked in frequently with the day-to-day project leaders. She worked with the project team to present the initiative to top leadership at various times, in order to secure their ongoing commitment to the changes and the resources needed for training and to ensure sustainability. These actions involved leadership in supporting the patient care teams’ goal to prevent falls for their patients.
What You Can Do:
- Consider approaching top-level administration, the board of trustees, and other leadership groups to ensure buy-in.
- Determine whether your facility’s EHR can be modified.
- Using gap analysis, determine whether any areas of the fall prevention process can be streamlined to make patient care easier for staff.
Module 1: Understanding Why Change Is Needed
Hospital: >200–400 beds
Pilot Units: Telemetry, Geri/Psych
Challenge: Lack of leadership buy-in or support.
Solution: Get the CNO involved.
Description: The CNO attended fall-prevention training at the hospital. She understands the project and holds all accountable. She holds weekly meetings with the Fall Team Lead. The Team Lead also presents all results at Nursing Leadership meetings. The CNO looks at the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) results regarding responsiveness to call bells as an indicator of the success of purposeful rounding, since responsiveness should reduce call bell use.
What You Can Do:
- Ask the CNO or other executive leadership to commit to participation in regular meetings with the Fall Prevention Team to check on progress, identify any gaps, and serve as an advocate for the team.
Module 1: Understanding Why Change Is Needed
Hospital: ≤50 beds
Pilot Unit: Acute Rehab
Challenge: Lack of leadership buy-in or support.
Solution: Communicate progress to senior leadership.
Description: The Fall Prevention Team gave a presentation to senior leaders to provide an update on their work over the past year and to secure their ongoing support and commitment to resources. The team discussed the following topics:
- What the team wanted from the Senior Leadership Team. It was looking for leadership support for implementation—not for content, as the team of experts that worked on this effort did a great job. This is an example of deference to expertise—letting the people closest to the work and with the most knowledge of the work do it and relying on senior leaders to remove any barriers.
- A historical perspective about this project, as well as the hospital’s processes and data.
- A brief review of strategies that have made a difference so far. These include proactive rounding and video monitoring.
- An update on the risk assessment process changes, which helped the leaders see how much easier it was going to be for the Interdisciplinary Team to share information. The team highlighted the differences between old and new processes. (They are transitioning to risk-based assessment and interventions tied to risk. In the past, they used more of a definitional risk-based assessment and interventions.)
- Plans for a rollout of the new risk-based assessment process systemwide.
What You Can Do:
- Share information with your board and other administrative leaders through multiple avenues (e.g., meetings, reports).
- Show them ongoing progress and improvement.
Module 1: Understanding Why Change Is Needed
Hospital: >200–400 beds
Pilot Units: Telemetry, Geri/Psych
Challenge: Lack of leadership buy-in or support.
Solution: Provide data when discussing fall prevention needs.
Description: The team did a deep dive report for leadership that covered falls in several units for 3 months when there were a total of 50 falls. The report was presented to administration and seeing these data engaged the administration.
In response to these findings, the administration suggested some changes in the audit tools. They also identified the need to increase staff engagement, coordinate post-fall huddles with event reporting via the hospital’s software, and have the Information Technology (IT) Department assist with mobility assessment documentation. In addition, the administration directed the Falls Team to bring the results of the report to staff via the Unit Champions.
What You Can Do:
- Conduct surveys or compile reports of available data to underscore the importance of reducing falls in the facility and to engage leadership in understanding why change is needed.
Module 1: Understanding Why Change Is Needed
Hospital: >400 beds
Pilot Units: Med/Surg, Telemetry
Challenge: Resource support—professional time and money.
Solution: Conduct a value analysis/needs assessment.
Description: The team conducted a value analysis/needs assessment to determine whether to purchase bedside commodes or walkers. Originally, staff thought walkers were needed. However, a review of post-fall huddle reports revealed that commodes were needed. The team presented data showing that 95 percent of falls in this unit happened when patients tried to travel to the toilet. Increased use of commodes for this unit would decrease the distance patients travel to use the toilet.
After a commode was placed in all rooms on the unit, falls decreased 27 percent. On another unit, which also received some commodes, falls decreased 19 percent. Among the interventions on these two patient care units, the purchase of commodes had the biggest impact on fall reduction. In addition, it boosted staff’s morale, since the idea came from staff on the unit.
What You Can Do:
- Review data to ensure that the most effective intervention is selected.
