Evidence Behind Pain, Agitation, and Delirium: Assessments and Sedation Management: Slide Presentation
AHRQ Safety Program for Mechanically Ventilated Patients
Slide 1: AHRQ Safety Program for Mechanically Ventilated Patients
Evidence Behind Pain, Agitation, and Delirium: Assessments and Sedation Management
Slide 2: Learning Objectives
After this session, you will be able to—
- Identify the objectives and benefits of using the ABCDEF bundle.
- Understand evidence supporting the use of the Society of Critical Care Medicine’s (SCCM) guidelines for the management of Pain, Agitation, and Delirium (PAD).
- Improve the care of mechanically ventilated patients in the intensive care unit (ICU) through delirium assessments and sedation management.
Slide 3: Pain, Agitation, and Delirium1
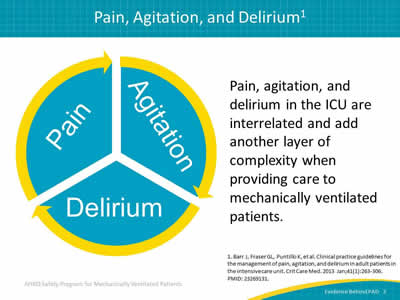
Image: Circle divided into three parts to illustrate the relationship between pain, agitation, and delirium.
Pain, agitation, and delirium in the ICU are interrelated and add another layer of complexity when providing care to mechanically ventilated patients.
1. Barr J, Fraser GL, Puntillo K, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med 2013 Jan;41(1):263-306. PMID: 23269131.
Slide 4: Pain, Agitation, and Delirium1
Image: Pain fragment of cycle.
- The International Association for the Study of Pain defines pain as an "unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage."
- The negative consequences of unrelieved pain in ICU patients are significant and long lasting.
- Many critically ill patients may be unable to self-report pain due to the use of mechanical ventilation or high doses of sedative agents or neuromuscular blocking agents.
1. Barr J, Fraser GL, Puntillo K, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med 2013 Jan;41(1):263-306. PMID: 23269131.
Slide 5: Pain, Agitation, and Delirium1
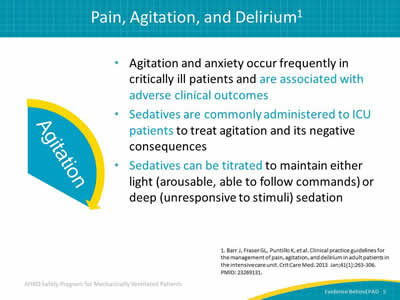
Image: Agitation fragment of cycle.
- Agitation and anxiety occur frequently in critically ill patients and are associated with adverse clinical outcomes.
- Sedatives are commonly administered to ICU patients to treat agitation and its negative consequences.
- Sedatives can be titrated to maintain either light (arousable, able to follow commands) or deep (unresponsive to stimuli) sedation.
1. Barr J, Fraser GL, Puntillo K, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med 2013 Jan;41(1):263-306. PMID: 23269131.
Slide 6: Pain, Agitation, and Delirium1
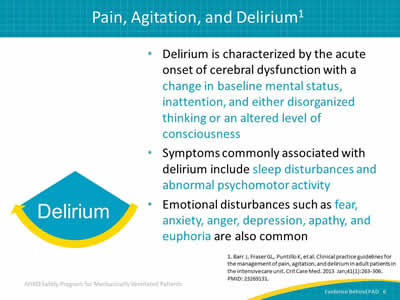
Image: Delirium fragment of cycle.
- Delirium is characterized by the acute onset of cerebral dysfunction with a change in baseline mental status, inattention, and either disorganized thinking or an altered level of consciousness.
- Symptoms commonly associated with delirium include sleep disturbances and abnormal psychomotor activity.
- Emotional disturbances such as fear, anxiety, anger, depression, apathy, and euphoria are also common.
1. Barr J, Fraser GL, Puntillo K, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med 2013 Jan;41(1):263-306. PMID: 23269131.
Slide 7: ABCDEF Bundle Checklist2
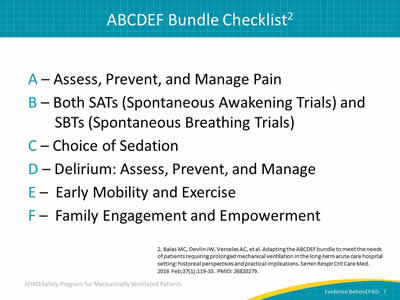
A – Assess, Prevent, and Manage Pain
B – Both SATs (Spontaneous Awakening Trials) and SBTs (Spontaneous Breathing Trials)
C – Choice of Sedation
D – Delirium: Assess, Prevent, and Manage
E – Early Mobility and Exercise
F – Family Engagement and Empowerment
2. Balas MC, Devlin JW, Verceles AC, et al. Adapting the ABCDEF bundle to meet the needs of patients requiring prolonged mechanical ventilation in the long-term acute care hospital setting: historical perspectives and practical implications. Semin Respir Crit Care Med 2016 Feb;37(1):119-35. PMID: 26820279.
