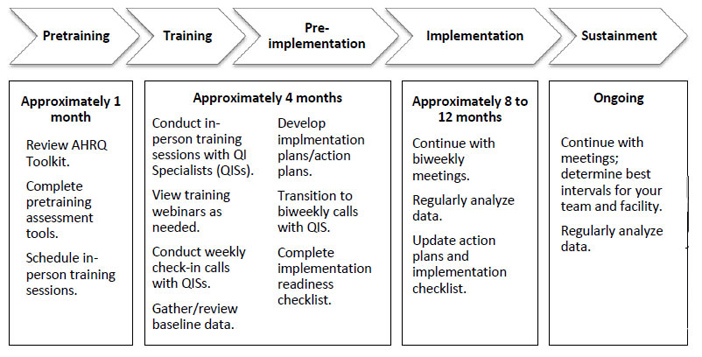
Now your hospital is ready to launch AHRQ’s Fall Prevention Program. The program has five phases. Each phase is listed below with approximate timeframes for each:
- Pretraining Phase (lasts approximately 1–2 months).
- Training Phase (lasts approximately 1–5 weeks).
- Preimplementation Phase (lasts approximately 1-4 months).
- Implementation Phase (lasts approximately 8–12 months).
- Sustainment Phase (ongoing).
Pretraining Phase
The Pretraining Phase lasts approximately 1–2 months. The purpose of this phase is to prepare your hospital for a successful Training Phase.
Develop a Project Charter
It’s a good idea to develop a project charter. This document helps your hospital clearly define the goals, scope, timing, milestones, team roles, and responsibilities for its Fall Prevention Program. In most cases, the Leadership Team develops the project charter and gives it to the Implementation Team.
A sample project charter template (PDF) is available. Table 3 provides some guidelines for project charters.
Table 3. Project Charter Guidelines
| Do | Don’t |
|---|---|
| Give the Implementation Team guidance about what they are being asked to accomplish. | Tell the team specifically how to complete the work. |
| Make the project charter clear and concise, focusing on key elements of requested work. | Include many pages of information. |
| Keep the project charter in a location where it is available to all involved in the project so it can serve as a reference and reminder to avoid scope creep as the project progresses. | File the project charter away in a notebook or in some folder on the Team Lead’s computer. |
| Identify a consistent format for all organizational project charters to make it easier for staff to use. | Make the project charter complicated. |
| Include which leadership and other committees will receive reports from your team and how often they will receive these reports. | |
| Provide guidance about the team’s decision-making authority. When appropriate, delineate the roles of those involved in making decisions about changes to be tested or made. Consider using a RACI chart (roles and responsibilities matrix) (Appendix A).
|
Be unclear about the team’s decision-making authority. |
| Needlessly limit the team’s ability to plan and conduct innovative small tests of change with formal approval processes. |
Identify Key Program Personnel
Before your hospital embarks on the Training Phase, it’s important to identify key Fall Prevention Program personnel. These may include the Implementation Team, Implementation Leaders, and QISs (or other instructors).
|
Note: During the AHRQ pilot initiative (see AHRQ’s Fall Prevention Program above), two QISs with expertise in QI and patient safety were assigned to each hospital. The QISs delivered the in-person training, assisted the hospital Implementation Team throughout the program, and provided as-needed technical assistance. They also served as liaisons between participating hospitals and national fall prevention experts. However, there are a variety of ways to implement AHRQ’s Fall Prevention Program. It is recommended that your hospital use QISs and make the Implementation Team accountable to them. This accountability was a critical factor in the success of the pilot initiative. Determine what responsibilities (if any) QISs will have in your hospital’s Fall Prevention Program. If you do opt to use QISs, decide whether they will be internal staff members or consultants brought in from outside. If you opt not to use QISs, decide who will lead the in-person training. Also decide who the Implementation Team will be accountable to and what resources will be available to the Implementation Team for any needed ongoing technical assistance. |
Identify the Implementation Team Leaders. The Leadership Team that developed the charter (or other appropriate group within your facility) should determine who will lead the Implementation Team. Make sure the Implementation Team Leaders have expertise in training, mentoring, leading QI programs, managing projects, managing change, and facilitating meetings. Ensure the Implementation Team Leaders have support from an executive leader who will closely track the needs and progress of the team, address barriers, and provide resources as needed.