- Ask unit-level staff what they are seeing related to patient falls and involve them in the solution gathering process.
Module 2: How To Manage Change
Hospital: >50–200 beds
Pilot Units: Med/Surg, Geri/Psych
Challenge: Delineating Implementation Team member roles.
Solution: Clearly define role of Unit Champion.
Description: The hospital had Unit Champions even before the prevention initiative started, but their roles needed to be better defined. As part of the initiative action plan, the champion role was defined, and Fall Champions were empowered to take the lead on the pilot units. The Unit Champions were provided with detailed lesson plans to use for unit staff education. Unit Champions were also responsible for data collection. The prevention initiative action plan is monitored by the Quality Department. Aggregate RCA determined a need for information to be shared. Unit Champions took on the responsibility of sharing fall prevention information and data on their units.
What You Can Do:
- Review job duties and expectations with all staff who will be on the Implementation Team.
- Clearly define the role of the Unit Champion and ensure that all staff understand their responsibilities related to fall prevention.
- Educate all staff on fall prevention activities and monitor to ensure that fall prevention activities are adequately implemented.
Module 2: How To Manage Change
Hospital: >400 beds
Pilot Units: Rehab, Medical, Cardiac Intermediate Care Unit (IMC)
Challenge: Effectively involving the pharmacist in the Fall Prevention Team.
Solution: Clearly define the role of the team’s hospital pharmacist.
Description: Frontline staff nurses needed more information about regularly-prescribed medications as a risk factor for falls on each specific unit. The team pharmacist provided this education. The pharmacist attends all team meetings and acts as a resource for medications. The pharmacist makes nurses more aware of medications as a risk factor and teaches patients and families about the side effects of medications.
What You Can Do:
- Consider how you will tap into the expertise of your hospital pharmacist (a member on the interdisciplinary team or as an ad hoc subject matter expert to consult on specific patients as appropriate).
Module 2: How To Manage Change
Hospital: >400 beds
Pilot Units: Med/Surg, Telemetry
Challenge: Delineating Implementation Team member roles.
Solution: Use patient care technicians (PCTs) more effectively in fall prevention activities.
Description: The Fall Prevention Team made the change from hourly rounding to purposeful rounding on the pilot units. PCTs were educated on purposeful rounding, since they are the ones who usually bring patients to the toilet. A complimentary meal (lunch or other) was included with the educational course to reinforce the PCTs’ value to the process. All leaders attended the complimentary meal.
During the educational session, the PCTs learned the following strategies: incorporating scripting during purposeful rounding, asking patients if they need to use the toilet, posting a toileting schedule in patients’ rooms, and telling patients when toileting will occur. Nurse managers monitor compliance and conduct focused rounding (including teach-back) with patients who are at high risk to ensure they have been rounded on and understand their fall risk. The educational session was found to boost PCTs’ morale.
The hospital is faced with increased patient days and several new employees. Content from the educational sessions will be incorporated into new employee orientation.
What You Can Do:
- Consider ways hospital leadership can communicate the importance of and support of new initiatives with PCTs and other specific team members.
- Incorporate content from the educational sessions on purposeful rounding into new employee orientation.
- Consider shadowing pilot unit staff to ensure that tasks are completed correctly and in a timely manner after initial implementation.
Module 2: How To Manage Change
Hospital: >50–200 beds
Pilot Units: Med/Surg
Challenge: Effectively planning for Implementation Team responsibilities.
Solution: Expand the role of the Unit Champion to include team responsibilities.
Description: To streamline team tasks, the role of the Unit Champion on the pilot units was expanded to include the following quality improvement activities:
- Participating in a comprehensive review of the fall policy and procedures.
- Reviewing evidence and best practices for fall prevention.
- Incorporating key interventions in the policy.
- Developing a fall prevention knowledge assessment tool for staff.
- Conducting audits to look at adherence to processes.
- Providing education for staff, both at scheduled times and during audits and other observations (including identifying barriers that staff encountered to following fall prevention processes).
- Planning the agenda for and facilitating team meetings.
The Unit Champions were given regularly-scheduled paid time to work on these quality improvement activities (12 hours/month each). Through this process, the organization reinforced the use of a standardized approach that incorporates best practices in support of fall prevention.
