Sustainability Module
Slide 1: Sustainability Module
Sustainability Module
Slide 2: Learning Objectives
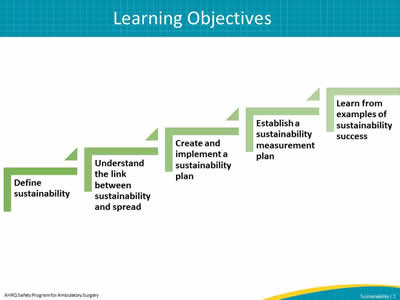
Image: Define sustainability.
Understand the link between sustainability and spread.
Create and implement a sustainability plan.
Establish a sustainability measurement plan.
Learn from examples of sustainability success.
Slide 3: Overview
- Defining sustainability and its importance in quality improvement.
- Linking sustainability and spread.
- Discussing barriers and solutions to sustainability.
- Developing and implementing a sustainability plan.
- Creating a sustainability measurement plan.
- Learning from examples of sustainabilty in different health care facilities.
Slide 4: Definition of Sustainability
- Ensuring gains are maintained beyond the life of the project1, or the institutionalization or routinization of programs into ongoing organizational systems
Slide 5: Importance of Sustainable Change in Continuous Improvement
- Assist with variability in health care.
- Provide continuous high-quality care and reliable safe practices.
- Prevent project fatigue.
- Control processes.
- Monitor progress.
- Engage senior leaders.
- Establish improvement culture and engaged staff.
- Create cultural legacy.
Slide 6: Sustainable Change After Project End?
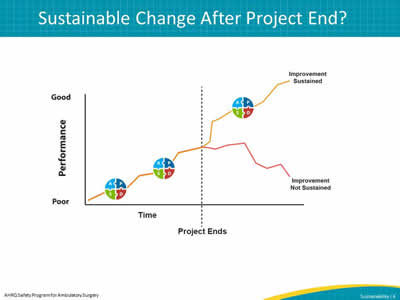
Image: Line graph showing that sustainability is about the change after a project ends. If improvement is not sustained, performance can return to the original rate or potentially worse. If improvement is sustained, performance can even surpass the improvements made during the project. It is this potential that makes sustainability so important. The graph has a line showing steadily improving performance, but then when the project ends, the line diverges into two separate lines -- one going up, reflecting continued improved performance when the improvement is sustained, and the other going down, reflecting decreasing performance when the improvement is not sustained.
Slide 7: What Does Sustainability Mean for Your Facility?
- How do you see other projects sustained in your facility?
- Are values, beliefs, and practices incorporated into the mission of your organization and/or are they incorporated into existing and routine care processes?
- What steps are taken to create a new norm?
Slide 8: Facilitators of Sustainable Change2

Image: Facilitators of sustainable change listed in ascending order on an iceberg:
Create sense of urgency.
Build the guiding team.
Develop a change vision and strategy.
Understanding and buy-in.
Empower others.
Short-term wins.
Image: TeamSTEPPS logo
As seen in TeamSTEPPS®
2Kotter J. Leading Change. Harvard Business School Press, Boston, MA, 1996, as cited in TeamSTEPPS Fundamentals Course: Module 8. Change Management: Instructor's Slides: TeamsTEPPS Fundamentals Course. November 2008. Agency for Healthcare Research and Quality, Rockville, MD.
Slide 9: Sustainability and Spread
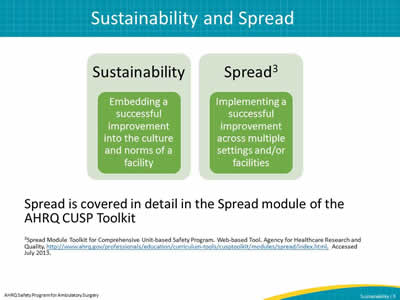
Image: Sustainability
Embedding a successful improvement into the culture and norms of a facility.
Spread
Implementing a successful improvement across multiple facilities.
Spread is covered in detail in the Spread module of the AHRQ CUSP Toolkit.
3Spread Module Toolkit for Comprehensive Unit-based Safety Program. Web-based Tool. Agency for Healthcare Research and Quality. Accessed July 2013.