Identify the QISs/Instructors.i Select the QISs or other instructors (e.g., Education Department personnel, Implementation Team Leaders, or other staff members) who will deliver the 6-hour in-person training (see Training Curriculum above) and provide ongoing technical assistance to the Implementation Team. These individuals will work to adopt and adapt the fall prevention action plan to fit the unit or hospital.
Choose the QISs/instructors with care. They should:
- Have QI training and experience.
- Be advocates of teamwork.
- Be dynamic presenters with a desire and talent to teach.
- Have strong oral communication skills.
- Hold positions that allow flexible scheduling.
- Be highly visible, accessible, and available for coaching throughout the change effort.
Fall prevention success cannot be achieved through classroom training alone. As in any change effort, the introduction of a quality improvement initiative requires champions in everyday practice to reinforce, monitor, and role-model fall prevention and QI principles.
Prepare for the In-Person Training
To ensure a successful in-person training, hospital leadership, the Implementation Leader, QISs, and instructors should prepare for it.
Hospital Leadership’s Responsibilities. Hospital leadership should prepare for the in-person training as follows:
- Provide participant handouts (e.g., hard copies of the participant agenda; participant slides; tools; and hospital processes, policies, and procedures).
- Send invitations to participants.
- Assign a person to take notes on the in-person training, including opportunities for improvement participants identify. (If there are two QISs/instructors, the one who is not presenting may fill this role.)
In addition, hospital leadership should provide the following for the in-person training:
- A room large enough to accommodate all participants.
- Needed audiovisual equipment, including a laptop computer, LCD projector, and screen.
- One or two flip charts with stands.
- Lunch for participants (or instructions to bring a bag lunch).
- Coffee/tea/water for morning and afternoon breaks.
Implementation Team Leader’s Responsibilities. The Implementation Team Leader, with input from other relevant staff, should prepare for the Training Phase as follows:
- Complete the following pretraining toolsii:
- Obtain the following hospital policies and procedures (to be shared during the in-person training):
- Universal fall precautions.
- Fall prevention care plan.
- Submit the completed pre-training tools, along with the hospital policies and procedures, to the QISs/instructors at least 2 weeks before the in-person training.
- Be prepared to discuss the policies and procedures and the completed tools during the in-person training.
Quality Improvement Specialists’/Instructors’ Responsibilities. The QISs/instructors should prepare for the Training Phase as follows:
- Review, understand, and be completely familiar with AHRQ’s Fall Prevention Toolkit.
- Review the training modules (see Table 1):
- Follow the guidelines for preparing for the in-person training. These are found at the beginning of each Instructor Training Guide.
- Customize the participant slides. Add your hospital’s name on the first slide. Insert images of the completed pre-training tools into the appropriate places within the slides (see Production Agenda to assist in determining where to include these tools).
- Watch the supplementary training webinars (see Table 1 and Appendix C).
- Review the pretraining tools and policies and procedures submitted by the Implementation Team Leader (see above). Identify gaps and opportunities for improvement to discuss during the in-person training.
- Develop a production agenda (see an example from AHRQ’s pilot initiative in Appendix D). This is a detailed timeline for the in-person training.
- Develop a participant agenda (see an example from AHRQ’s pilot initiative in Appendix E). This is a less-detailed version of the production agenda.
- Invite/ask a senior-level hospital administrator to provide a welcome and discuss the urgency for your hospital’s Fall Prevention Program.
- Schedule the in-person training:
- The Implementation Team Leader should work with the QISs/instructors to schedule the 6-hour in-person training (see Training Curriculum above). Determine which staff members should participate and to what extent. Members of the Implementation Team and tentative unit champions will likely attend the entire training. Others, such as Information Technology (IT) and Education Department staff, may need to attend only the parts of the training directly relevant to their jobs.
- To prevent disruptions and scheduling problems and to maximize learning, excuse participants from all other duties during the in-person training.