Expanding the Unit Champion’s role to include planning, education, and data collection benefited the team in many ways. The Unit Champion is a professional who understands the culture of the hospital and the specific patient care units and has the professional expertise to understand policies and procedures and quality improvement. The Unit Champion serves as the expert on the ground who helps determine and carry out evidence-based best practices for fall prevention.
What You Can Do:
- Review job duties and expectations; the in-person training session may be a good point to begin this discussion. Survey staff to ensure that they understand their responsibilities related to fall prevention. Work with all staff to ensure that the fall prevention activities are adequately covered.
Module 2: How To Manage Change
Hospital: >50–200 beds
Pilot Units: Medical
Challenge: Process analysis assessment.
Solution: Map the steps of fall prevention processes, and analyze problematic areas.
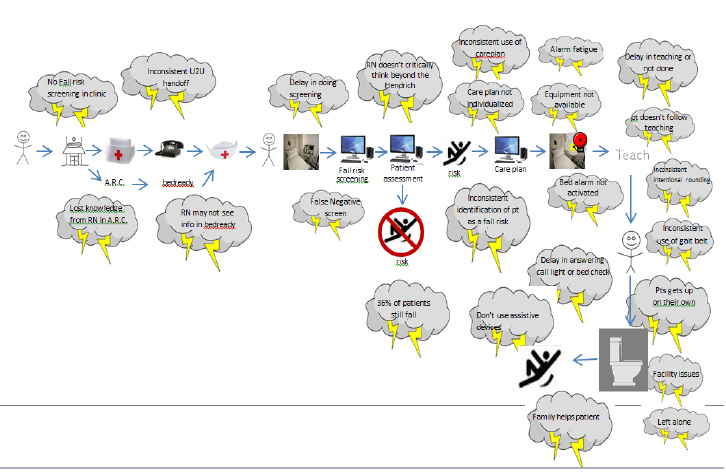
Description: The Fall Prevention Team used a LEAN QI transformation approach to problem solving to help uncover the opportunities to strengthen their fall prevention efforts. They developed a process map showing a high-level view of the steps in their fall prevention processes (e.g., arrival of the patient in the clinic, transfer to a hospital bed, fall risk screening, patient assessment, care planning, patient teaching, support of patient mobility in the hospital).
The team identified where breakdowns, workarounds, duplication, or variation occurred at each step and indicated those using “storm clouds” (see Figure F-1 below). Then the team prioritized which steps and problems in the process to work on.
What You Can Do:
- As suggested in the pretraining phase, use Tool 2C: Current Process Analysis from AHRQ’s Fall Prevention Toolkit to map your current fall prevention processes and evaluate areas of opportunity within your processes. Address these problems using quality improvement methods, such as PDSA and Lean QI methods.
Figure F-1. Illustration of Process Problems Using Storm Clouds
Module 3: Best Practices in Fall Prevention
Hospital: >400 beds
Pilot Units: Ortho/Trauma, Medical/Telemetry
Challenge: Conducting risk/post-fall assessments.
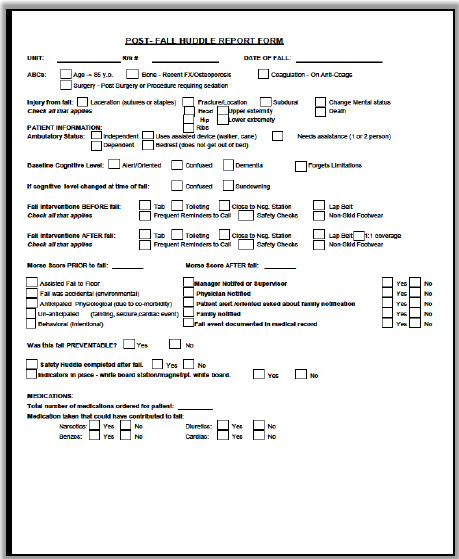
Solution: Hardwire the post-fall assessment process in an ongoing system.
Description: The Fall Prevention Team redesigned their post-fall assessment form based on AHRQ Toolkit Tool 3O: Postfall Assessment for Root Cause Analysis. This standard form (see Figure F-2 below) is key to maintaining the patient’s safety and to organizational learning about how to prevent future falls.
After noticing low compliance with the paper form, the team embedded the form in their safety event reporting system, where completion is mandatory. This change has helped hospital staff track and trend falls. The nurse manager reviews the information and communicates findings during safety huddles.
What You Can Do:
- Use a standardized approach to post-fall evaluation.