Slide 8: ABCDEF Bundle Objectives3-6
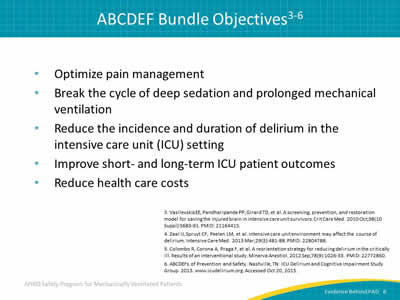
- Optimize pain management.
- Break the cycle of deep sedation and prolonged mechanical ventilation.
- Reduce the incidence and duration of delirium in the intensive care unit (ICU) setting.
- Improve short- and long-term ICU patient outcomes.
- Reduce health care costs.
3. Vasilevskis EE, Pandharipande PP, Girard TD, et al. A screening, prevention, and restoration model for saving the injured brain in intensive care unit survivors. Crit Care Med 2010 Oct;38(10 Suppl):S683-91. PMID: 21164415.
4. Zaal IJ, Spruyt CF, Peelen LM, et al. Intensive care unit environment may affect the course of delirium. Intensive Care Med 2013 Mar;29(3):481-88. PMID: 22804788.
5. Colombo R, Corona A, Praga F, et al. A reorientation strategy for reducing delirium in the critically ill. Results of an interventional study. Minerva Anestiol 2012 Sep;78(9):1026-33. PMID: 22772860.
6. ABCDEFs of Prevention and Safety. Nashville, TN: ICU Delirium and Cognitive Impairment Study Group. 2013. www.icudelirium.org. Accessed Oct 20, 2015.
Slide 9: ABCDEF Implementation Success: Meta-Analysis7
Critical Care
A Systematic Review of Implementation Strategies for Assessment, Prevention, and Management of ICU Delirium and Their Effect on Clinical Outcomes
Trogrlić et al. 2015
Meta-analysis involved 21 studies, all including process measures and 9 with clinical outcomes data
7. Trogrlić Z, van der Jagt M, Bakker J, et al. A systematic review of implementation strategies for assessment, prevention, and management of ICU delirium and their effect on clinical outcomes. Crit Care 2015 Apr 9;19(1):157. PMID: 25888230.
Slide 10: ABCDEF Implementation Success: Meta-Analysis7
- A variety of programs improved process measures:
- e.g., 92% delirium screening adherence.
- Using more than six implementation strategies and integrating either PAD guidelines or ABCDE bundle:
- Statistically lower mortality and shorter ICU length of stay.
- Delirium "incidence" static; delirium duration may be better metric.
- Strategies targeting organizational changes in addition to provider behavior also associated with reduced mortality.
7. Trogrlić Z, van der Jagt M, Bakker J, et al. A systematic review of implementation strategies for assessment, prevention, and management of ICU delirium and their effect on clinical outcomes. Crit Care 2015 Apr 9;19(1):157. PMID: 25888230.
Slide 11: Keystone’s ABCDE Bundle Collaborative Results8
- 51 hospitals in Michigan’s Keystone ICU initiative.
- Those implementing combined SATs and delirium screening were 3.5 times as likely to exercise ventilated patients.
- Incomplete or nonsequential bundle implementation yielded lower success rates.
- Authors concluded that with regard to the ABCDE bundle, "[T]he whole truly is greater than the sum of its parts."
8. Miller MA, Govindan S, Watson SR, et al. ABCDE, but in that order? A cross-sectional survey of Michigan intensive care unit sedation, delirium, and early mobility practices. Ann Am Thorac Soc 2015 Jul;12(7):1066-71. PMID: 25970737.
Slide 12: 2013 Society of Critical Care Medicine PAD Guidelines1
Critical Care Medicine
Journal of the Society of Critical Care Medicine
Clinical Practice Guidelines for the Management of Pain, Agitation, and Delirium in Adult Patients in the Intensive Care Unit
Barr, et al. 2013.
1. Barr J, Fraser GL, Puntillo K, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med 2013 Jan;41(1):263-306. PMID: 23269131.