During the AHRQ pilot initiative (see AHRQ’s Fall Prevention Program above), the in-person training took place in a single 1-day session. However, there are many alternatives to a 1-day training. Below are two examples:
- Deliver the five modules in two separate sessions:
- Session 1—Module 1: Understanding Why Change Is Needed, Module 2: How To Manage Change, and Module 3: Best Practices in Fall Prevention
- Session 2—Module 4: How To Implement the Fall Prevention Program in Your Organization and Module 5: How To Measure Fall Rates and Fall Prevention Practices
- Deliver one module per week for 5 consecutive weeks.
Stay in Touch
The Implementation Team and QISs/instructors should hold weekly check-in calls or meetings throughout the Pretraining Phase.
Training Phase
The Training Phase lasts approximately 1–5 weeks. During the Training Phase, the QISs/instructors will deliver the in-person training. In addition, it is strongly recommended that participants of the in-person training view the training webinars during this phase (see Training Curriculum above).
Prepare for the Training Phase
To ensure a successful Training Phase, hospital leadership, the Implementation Leader, and the QISs/instructors should prepare for the Training Phase (see Pretraining Phase above).
Complete a Draft Action Plan
One objective of the in-person training is to complete Tool 2F: Action Plan. This draft can be fine tuned by a core group from the Implementation Team over the following week or so and shared with the team for approval. The action plan is a living document that may change over time as it is implemented and tested.
Tool 2F includes the following key interventions to be identified and prioritized:
- Analyze the current state of fall prevention practices in this organization.
- Identify the set of prevention practices to be used in the redesigned system.
- Assign roles and responsibilities for implementing the redesigned fall prevention practices.
- Put the redesigned care processes into practice.
- Monitor fall rates and practices.
- Sustain the redesigned prevention practices.
Stay in Touch
The Implementation Team and QISs/instructors should continue to hold weekly check-in calls or meetings during the Training Phase.
Preimplementation Phase
The Preimplementation Phase lasts approximately 1–4 months. The purpose of the Preimplementation Phase is to prepare your hospital for a successful Implementation Phase.
Identify Opportunities for Improvement
The Implementation Team should start by identifying opportunities for improvement. (It may have identified some opportunities during the in-person training.) The team should follow your organization’s methodology or model for making improvements (e.g., Lean methodology, Model for Improvement).
Prioritize Opportunities for Improvement
Next, the Implementation Team should decide which of these opportunities for improvement to focus on. Try not to tackle everything at once. The team should focus on just a few key interventions.
To keep your prevention initiative moving forward, the Implementation Team should meet weekly during the 2 weeks after the in-person training for focused discussions on prioritizing opportunities for quality improvement. Appendix B tells how to prioritize these opportunities.
Refine the Action Plan
Once the Implementation Team has identified and prioritized opportunities for improvement, it can refine the draft action plan it created during the Training Phase. The goal is to develop an action plan within 2 weeks after the in-person training. The team may want to use Tool 2F or an alternate version of the action plan to address the following items:
- How to develop unit teams and how they will work with the Implementation Team.
- Roles and responsibilities of each staff member and unit champions.
- Standards of care and practices to be met.
- Which fall prevention practices go beyond a single unit and how they will be addressed.
- How gaps in staff education and competency will be addressed.
- Plans for rolling out new standards and practices and how they will be integrated into ongoing work processes.
- Who is accountable for measuring and monitoring implementation.
- How changes in performance will be assessed (both process and outcome measures).
- How the effort will be sustained.
Collect Baseline Data
The Implementation Team should gather and review baseline fall data. To learn more about measurement, see the supplementary Training webinar Measuring Fall and Fall-Related Injury Rates and Prevention Practices and the Learning Network webinars Creating Control Charts To Interpret Fall Data and Measurement: Using Data To Tell a Story.
Complete the Preimplementation Checklist
Before moving on to the Implementation Phase, the Implementation Team may want to use the checklist in Table 4, which was developed for the AHRQ pilot initiative (see AHRQ’s Fall Prevention Program above), to confirm that it has completed all the Preimplementation Phase activities.