- Link risk management with post-fall huddles, in an effort to prevent future falls in this patient and in other patients.
Embed the post-fall assessment form in the event reporting system for seamless tracking and trending.
Figure F-2. Post-Fall Huddle Report Form
Module 3: Best Practices in Fall Prevention
Hospital: ≤50 beds
Pilot Unit: Acute Rehab
Challenge: Adequately monitoring patients at high risk of falling.
Solution: Institute video monitoring.
Description: The Implementation Team contributed to policy development, training for nurses and therapists, and monitoring of falls that occurred under video monitoring. Video monitoring equipment was purchased, including four stationary units and 15 mobile units. The team developed inclusion/exclusion criteria to assist in determining which patients may benefit from the use of video monitoring, as shown in Table F-1 below.
Table F-1. Video Monitoring Inclusion and Exclusion Criteria
| Inclusion Criteria | Exclusion Criteria |
|---|---|
|
|
The video monitoring system can speak to the patient using preprogrammed phrases available in different languages. Preprogrammed phases include “Wait for your nurse” and “Stop! Don’t get up.” The monitor tech can also use the monitoring system to talk to the patient directly, individualizing intervention messages as appropriate. (Usage reports indicate that individualized intervention messages are used more frequently than the preprogramed responses.) A runner is available for emergencies. If needed, the runner can push an alarm to alert nearby staff.
Education included special training for monitor techs and runners. Frontline clinicians received training on using the video monitor, using the alarm, communicating through the monitors, and indicating when privacy was needed or the patient was out of the room (e.g., for therapy). Basic education was provided for all clinicians. A monitoring room was set up with large viewing monitors. Documentation forms were created for video monitoring staff to track behaviors, trends, interventions, and need for ongoing video monitoring.
Video monitoring has helped reduce falls and falls with injury. It also supplements one-on-one monitoring, which has increased the hospital’s capacity to accept patients who are at high risk of falling.
What You Can Do:
- Various processes can be implemented to help ensure that falls are prevented; consider technology-related innovations as appropriate.
Module 3: Best Practices in Fall Prevention
Hospital: >400 beds
Pilot Units: Med/Surg, Telemetry
Challenge: Ensuring staff conduct rounds as intended.
Solution: Script purposeful rounding.
Description: The hospital found that most hospitalwide falls happen when patients go to the bathroom. The Fall Prevention Team created a more bathroom-driven rounding schedule. During the daytime and evening shifts, staff ask patients every 2 hours if they need to use the bathroom. During the night, staff wake patients up twice to ask if they need to use the bathroom, but they honor patient preferences.
A script was developed in collaboration with the Director of Service Excellence, and education on scripting was provided for all shifts. To implement this program, hospital staff held planning meetings. The Core Team met weekly, the Fall Reduction Team met biweekly, and the unit met monthly. The hospital provided housewide education and specific education for patient care technicians (PCTs). It also conducted biweekly audits.
The Fall Prevention Team created scripts to help staff talk to patients about toileting (see Figure F-3 below). The scripts explain the rounding schedule and ask patients about their nighttime bathroom routine. They state that the hospital’s goal is patient safety and urge patients to ask whenever they need help getting to the bathroom.
Staff meetings were held to educate staff on the scripting. Nurses and PCTs were encouraged to make the scripting their own so their words would flow more naturally. Scripting was rolled out to evening and night shifts, since most falls occurred during those times.
The rounding schedule requires nurses to round on odd hours and techs to round on even hours. The nighttime routine includes communication with each high-risk patient ahead of time to determine their usual toilet schedule and rounding request if they are awake and alert. If they are not awake and alert, they will be rounded on at the usual hours of midnight, 3 a.m., and 5 a.m.
The rounding focused on high fall risk patients. Meaningful rounding was implemented using the Henry Ford model to include modified scripting and rounding on a clock heavily influenced by patient communication.
What You Can Do:
- Consider using a script to maximize effectiveness of purposeful rounding.
- Compile data on underlying reasons for patient falls in your facility.
- Use available resources to address the problem.