Slide 13: 2013 Society of Critical Care Medicine PAD Guidelines1
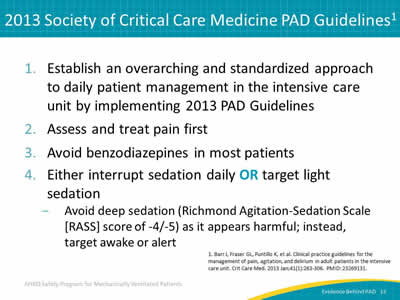
- Establish an overarching and standardized approach to daily patient management in the intensive care unit by implementing 2013 PAD Guidelines.
- Assess and treat pain first.
- Avoid benzodiazepines in most patients.
- Either interrupt sedation daily OR target light sedation:
- Avoid deep sedation (Richmond Agitation-Sedation Scale [RASS] score of -4/-5) as it appears harmful; instead, target awake or alert.
1. Barr J, Fraser GL, Puntillo K, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med 2013 Jan;41(1):263-306. PMID: 23269131.
Slide 14: 2013 Society of Critical Care Medicine PAD Guidelines1
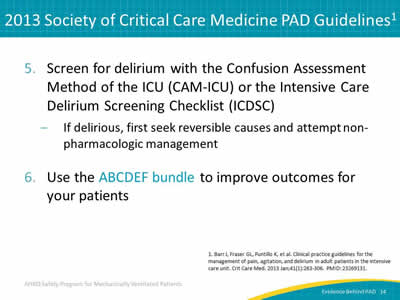
- Screen for delirium with the Confusion Assessment Method of the ICU (CAM-ICU) or the Intensive Care Delirium Screening Checklist (ICDSC):
- If delirious, first seek reversible causes and attempt non-pharmacologic management.
- Use the ABCDEF bundle to improve outcomes for your patients.
1. Barr J, Fraser GL, Puntillo K, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med 2013 Jan;41(1):263-306. PMID: 23269131.
Slide 15: SCCM: PAD Treatment of Delirium Recommendations1
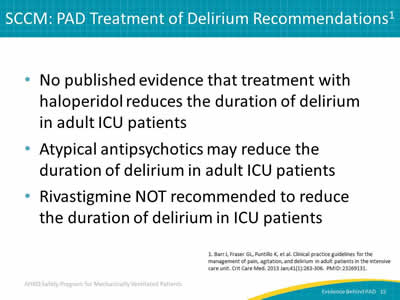
- No published evidence that treatment with haloperidol reduces the duration of delirium in adult ICU patients.
- Atypical antipsychotics may reduce the duration of delirium in adult ICU patients.
- Rivastigmine NOT recommended to reduce the duration of delirium in ICU patients.
1. Barr J, Fraser GL, Puntillo K, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med 2013 Jan;41(1):263-306. PMID: 23269131.
Slide 16: Delirium Screening in the ICU
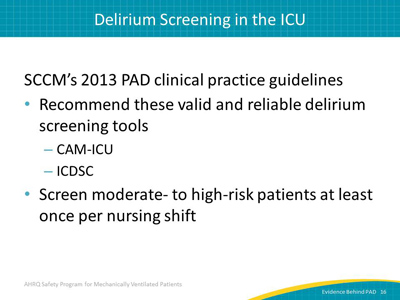
SCCM’s 2013 PAD clinical practice guidelines:
- Recommend these valid and reliable delirium screening tools:
- CAM-ICU.
- ICDSC.
- Screen moderate- to high-risk patients at least once per nursing shift.
Slide 17: Don’t Forget About Dr. Dre

Diseases
Sepsis, chronic obstructive pulmonary disease, congestive heart failure
Drug Removal
SATs and stopping benzodiazepines/narcotics
Environment
Immobilization, sleep and day/night, hearing aids, glasses, noise
Image: Photograph of Beats by Dre headphones and box.
Slide 18: Johns Hopkins Medicine Quality Improvement (QI) Project9

Reduced delirium via fewer benzodiazepines and more mobility
Image: Table of outcomes, pre-QI, post-QI, and p-values. The outcomes are days with any benzodiazepine use*, days alert (RASS -1 to +1), physical/occupational therapy (PT/OT) in medical ICU, Number of PT/OT treatments in ICU, days without delirium, days of delirium in ICU, and days of coma.
* Benzodiazepine dose (median midazolam mg) from 47 mg down to 15 mg/day.
9. Needham DM, Korupolu R, Zanni JM, et al. Early physical medicine and rehabilitation for patients with acute respiratory failure: a quality improvement project. Arch Phys Med Rehabil 2010 Apr;91(4):536-42. PMID: 20382284.