Slide 10: Linking Sustainability and Spread
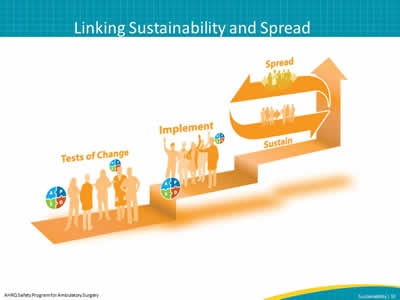
Image: The project lifecycle begins with tests of change followed by implementation. After implementation, changes can be sustained or spread to others. Often times spread and sustainability may occur concurrently. The figure illustrates this cycle by showing each point in the cycle as a step on a staircase.
Slide 11: Planning for Sustainability
- Plan early
– Engage senior leaders and administration early. - Identify barriers to sustainability.
- Discover potential solutions.
- Learn how to create a sustainability plan.
Slide 12: Planning Early
- Plan for resources
– Financial
– Staffing - Identify leaders and program champion(s).
- Educate staff.
- Plan for modification of goal(s)
– Identify what continued success looks like.
Image: four medical providers standing together
Slide 13: Potential Barriers to Sustainability
- Lack of organizational infrastructure and resources
- Staff turnover
- Organizational skepticism
- Individual resistance to change
Slide 14: Workable Solutions to Sustainability Barriers
- Lack of organizational infrastructure and resources
– Develop strategies and flexibility to account for resource fluctuation.
– Plan financial resources for maintaining improvements beyond the project end. - Staff turnover
– Embed newly developed processes into new staff orientation and organizational policies.
– Train staff continuously including train-the-trainer education.
– Develop volunteer network to assist in case of staffing fluctuations and/or shortage (funding, staff turnover).
Slide 15: Workable Solutions to Sustainability Barriers
- Managing skepticism1
– Present ongoing evidence that the new process is a better one.
– Show staff and stakeholders real data.
– Reserve staff time away from normal duties to work on proposed improvements.
– Encourage active senior leader engagement- Consider measuring how frequently senior leaders and administrators review sustainability data/outcomes as indicators of engagement.
Slide 16: Barrier: Individual Resistance to Change
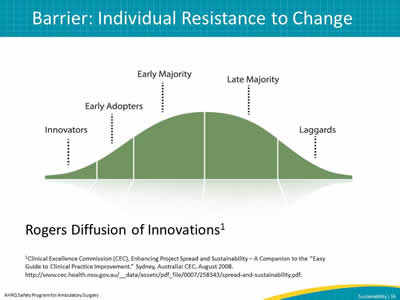
Image: Using Roger's Diffusion of Innovations to show individuals at different levels of adoption as the barrier of individual resistance to change.
Rogers Diffusion of Innovations1
Slide 17: Factors That Influence Individual Resistance or Adoption
- Perceived relative advantage1
- Fuzzy boundaries
- Compatibility
- Risk
- Complexity
- Task Issues
- Trialability
- Knowledge required to use it
- Observability
- Augmentation/support
- Reinvention
Slide 18: Steps to Creating and Implementing a Sustainability Plan
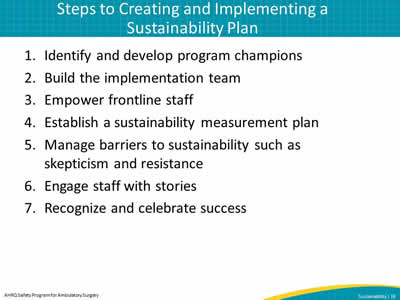
- Identify and develop program champions.
- Build the implementation team.
- Empower frontline staff.
- Establish a sustainability measurement plan.
- Manage barriers to sustainability such as skepticism and resistance.
- Engage staff with stories.
- Recognize and celebrate success.
Slide 19: 1. Identify and Develop Program Champion(s)
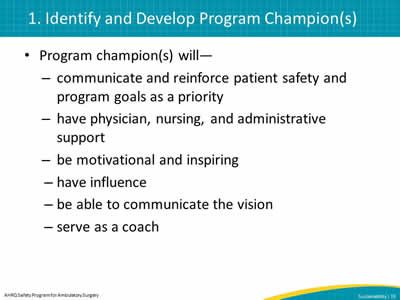
- Program champion(s) will—
– communicate and reinforce patient safety and program goals as a priority.