Figure F-3. Sample Rounding Script
|
Fall Prevention RN and PCT Memorable Rounding Scripting RNs will round on patients during odd hours, and PCTs will round on even hours. During the morning rounds, the RNs and PCTs will say: “Good morning. My name is ____, and I want to make sure we are fulfilling your needs. Our goal is to provide you with an excellent patient experience and prevent you from falling, so you will have a member of our team coming in every hour to assist your needs. During the daytime, we will come in at 8, 10, 12, 2, 4, and 6 [or 9, 11, 1, 3, and 5] to take you to the bathroom. If you need to change positions or go to the bathroom sooner, please press the red nurse button and ask for assistance. Do you need to go to the bathroom now?” During the afternoon rounds, the RNs and PCTs will say: “Good morning. My name is ____, and I want to make sure we are fulfilling your needs. Our goal is to provide you with an excellent patient experience and prevent you from falling, so you will have a member of our team coming in every hour to assist your needs. We will come in at 2, 4, 6, and 8 [or 1, 3, 5, and 7] to take you to the bathroom. If you need to change positions or go to the bathroom sooner, please press the red nurse button and ask for assistance. Do you need to go to the bathroom now?” During the evening medication pass, the RNs will say: “Hello, Mr./Mrs. ____. Around midnight and 5:00 a.m., we will be entering your room to take you to the bathroom. How often do you normally get up to go to the bathroom at home? We will honor your normal routine. Our goal is maintaining your safety throughout the night, and we do not want you to fall. Do you need to go to the bathroom now?” During the evening and early morning bathroom rounds, the RNs and PCTs will say: “Hello, Mr./Mrs. ____. I am sorry to wake you, but I need to get you up and assist you to the bathroom at this time.” After placing the patient back in bed, the RNs and PCTs will say: “Again, I am sorry to have woken you at this time, but our goal is to maintain your safety through the evening. Is there anything I can do for you at this time?” |
Module 3: Best Practices in Fall Prevention
Hospital: >400 beds
Pilot Units: Ortho/Trauma, Medical/Telemetry
Challenge: Improving care planning, standardizing care, and using shared decision making.
Solution: Link risk assessment factors to care planning and patient education.
Description: The Fall Prevention Team developed a tool (see Figure F-4) that links the findings from the fall risk assessment to the care plan and serves as an educational tool for the patient and family. The tool provides visual cues for individualized fall prevention awareness and encourages shared decision making with the patient and family.
The tool was piloted on both pilot units, was audited, and had good results. The team believes the tool may improve interrater reliability of fall risk. Staff are expected to use the tool with patients within their first 2 hours on shift. The team is working with their electronic medical record vendor to ensure purchase of needed modules to incorporate clinical practice guidelines and enhance shift handoff communication.
Figure F-4. Individualized Fall Education Plan
Based on Fall Risk Assessment
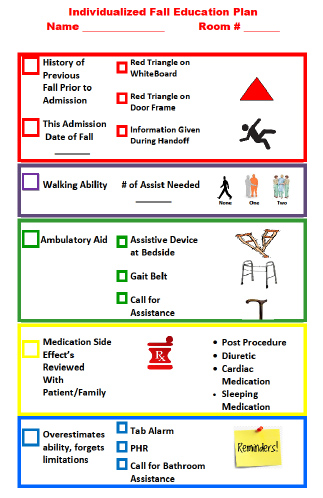
What You Can Do:
- Ensure that once risk assessment has identified patient risk factors, care planning matches the identified risks.
- Make sure that patients and their families understand the patient’s fall risk and how the proposed care plan addresses these risks.
- Identify specific aspects of the care plan that patients and families can help to implement.
Module 3: Best Practices in Fall Prevention
Hospital: >400 beds
Pilot Units: Rehab, Medical, Cardiac IMC
Challenge: Improving care planning and standardizing care.
Solution: Enhance EHR documentation.
Description: IT changed EHR documentation from a check box system to a free text system. While more time consuming, the new system improved nurses’ use of critical thinking when assessing fall risk and individualizing care plans. Clinical directors on the units now perform twice-daily chart audits and provide staff education in real time as issues are found. This procedure has improved accountability and sustainability.
What You Can Do:
- Consider including a representative from IT on your interdisciplinary team, or establish a point of contact who can support the team on an ad hoc basis.
- Determine whether your facility’s EHR can be modified.
- Determine the best ways to integrate risk assessment with care planning.
Module 3: Best Practices in Fall Prevention
Hospital: >400 beds
Pilot Units: Med/Surg, Telemetry
Challenge: Improving care planning and standardizing care
Solution: Use the facility’s EHR features for maximum productivity.