Slide 19: Wake Up and Breathe Program Results: Indiana University10
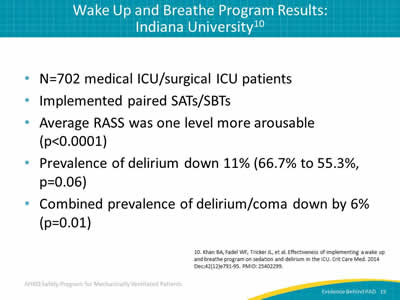
- N=702 medical ICU/surgical ICU patients.
- Implemented paired SATs/SBTs.
- Average RASS was one level more arousable (p<0.0001).
- Prevalence of delirium down 11% (66.7% to 55.3%, p=0.06).
- Combined prevalence of delirium/coma down by 6% (p=0.01).
10. Khan BA, Fadel WF, Tricker JL, et al. Effectiveness of implementing a wake up and breathe program on sedation and delirium in the ICU. Crit Care Med 2014 Dec;42(12)e791-95. PMID: 25402299.
Slide 20: Efficacy and Safety11
Critical Care Medicine
Journal of the Society of Critical Care Medicine
Effectiveness and Safety of the Awakening and Breathing Coordination, Delirium Monitoring/Management, and Early Exercise/Mobility Bundle
Balas et al. 2014
1.5-year prospective QI study conducted in 5 ICUs, 1 stepdown unit, and 1 oncology hematology special care unit within a tertiary care hospital.
11. Balas MC, Vasilevskis EE, Olsen KM, et al. Effectiveness and safety of the awakening and breathing coordination, delirium monitoring/management, and early exercise/mobility bundle. Crit Care Med 2014 May;42(5):1024-36. PMID: 24394627.
Slide 21: Efficacy and Safety: Ventilator-Free Days11
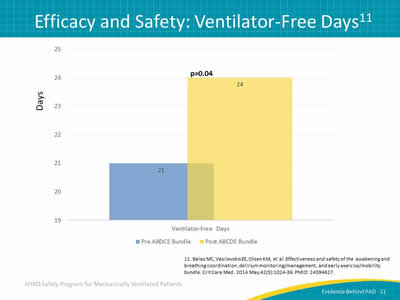
Image: Bar graph of ventilator-free days. Ventilator-free days increased from 21 to 24 after use of the ABCDE bundle.
11. Balas MC, Vasilevskis EE, Olsen KM, et al. Effectiveness and safety of the awakening and breathing coordination, delirium monitoring/management, and early exercise/mobility bundle. Crit Care Med 2014 May;42(5):1024-36. PMID: 24394627.
Slide 22: Efficacy and Safety: Delirium Results11
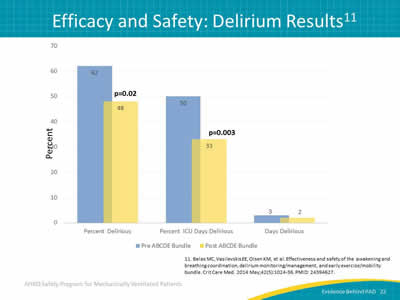
Image: Bar graph of delirium results. The following improvements were seen after use of the ABCDE bundle: percent delirious dropped from 62 to 48, percent ICU days delirious dropped from 50 to 33, and days delirious decreased from 3 to 2.
11. Balas MC, Vasilevskis EE, Olsen KM, et al. Effectiveness and safety of the awakening and breathing coordination, delirium monitoring/management, and early exercise/mobility bundle. Crit Care Med 2014 May;42(5):1024-36. PMID: 24394627.
Slide 23: Efficacy and Safety: Early Mobility Results11
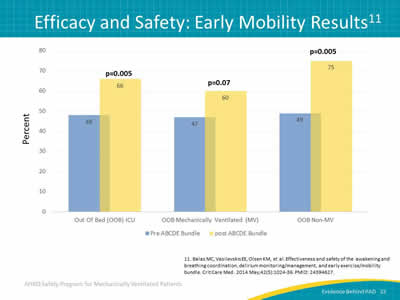
Image: Bar graph of early mobility results. The following improvements were seen after use of the ABCDE bundle: The percent of ICU patients out of bed increased from 48 to 66, percent of mechanically ventilated patients out of bed increased from 47 to 60, and the percent of non-mechanically ventilated patients out of bed increased from 49 to 75.