– have physician, nursing, and administrative support.
– be motivational and inspiring.
– have influence.
– be able to communicate the vision.
– serve as a coach.
Slide 20: 2. Build the Implementation Team
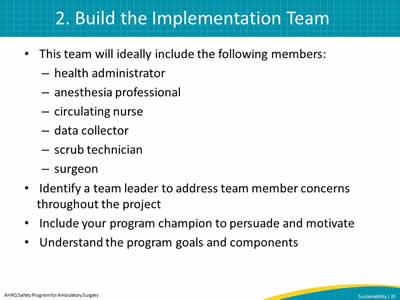
- This team will ideally include the following members:
– health administrator
– anesthesia professional
– circulating nurse
– data collector
– scrub technician
– surgeon - Identify a team leader to address team member concerns throughout the project.
- Include your program champion to persuade and motivate.
- Understand the program goals and components.
Slide 21: 3. Empower Frontline Staff
Frontline staff will—
- Feel comfortable bringing up patient safety concerns to other team members or team leaders.
- Speak up when a potential break in patient safety protocol may occur or actually occurs.
- Be commended, and not punished, for speaking up about patient safety.
Image: clip art of frontline staff member raising hand.
Image: TeamSTEPPS logo
As seen in TeamSTEPPS®
Slide 22: 4. Establish a Sustainability Measurement Plan
- Build systems for collecting process, outcome, and quality improvement activity data.
- Use data to continuously improve performance.
Slide 23: 5. Manage Skepticism and Resistance
Active involvement of the administrative and clinical champions including—
- Motivation by the project leaders for team members to try the program interventions.
- Staff experiencing positive outcomes from new ways of doing things.
- Dedicated time and resources to carry out the interventions.
Slide 24: 6. Engaging Staff With Stories
- Stories are a powerful way to engage staff in ways that numbers cannot.
- Encourage your team leaders to discuss actual patient stories to drive home important lessons.
Image: photo of audio on page
Select audio symbol to play audio, or access audio at:
https://www.ahrq.gov/hai/tools/ambulatory-surgery/sections/sustainability.html
Slide 25: 7. Recognizing and Celebrating Success
Images: health care team clip art and photo of audio on page
Select audio symbol to play audio, or access audio at:
https://www.ahrq.gov/hai/tools/ambulatory-surgery/sections/sustainability.html
Slide 26: Establishing a Sustainability Measurement Plan
- Assess readiness for sustainability.
- Build a measurement system
– Who, what, when, how to measure. - Establish robust followup and transparent feedback system.
Slide 27: Assess Readiness for Sustainability
- Act on a sustainability plan only after gains have been achieved
- Ask four key questions before carrying out the plan4:
- Is the intervention near the final stage of development? If there were room for further changes, would those alter the implementation?
- Has real, measurable improvement been demonstrated?
- Who cares about the improvement? Does the project represent the views of all involved?
- What policy or technological changes may make the project redundant? When might this happen?
Slide 28: Tools for Assessing Readiness for Sustainability1
- Sustainability Scoring Tool (CCE: Australia Guide).
- Change Achievement Success Indicator (CASI).
Image: clip art of open book
1Clinical Excellence Commission (CEC), Enhancing Project Spread and Sustainability – A Companion to the "Easy Guide to Clinical Practice Improvement." Sydney, Australia: CEC. August 2008. http://www.cec.health.nsw.gov.au/__data/assets/pdf_file/0007/258343/spread-and-sustainability.pdf.