Description: The Fall Prevention Team worked with their EHR vendor to reeducate staff specifically on features in the system that should be used to link the care plan to the risk assessment.
What You Can Do:
- Consider including a representative from IT on your interdisciplinary team, or establish a point of contact who can support the team on an ad hoc basis.
- Determine the most efficient ways to use your facility’s EHR.
- Determine the best ways to integrate risk assessment with care planning.
Module 3: Best Practices in Fall Prevention
Hospital: >50–200 beds
Pilot Units: Med/Surg
Challenge: Lack of time for staff to do hourly rounding.
Solution: Use dedicated CNAs for purposeful hourly rounding.
Description: Dedicated CNAs conduct purposeful hourly rounding. One CNA does all the rounding on day shifts, and another CNA does all the rounding on evening shifts. Staff and patients like this practice, and it has improved the hospital’s patient experience survey scores. Patients report feeling that staff are in the room to help them more often.
For some nonurgent needs, patients decide to wait until the rounder comes back to help them. Staff report that this approach lessens noise on the unit, reduces call light usage, and prevents some staff interruptions.
What You Can Do:
- Consider ways to make purposeful hourly rounding more efficient, including by dedicating staff to this task.
- Share the purposeful hourly scheduling information with patients and their families to lessen the number of nonurgent calls between rounds.
Module 3: Best Practices in Fall Prevention
Hospital: >400 beds
Pilot Units: Medical, Acute Rehab
Challenge: Post-fall huddles were not implemented in a timely manner.
Solution: Standardize the post-fall huddle, and include all relevant staff.
Description: The hospital uses a hospitalwide paging system to announce post-fall huddles using a specific code and noting the specific unit where the fall occurred. When the code is announced, a standard tool to capture information, including risk assessment, universal fall precautions, environment, and outcomes, is used to guide the post fall huddle discussion.
Staff who participate in the discussion include the assigned nurse, CNA, nursing supervisor, charge nurse, manager or director for the department, and any staff who witnessed the fall. In addition, the Director of Risk Management and Patient Safety and the Risk Management Coordinator participate as available.
What You Can Do:
- Consider standardizing the post-fall process hospitalwide so that all staff understand the process after a fall has occurred.
- Consider ways to ensure that all staff needed for a post-fall huddle are informed of the fall and can get to the unit in a timely manner to complete the huddle.
Module 3: Best Practices in Fall Prevention
Hospital: >400 beds
Pilot Units: Medical, Acute Rehab
Challenge: Staff communication about fall risk.
Solution: Enhance communication about fall risk during shift handoffs and huddles.
Description: To facilitate exchange of pertinent information among certified nursing assistants (CNAs) at shift change, CNAs round together on patients before shift change. Rounding includes discussion of information on toileting, mobility, and implementation of fall precautions and interventions. This purposeful rounding occurs in the patient’s room or wherever the patient is (i.e., not in the break room) and includes the patient. In both pilot units, the team enhanced handoff communication between nurses at shift change to include discussion of fall risk.
In addition, the team implemented daily shift huddles addressing safety issues. During shift huddles, patients at risk of falling are discussed. This discussion includes patient-specific risk factors and interventions. For example, the following information is shared:
- Patients with impulsivity who get up without calling for assistance, so a bed or chair alarm is required.
- Patients at risk for falling because of issues with new medications, elimination, activity level, or transfer assistance needs.
- Patients who have gotten up from their bed or wheelchair unsupervised.
- Patients with a change in condition.
Also during shift huddles, staff members are reminded to complete the hourly rounding sheet for patients identified at high risk of falling.
What You Can Do:
- Communicate patient risk factors orally during shift handoffs and shift huddles, including any change in fall risk factors during the shift.
- Review medical record documentation and patient care worksheets.
- Include the patient in handoff communications when possible.
Module 3: Best Practices in Fall Prevention
Hospital: >50–200 beds
Pilot Units: Medical
Challenge: Maintaining Unit Team’s situational awareness of patients at highest risk for falls.
Solution: Use shift huddles to identify the three patients most at risk to fall on each shift.
Description: The Fall Prevention Team identified an opportunity to heighten collective and individual awareness of patients on the unit who were at the highest risk to fall. Many of the patients are considered high risk based on risk assessment results. However, the team sought to identify and focus on those most at risk. They examined the shift huddle process and determined that the huddle could be used to enhance communication about fall risk.
