Debrief Example - Implementation Guide
Slide 1: Debrief Example
Quality Improvement Study
<name> Ambulatory Surgery Center
<insert date>
Slide 2: Problem Statement
- The surgical safety checklist has been shown to reduce surgical mortality and complication rates in a variety of surgical settings.
- A critical component of the checklist is the completion of a debrief after each case.
- The debrief provides an opportunity to address—
- Equipment problems.
- Key concerns for patient recovery and management.
- Ideas for making the next case safer and/or more efficient.
- When any elements of the debrief are omitted, teams miss opportunities to discuss continuous quality improvement, resulting in negative safety implications for patients.
Slide 3: Improvement Team
- Project Leader(s)
– <insert name> - Team Members
– <insert name> - Administrator/Manager
– <insert name> - Anesthesiologist/Certified Registered Nurse Anesthetist
– <insert name> - Circulating Nurse
– <insert name> - Scrub Technician
– <insert name> - Surgeon
– <insert name> - Data collector
– <insert name> - Anesthesia Technician
– <insert name> - Pre-op/Post-Anesthesia Care Unit Nurse (PACU)
– <insert name> - Physician Assistant
– <insert name> - Infection Preventionist
Slide 4: Data Description
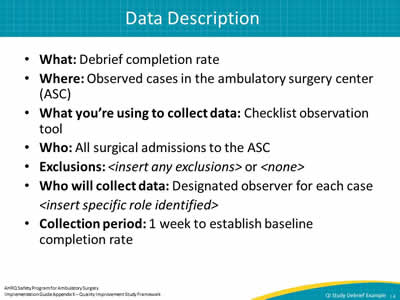
- What: Debrief completion rate.
- Where: Observed cases in the ambulatory surgery center (ASC).
- What you’re using to collect data: Checklist observation tool.
- Who: All surgical admissions to the ASC.
- Exclusions: <insert any exclusions> or <none>
- Who will collect data: Designated observer for each case
<insert specific role identified> - Collection period: 1 week to establish baseline completion rate.
Slide 5: Data Collection
- Baseline data collection period: 3/2/2015 – 3/6/2015
- Number of cases observed: 23
- Data collected
- Tally sheet of debriefs completed.
- Observation log data.
Slide 6: Data Collection
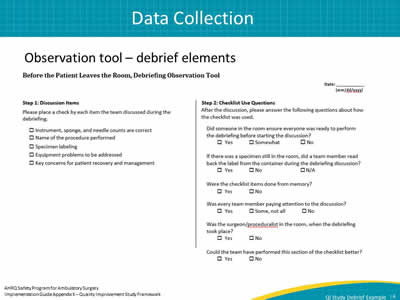
Observation tool – debrief elements
Image: portion of debriefing observation tool.
Slide 7: Baseline Data
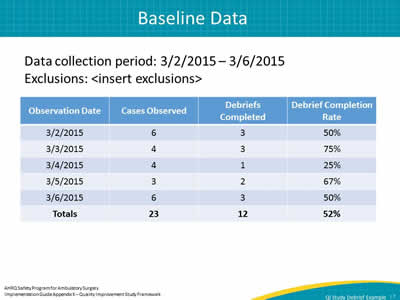
Data collection period: 3/2/2015 – 3/6/2015
Exclusions: <insert exclusions>
| Observation Date | Cases Observed | Debriefs Completed |
Debrief Completion Rate |
|---|---|---|---|
| 3/2/2015 | 6 | 3 | 50% |
| 3/3/20153 | 4 | 3 | 75% |
| 3/4/2015 | 4 | 1 | 25% |
| 3/5/2015 | 3 | 2 | 67% |
| 3/6/2015 | 6 | 3 | 50% |
| Totals | 23 | 12 | 52% |
Slide 8: The Goal
To achieve a 100% completion rate for all elements of the debrief for all surgical cases by June 1, 2015.
Slide 9: Data Comparison
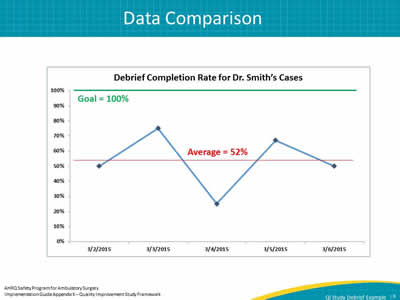
Image: example chart of debrief completion rate.
Slide 10: Data Comparison
Image: handwritten graphs used for data comparison
Slide 11: Data Comparison

Debrief completion rate goal: 100%
Observed debrief completion rate: 52%
Current performance: Below goal by 48%
Slide 12: Cause of the Problem
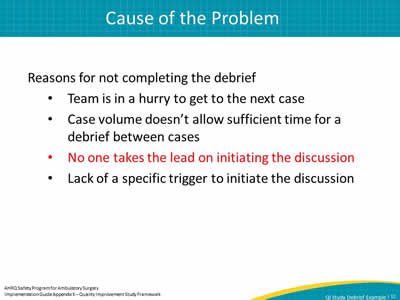
Reasons for not completing the debrief
- Team is in a hurry to get to the next case.