Slide 29: Build a Measurement System
- Choose who, what, when, and how to measure
– WHO will measure- Example: Nurse/data coordinator tracks surgical site infection data monthly for reporting purposes
- Set the goals
– Example: To sustain a low rate of surgical site infections within unit/facility - Choose a Family of Measures framework
- Use process, outcome, and balancing measures
Image: clip art of low hanging fruit on tree
Slide 30: Family of Measures (FOM) Example5
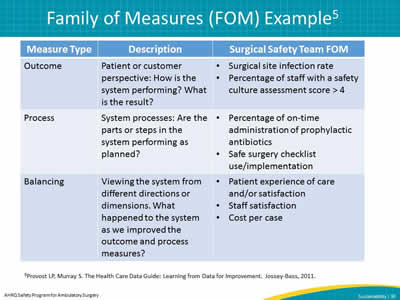
| Measure Type | Description | Surgical Safety Team FOM |
|---|---|---|
|
Outcome |
Patient or customer perspective: How is the system performing? What is the result? |
|
|
Process |
System processes: Are the parts or steps in the system performing as planned? |
|
|
Balancing |
Viewing the system from different directions or dimensions. What happened to the system as we improved the outcome and process measures? |
|
5Provost LP, Murray S. The Health Care Data Guide: Learning from Data for Improvement. Jossey-Bass, 2011.
Slide 31: When To Measure
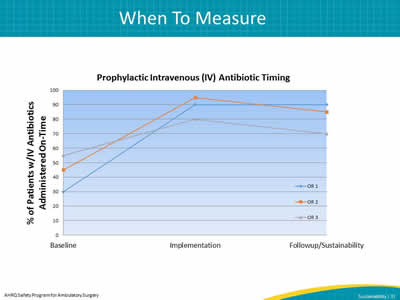
Image: run chart example to show prophylactic IV antibiotic timing and when to measure.
Slide 32: How To Measure
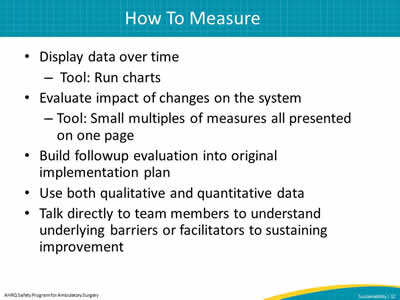
- Display data over time
– Tool: Run charts - Evaluate impact of changes on the system
– Tool: Small multiples of measures all presented on one page - Build followup evaluation into original implementation plan
- Use both qualitative and quantitative data
- Talk directly to team members to understand underlying barriers or facilitators to sustaining improvement
Slide 33: How To Measure: Run Charts5
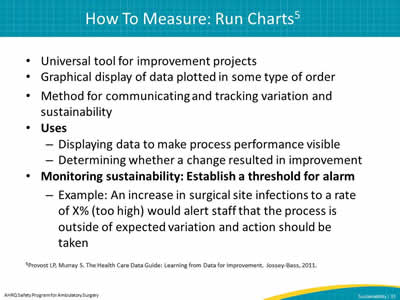
- Universal tool for improvement projects.
- Graphical display of data plotted in some type of order.
- Method for communicating and tracking variation and sustainability.
- Uses
– Displaying data to make process performance visible.
– Determining whether a change resulted in improvement. - Monitoring sustainability: Establish a threshold for alarm
– Example: An increase in surgical site infections to a rate of X% (too high) would alert staff that the process is outside of expected variation and action should be taken.
5Provost LP, Murray S. The Health Care Data Guide: Learning from Data for Improvement. Jossey-Bass, 2011.
Slide 34: How To Measure: Run Chart Example
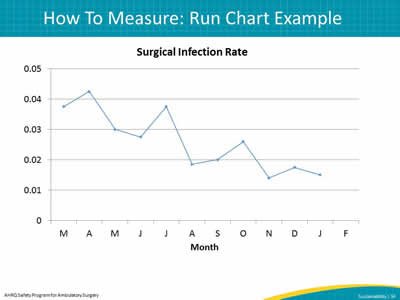
Image: run chart to show an example of tracking surgical infection rates.
Slide 35: How To Measure: Small Multiples Example
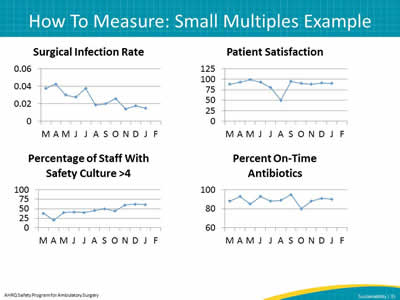
Images: surgical infection rate example.
patient satisfaction run chart example.
percentage of staff with safety culture >4 example.
percent on-time antibiotics run chart example.