Table 4. Preimplementation Checklist
| Tasks | Completion Date |
|---|---|
| Initial Post-Training Priorities | |
| Identify pilot units | |
| Establish various teams | |
| Multidisciplinary | |
| Pilot unit managers on Implementation Team | |
| Conduct process mapping | |
| Use fall knowledge assessment | |
| Create action plan outline | |
| Continue to watch webinars | |
| Primary Preimplementation Priorities | |
| Draft action plan | |
| Prioritize list of improvement opportunities | |
| Conduct resource needs assessment | |
| Select improvement practices | |
| Determine goals for improvement | |
| Develop aim statement | |
| Develop staff education/assessment plan | |
| Create plans to roll out new standards/practices | |
| Assign staff person to monitor implementation | |
| Determine how to measure performance | |
| Determine data collection process | |
| Collect/assess process measure data | |
| Collect/assess outcome measure data | |
| Create sustainment plan | |
| Final Preimplementation Priorities | |
| Finalize implementation action plan | |
| Secure team buy-in | |
Stay in Touch
The Implementation Team and QISs/instructors should continue to hold check-in calls or meetings. If prudent, they can decrease their meetings to every other week during the Preimplementation Phase.
Implementation Phase
The Implementation Phase lasts approximately 8–12 months. During the Implementation Phase, the Implementation Team will implement the interventions that it prioritized in the action plan.
View Webinars
Team members should view any relevant supplementary Learning Network webinars (see Table 1 and Appendix C).
Pilot Interventions
The Implementation Team will pilot the interventions as follows:
- Choose one or two pilot units.
- Train staff on new procedures.
- Collect process and outcome measures and feedback on new procedures.
- Communicate results.
Refine practices to address any problems.
- Start to identify which practices can be spread to other hospital units or departments.
- Assign all staff roles and responsibilities to prevent falls.
- Assign specific individuals or groups to each duty identified.
- Identify any existing fall prevention experts your facility has access to, and provide staff education in collaboration with these experts.
- Determine paths of ongoing communication and reporting for fall prevention processes.
- Build fall prevention practices into ongoing work processes.
- Collect and analyze data to learn about fall rates, fall-related injuries, and causes of falls.
- Measure fall prevention practices.
- Meet regularly to assess progress.
- Create a plan to implement targeted practices to other areas in the hospital.
Complete the Implementation Checklist
The Implementation Team may want to complete the checklist in Table 5 and review it with the QISs/instructors. The checklist helps assess the progress of the Team’s QI efforts. It’s a good idea to revisit the checklist every 2 months during the Implementation Phase.
Table 5. Managing Change During Implementation
| Yes | No | Comments/ Description | |
|---|---|---|---|
| Implementation Team | |||
| Are Team Leaders and Implementation Team in place? | |||
| Does team meet biweekly to review and discuss progress? | Who attends? | ||
| Do Team Leaders/key staff participate in regular conference calls with QISs/instructors? | Who attends? | ||
| Does Unit Implementation Team meet regularly to review/discuss progress? | How often? | ||
| Senior leadership – Senior Admin Leader on Team? Does he/she visibly promote, support, and resource the project? |
|||
| Project manager – Does he/she have adequate support to manage the project? | |||
| Specific goals set? | List goals. | ||
| Action Plan | |||
| Updated at least every 2 months? | |||
| Challenges to implementing the action plan prevention practices identified at organization and unit levels? | |||
| Strategies for building new practices into daily routine are in place? | |||
| Processes/Support in Place To Facilitate Action Plan | |||
| Communication – Do you have a communication plan to keep staff and the Implementation Team up to date on rates/results and progress of prevention program? | Describe plan and progress: | ||
| Do you have a plan to communicate rates/ progress/ resource needs to senior leadership? | Describe plan and progress: | ||
| Do you have a plan to keep other stakeholders up to date? | Describe plan and progress: | ||
| Do you have a plan for soliciting positive and negative feedback about the prevention strategies from staff? | Describe feedback/what you do with feedback: | ||
| Do you have a plan for soliciting feedback from patients and families? | Describe feedback/what you do with feedback: | ||
| Do you document your efforts on this initiative for organizational history and learning? | |||
| Education – Did you provide staff education to support the changes being made? List topics/mechanisms used for education: | |||
| 1. | |||
| 2. | |||
| 3. | |||
| 4. | |||
| Education: Do you have a patient/family prevention education plan? | |||
| Monitoring | |||
| Is a problem-solving feedback loop in place with plans to redesign practices as needed? | |||
Cope With Challenges
Implementation of new processes can bring various challenges. The hospitals involved in the AHRQ pilot initiative experienced a variety of barriers and worked to overcome them. Appendix F (Hospital Practice Insights: Challenges and Solutions) provides some of the challenges they encountered and how they coped with these challenges.