- Case volume doesn’t allow sufficient time for a debrief between cases.
- No one takes the lead on initiating the discussion.
- Lack of a specific trigger to initiate the discussion.
Slide 13: Corrective Actions/Interventions
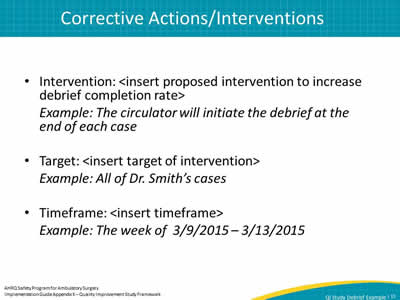
- Intervention: <insert proposed intervention to increase debrief completion rate>
Example: The circulator will initiate the debrief at the end of each case - Target: <insert target of intervention>
Example: All of Dr. Smith’s cases - Timeframe: <insert timeframe>
Example: The week of 3/9/2015 – 3/13/2015
Slide 14: Materials Developed (optional)
Slide 15: Change Data
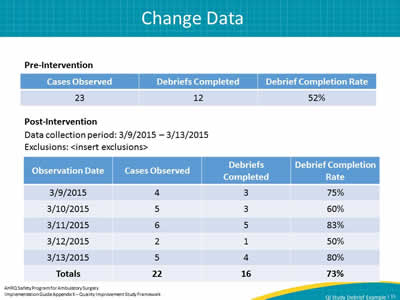
Pre-Intervention
| Cases Observed | Debriefs Completed | Debrief Completion Rate |
|---|---|---|
| 23 | 12 | 52% |
Post-Intervention
Data collection period: 3/9/2015 – 3/13/2015
Exclusions: <insert exclusions>
| Observation Date | Cases Observed |
Debriefs Completed |
Debrief Completion Rate |
|---|---|---|---|
| 3/9/2015 | 4 | 3 | 75% |
| 3/10/2015 | 5 | 3 | 60% |
| 3/11/2015 | 6 | 5 | 83% |
| 3/12/2015 | 2 | 1 | 50% |
| 3/13/2015 | 5 | 4 | 80% |
| Totals | 22 | 16 | 73% |
Slide 16: Data Comparison
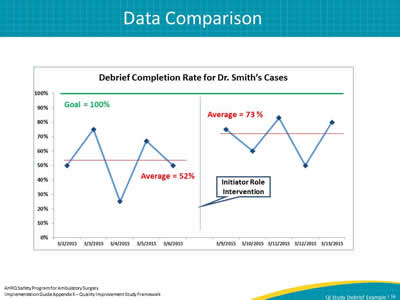
Image: example chart of debrief completion rate.
Slide 17: Data Comparison
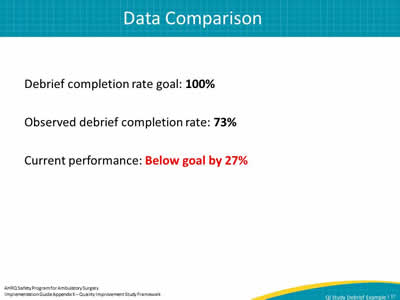
Debrief completion rate goal: 100%
Observed debrief completion rate: 73%
Current performance: Below goal by 27%
Slide 18: Additional Corrective Actions or Remeasurements
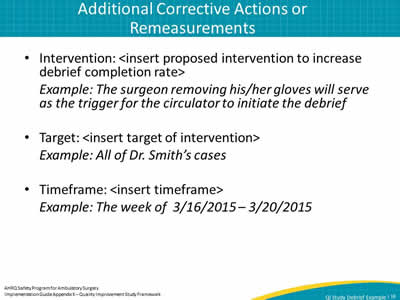
- Intervention: <insert proposed intervention to increase debrief completion rate>
Example: The surgeon removing his/her gloves will serve as the trigger for the circulator to initiate the debrief - Target: <insert target of intervention>
Example: All of Dr. Smith’s cases - Timeframe: <insert timeframe>
Example: The week of 3/16/2015 – 3/20/2015
Slide 19: Materials Developed (optional)
Slide 20: Remeasurement
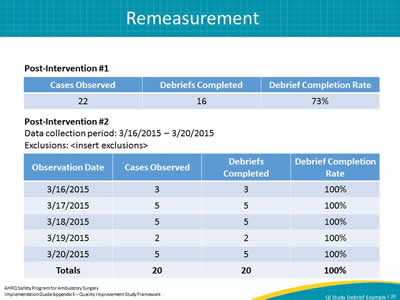
Pre-Intervention # 1
| Cases Observed | Debriefs Completed | Debrief Completion Rate |
|---|---|---|
| 22 | 16 | 73% |
Post-Intervention # 2
Data collection period: 3/16/2015 – 3/20/2015
Exclusions: <insert exclusions>
| Observation Date | Cases Observed |
Debriefs Completed |
Debrief Completion Rate |
|---|---|---|---|
| 3/16/2015 | 3 | 3 | 100% |
| 3/17/2015 | 5 | 5 | 100% |
| 3/18/2015 | 5 | 5 | 100% |
| 3/19/2015 | 2 | 2 | 100% |
| 3/20/2015 | 5 | 5 | 100% |
| Totals | 20 | 20 | 100% |
Slide 21: Data Comparison
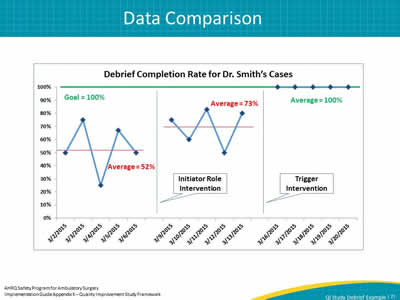
Image: Chart shows baseline data, data post initiator role intervention, and trigger intervention data.