Slide 36: Establish Followup and Feedback System
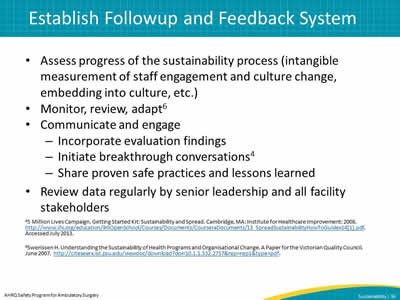
- Assess progress of the sustainability process (intangible measurement of staff engagement and culture change, embedding into culture, etc.)
- Monitor, review, adapt6
- Communicate and engage
– Incorporate evaluation findings
– Initiate breakthrough conversations4
– Share proven safe practices and lessons learned - Review data regularly by senior leadership and all facility stakeholders
Slide 37: Sustainability Examples: Organizational Structure
- The Community Health Network in Indiana uses central line insertion kits that contain all the tools and checklists to comply with their improvement process’s central line bundle elements.4
- Many hospitals merge multiple workflows to streamline daily practice (i.e., medication reconciliation forms that double as admission order forms).
Slide 38: Sustainability Examples: Data
- Baptist Memorial Health Care created a measurement system including4—
– An appointed facilitator.
– A process for collecting, reporting, and inputting data into system database.
– Generation of graphics to show performance trends.
– Communication to senior leadership and medical staff.
– Refining of the improvement plan based on data. - Minnesota Children’s Hospitals and Clinics uses a screen saver slide show on all hospital computer terminals to display up-to-date intervention results.
Slide 39: Sustainability Examples: Capacity Building
- The Advocate Health System in Chicago participates in capacity building by providing education around quality improvement, process improvement, and measurement techniques in regular staff seminars.4
Slide 40: Summary
- Sustainability helps organizations embed processes into their organizational culture
- Organizations need to be prepared to address barriers that can affect sustainability
- An effective sustainability plan includes—
– Planning early in the improvement process.
– Easy to reach goals.
– Program champion.
– Fit within organizational mission.
– Ongoing evaluation and transparency of measures.
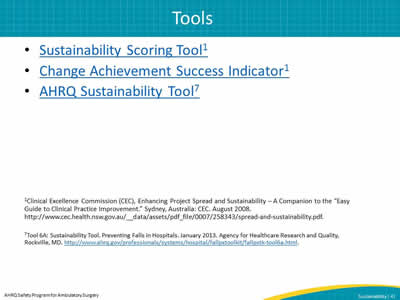
Slide 41: Tools
Slide 42: References
- Clinical Excellence Commission (CEC), Enhancing Project Spread and Sustainability – A Companion to the "Easy Guide to Clinical Practice Improvement." Sydney, Australia: CEC. August 2008. http://www.cec.health.nsw.gov.au/__data/assets/pdf_file/0007/258343/spread-and-sustainability.pdf.
- Kotter J. Leading Change. Harvard Business School Press, Boston, MA, 1996, as cited in TeamSTEPPS Fundamentals Course: Module 8. Change Management: Instructor's Slides: TeamsTEPPS Fundamentals Course. November 2008. Agency for Healthcare Research and Quality, Rockville, MD.
- Spread Module Toolkit for Comprehensive Unit-based Safety Program. Web-based Tool. Agency for Healthcare Research and Quality. Accessed July 2013.
- 5 Million Lives Campaign. Getting Started Kit: Sustainability and Spread. Cambridge, MA: Institute for Healthcare Improvement; 2008. Accessed July 2013.
- Provost LP, Murray S. The Health Care Data Guide: Learning from Data for Improvement. Jossey-Bass, 2011.
- Swerissen H. Understanding the Sustainability of Health Programs and Organisational Change. A Paper for the Victorian Quality Council. June 2007.
- Tool 6A: Sustainability Tool. Preventing Falls in Hospitals. January 2013. Agency for Healthcare Research and Quality, Rockville, MD.