Stay in Touch
The Implementation Team and QISs/instructors should continue to hold check-in calls or meetings every other week.
Sustainment Phase
The Sustainment Phase is ongoing. During the Sustainment Phase, your organization will work to make the interventions and improved outcomes normal, integrated, and mainstream—part of your hospital’s culture. This phase includes changing thoughts and attitudes as well as processes and outcomes. Sustaining an improvement means that the progress is locked in, and staff don’t revert to the old ways of doing things. To learn more about sustainment, see the supplementary Training webinar Sustaining Fall Prevention Practices at Your Hospital and the Learning Network webinar Sustainability.
Provide Leadership Support Throughout Your Fall Prevention Program
To sustain the interventions, hospital leadership must provide support from project inception through implementation and after. Hospital leadership must assess how the changes are affecting staff. Are staff making the changes as intended? If not, why not? What barriers are staff encountering, and how can management remove these barriers?
Communicate Clearly
Leaders and staff need to have a common vision of the change and how it will contribute to the overall goal. Make sure they understand what specific systems and processes will change (e.g., reminders or prompts in the EHR to conduct fall risk assessment within a certain time) and who will carry out these actions. Communication channels created or reinforced during the Fall Prevention Program should continue throughout the Sustainment Phase.
Track Performance
The Implementation Team should assess the extent to which organizational structures and routines have changes and if old behaviors are resurfacing. They should evaluate performance at both an intervention level and an outcome level at least quarterly. Senior-level staff should be responsible for sustaining gains and reviewing intervention-level performance monthly in a structured reporting format (e.g., an organizational scorecard).
To learn more about measurement, see the supplementary training webinar Measuring Fall and Fall-Related Injury Rates and Prevention Practices and the Learning Network webinars Creating Control Charts To Interpret Fall Data and Measurement: Using Data To Tell a Story.
Celebrate Progress
The Implementation Team should reinforce desired behaviors. Appendix F (Hospital Practice Insights: Challenges & Solutions) suggests ways to celebrate progress.
Plan for Sustainment
At the end of the Implementation Phase, the Implementation Team should identify what is needed to sustain fall prevention efforts, including organizational support (e.g., new staff training, existing staff refreshers, IT support for reporting performance data). It should also decide who will be responsible for sustaining ongoing fall prevention efforts. In planning for sustainment, your Implementation Team may find it helpful to discuss the questions in Table 6, which were developed for the AHRQ pilot initiative (see AHRQ’s Fall Prevention Program above), with their QISs/instructors.
Table 6. Plan for Sustainment
| Discussion Question | Answer |
|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Stay in Touch
The Implementation Team and QISs/instructors should continue to hold check-in calls or meetings for 6 to 12 months after implementation. In addition, the Implementation Team should keep meeting regularly.
Figure 1 shows the phases and activities of the AHRQ pilot initiative (see AHRQ’s Fall Prevention Program above). It illustrates how a QI program might be organized.
Figure 1. Timeline of Fall Prevention Program Activities
i. Some content in this section was adapted from TeamSTEPPS 2.0 Course Management Guide, retrieved July18, 2017, from https://www.ahrq.gov/teamstepps/instructor/essentials/coursemgmt.html.
ii. Be sure to begin these assessments several weeks before the in-person training to allow enough time to complete them thoroughly.