Slide 22: Data Comparison
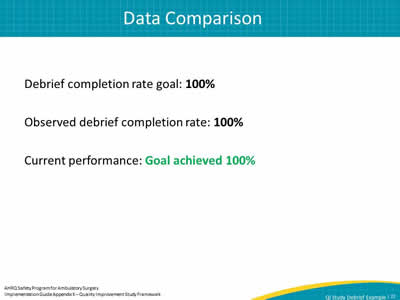
Debrief completion rate goal: 100%
Observed debrief completion rate: 100%
Current performance: Goal achieved 100%
Slide 23: Conclusions
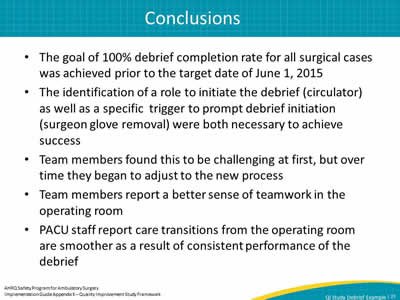
- The goal of 100% debrief completion rate for all surgical cases was achieved prior to the target date of June 1, 2015.
- The identification of a role to initiate the debrief (circulator) as well as a specific trigger to prompt debrief initiation (surgeon glove removal) were both necessary to achieve success.
- Team members found this to be challenging at first, but over time they began to adjust to the new process.
- Team members report a better sense of teamwork in the operating room.
- PACU staff report care transitions from the operating room are smoother as a result of consistent performance of the debrief.
Slide 24: Communication/Reporting of Findings
- The results of this study were shared with the board on XX/XX/2015
- <insert excerpt from board meeting minutes>
Slide 25: Sustaining the Gains
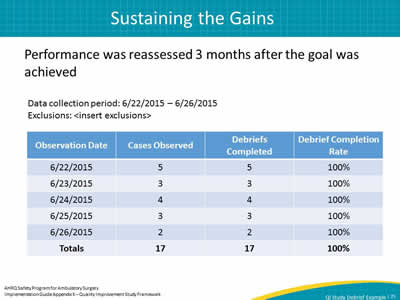
Performance was reassessed 3 months after the goal was achieved
Data collection period: 6/22/2015 – 6/26/2015
Exclusions: <insert exclusions>
| Observation Date | Cases Observed |
Debriefs Completed |
Debrief Completion Rate |
|---|---|---|---|
| 6/22/2015 | 5 | 5 | 100% |
| 6/23/2015 | 3 | 3 | 100% |
| 6/24/2015 | 4 | 4 | 100% |
| 6/25/2015 | 3 | 3 | 100% |
| 6/26/2015 | 2 | 2 | 100% |
| Totals | 17 | 17 | 100% |
Slide 26: Sustaining the Gains
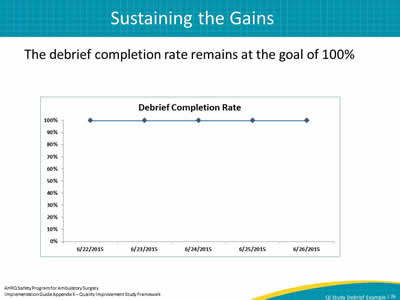
The debrief completion rate remains at the goal of 100%
Image: chart illustrating the debrief completion rate remaning at the goal of 100%
Slide 27: Future Work
- Completion rates for other elements of the surgical safety checklist will be explored
- Completion of preop briefing.
- Completion of the timeout
- Completion of surgeon sharing any changes to operative plan and possible difficulties.
- Completion of team introductions.
- Completion of surgeon's statement regarding concerns before starting the procedure.
- Consistent use of each component on the checklist will help improve the safety culture in our center.