The team revised the huddle to include information on patients who had fallen, the interventions that were in place to prevent another fall, and the three patients most at risk to fall. Leaders monitored this process across shifts to assess compliance, benefits, and challenges.
Nursing staff and charge nurses appreciate the predictability of the message and knowing what to expect. They report having a heightened sense of awareness about the three patients at highest risk to fall. If they see a call light or hear an alarm for those patients, they know that it may be an opportunity to prevent that patient from falling.
What You Can Do:
- Communicate about high-risk fall patients during shift change to increase awareness of those needing additional preventive care.
Module 4: How To Implement the Fall Prevention Program in Your Organization
Hospital: >400 beds
Pilot Units: Med/Surg, Telemetry
Challenge: Staff engagement.
Solution: Recognize staff efforts.
Description: The Fall Prevention Team held a breakfast for the PCTs to reinforce the importance of purposeful rounding and teamwork. They also planned a party to celebrate the PCTs and their role in the Fall Prevention Program.
What You Can Do:
- Recognize the important role of bedside staff in fall prevention efforts.
- Explore opportunities to generate and maintain excitement about the change process.
Module 4: How To Implement the Fall Prevention Program in Your Organization
Hospital: >400 beds
Pilot Units: Ortho/Trauma, Medical/Telemetry
Challenge: Staff education.
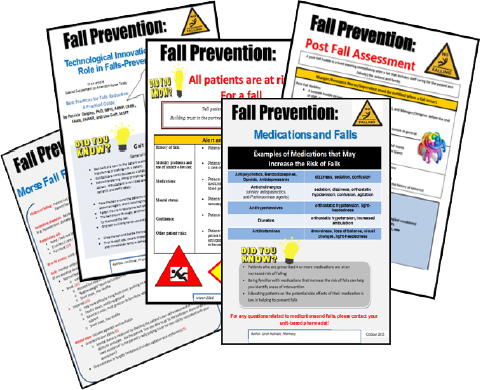
Solution: Develop and post monthly educational fall prevention pieces.
Description: The Fall Prevention Team developed a monthly fall prevention staff education program. Each discipline takes a turn making an educational flier (see Figure F-5). The flier is then posted on all floors and discussed during safety huddles.
What You Can Do:
- Include all disciplines in developing fall prevention staff education.
Figure F-5. Fall Prevention Educational Fliers
Module 4: How To Implement the Fall Prevention Program in Your Organization
Hospital: >400 beds
Pilot Units: Med/Surg, Telemetry
Challenge: Staff education.
Solution: Recognize and educate bedside staff.
Description: The Fall Prevention Team realized that success with the Fall Prevention Program required engagement of the PCTs. The team developed an educational program and planned a new 10-week PCT University. The program includes scripting for rounding, competency assessment, and auditing.
What You Can Do:
- Invest time and resources in educating frontline staff.
- Consider the unique needs of clinical and nonclinical staff.
- Educate all hospital staff, from top leadership to housekeeping staff.
Module 4: How To Implement the Fall Prevention Program in Your Organization
Hospital: >50–200 beds
Pilot Units: Medical
Challenge: Staff critical thinking skills.
Solution: Provide just-in-time coaching.
Description: The Implementation Team supports staff’s critical thinking by providing just-in-time coaching. For example, unit leaders observe PCTs’ bedside handoffs. They found that some PCTs believed it was rude to have conversations in front of patients. Leaders talked to and coached staff about the purpose of bedside handoffs and how to perform them in a respectful and helpful manner that includes the patient. Leaders reinforced this practice during staff meetings and staffing huddles. Leaders continue to talk with staff about the benefits of bedside handoffs (reducing patient falls) and to provide personal coaching to support staff member growth.
What You Can Do:
- Use in-person coaching to improve staff’s handoff skills and critical thinking.
- Educate staff on the importance and benefits of including the patient in handoffs.
Module 4: How To Implement the Fall Prevention Program in Your Organization
Hospital: >400 beds
Pilot Units: ICU, Med/Surg
Challenge: Staff turnover.
Solution: Institute a 1-year RN residency program.
Description: The hospital instituted a 1-year residency program for new graduate nurses in an effort to retain them. The goal is to provide specific orientation and on-the-job training to empower new nurses to learn and be confident in their skills. The program consists of:
- Three-month orientation.
- Three-week orientation to hospital.
- Nine-week preceptorship with floor nurses to build skills.
- Monthly forums to talk about their work and provide an emotionally supportive atmosphere.
- Graduation ceremony.
- Pay raise upon graduation.
The program improved retention of new graduate nurses. Its 2-year retention rate was 85 to 95 percent. Each class has 30 nurses.
What You Can Do:
- Determine how your facility can best retain and incorporate new nurses into its Fall Prevention Program and other patient safety efforts.
- Explore implementation of a residency program to support retention.
Module 4: How To Implement the Fall Prevention Program in Your Organization
Hospital: >200–400 beds
Pilot Units: Telemetry, Geri/Psych
Challenge: Staff turnover.
Solution: Develop a new graduate education program.
Description: The hospital had many staffing vacancies in nurse and CNA positions. It also experienced occasional shortages when CNAs were reassigned as sitters in the ER. In addition, the hospital had a high turnover rate for nurses who came in as new graduates and, after some training and experience, left for nearby academic hospitals. In response, the hospital developed an 8- to 10-week educational program for new graduates.
What You Can Do:
- Determine how your facility can best retain and incorporate new nurses into its Fall Prevention Program and other patient safety efforts.
- Consider reviewing your organization’s onboarding process, identifying and acting on opportunities for improvement.
Module 5: How To Measure Fall Rates and Fall Prevention Practices
Hospital: >50–200 beds
Pilot Units: Med/Surg, Geri/Psych
Challenge: Monitoring your Fall Prevention Program.
Solution: Collect process and outcome data.
Description: The Fall Prevention Team conducted audits of evidence-based practices. They measured the quality of the rounding and audited use of the 5 Ps. Team members conducted observational audits and 10 random chart review audits per week on the pilot unit. They also audited intentional rounding on several units and monitored all fall data.
What You Can Do:
- Monitor process and outcome measures to determine what processes can be improved to decrease fall rates.
Module 5: How To Measure Fall Rates and Fall Prevention Practices
Hospital: >400 beds
Pilot Units: Medical, Acute Rehab
Challenge: Reluctance to count assisted falls as falls.
Solution: Collect data on all falls, but also monitor assisted falls as a subset.
Description: Some staff were reluctant to consider and count assisted falls as falls—particularly on rehab units where patients were being appropriately encouraged and tested to increase mobility. Leaders continued to support counting and reporting assisted falls to be transparent and consistent with National Database of Nursing Quality Indicators definitions but also began tracking the number of assisted falls for quality improvement and measurement purposes.
What You Can Do:
- Encourage staff to collect data on all falls.
- Consider collecting data on all types of falls (e.g., assisted falls, falls without injury, falls with injury).
Module 5: How To Measure Fall Rates and Fall Prevention Practices
Hospital: >200–400 beds
Pilot Units: Telemetry, Geri/Psych
Challenge: Involving other disciplines in fall prevention.
Solution: Use data to drive quality improvement.
Description: At the request of hospital leadership, the Fall Implementation Team prepared a deep dive report encompassing 3 months of falls on the Med/Surg, Telemetry, and Behavioral Health Units (total of 50 falls). Forty percent of the falls occurred with staff in attendance, which may have prevented falls with injury.
Further evaluation found that with assisted falls, the staff in attendance were mainly Transport Team members. The Fall Prevention Team met with the Transport Team supervisor to discuss this finding. Together, they agreed to have transport staff attend nursing general orientation and nursing care orientation to educate transport staff on prevention strategies. The culture of this hospital is to look at its data when even the smallest trend is seen and use data to drive change and obtain buy-in from stakeholders.
What You Can Do:
- Use process data to explain when, where, and how falls are occurring.
- Educate all relevant disciplines.
Module 5: How To Measure Fall Rates and Fall Prevention Practices
Hospital: >50–200 beds
Pilot Units: Med/Surg, Geri/Psych
Challenge: Lack of national benchmarks.
Solution: Compare fall prevention performance with previous fall rates.
Description: The hospital benchmarked against its earlier fall rate data, using unit-level data that goes back 3 years. It looks at data for all falls, as well as for falls with injury. The data show a drop in falls with major injury from six falls in fiscal year 2014 to four in fiscal year 2015 to one in fiscal year 2016. The data also reveal a reduction in fall rates for both the entire hospital system and for the pilot units.
What You Can Do:
- Focus on improvement over time within hospital units and the hospital overall, rather than focusing on your hospital’s performance compared with an external benchmark.