11. Balas MC, Vasilevskis EE, Olsen KM, et al. Effectiveness and safety of the awakening and breathing coordination, delirium monitoring/management, and early exercise/mobility bundle. Crit Care Med 2014 May;42(5):1024-36. PMID: 24394627.
Slide 24: 28-Day Mortality Results11
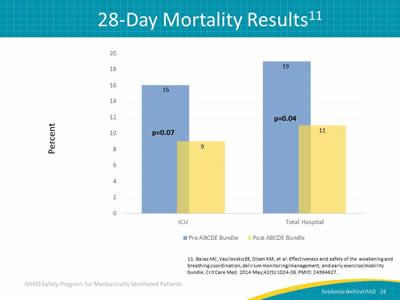
Image: Bar graph of 28-day mortality results. Mortality declined in both the total hospital and the ICU after use the ABCDE bundle, from 16 percent to 9 percent in the ICU and from 19 percent to 11 percent in the total hospital.
11. Balas MC, Vasilevskis EE, Olsen KM, et al. Effectiveness and safety of the awakening and breathing coordination, delirium monitoring/management, and early exercise/mobility bundle. Crit Care Med 2014 May;42(5):1024-36. PMID: 24394627.
Slide 25: Maslow’s Hierarchy of Needs in Critical Care12
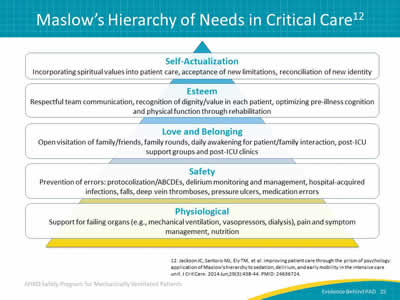
Image: Pictoral representation of Maslow's Hierarchy of Needs in critical care. Starting at the base of a pyramid and going up, the needs are physiological, safety, love and belonging, esteem, and self-actualization.
12. Jackson JC, Santoro MJ, Ely TM, et al. Improving patient care through the prism of psychology: application of Maslow's hierarchy to sedation, delirium, and early mobility in the intensive care unit. J Crit Care 2014 Jun;29(3):438-44. PMID: 24636724.
Slide 26: Questions?

Image: Group of people holding signs with question marks on them.
Slide 27: References
1. Barr J, Fraser GL, Puntillo K, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med 2013 Jan;41(1):263-306. PMID: 23269131.
2. Balas MC, Devlin JW, Verceles AC, et al. Adapting the ABCDEF bundle to meet the needs of patients requiring prolonged mechanical ventilation in the long-term acute care hospital setting: historical perspectives and practical implications. Semin Respir Crit Care Med 2016 Feb;37(1):119-35. PMID: 26820279.
3. Vasilevskis EE, Pandharipande PP, Girard TD, et al. A screening, prevention, and restoration model for saving the injured brain in intensive care unit survivors. Crit Care Med 2010 Oct;38(10 Suppl):S683-91. PMID: 21164415.
4. Zaal IJ, Spruyt CF, Peelen LM, et al. Intensive care unit environment may affect the course of delirium. Intensive Care Med 2013 Mar;29(3):481-88. PMID: 22804788.
Slide 28: References
5. Colombo R, Corona A, Praga F, et al. A reorientation strategy for reducing delirium in the critically ill. Results of an interventional study. Minerva Anestiol 2012 Sep;78(9):1026-33. PMID: 22772860.
6. ABCDEFs of Prevention and Safety. Nashville, TN: ICU Delirium and Cognitive Impairment Study Group. 2013. www.icudelirium.org. Accessed Oct 20, 2015.
7. Trogrlić Z, van der Jagt M, Bakker J, et al. A systematic review of implementation strategies for assessment, prevention, and management of ICU delirium and their effect on clinical outcomes. Crit Care 2015 Apr 9;19(1):157. PMID: 25888230.
8. Miller MA, Govindan S, Watson SR, et al. ABCDE, but in that order? A cross-sectional survey of Michigan intensive care unit sedation, delirium, and early mobility practices. Ann Am Thorac Soc 2015 Jul;12(7):1066-71. PMID: 25970737.
Slide 29: References
9. Needham DM, Korupolu R, Zanni JM, et al. Early physical medicine and rehabilitation for patients with acute respiratory failure: a quality improvement project. Arch Phys Med Rehabil 2010 Apr;91(4):536-42. PMID: 20382284.
10. Khan BA, Fadel WF, Tricker JL, et al. Effectiveness of implementing a wake up and breathe program on sedation and delirium in the ICU. Crit Care Med 2014 Dec;42(12)e791-95. PMID: 25402299.
11. Balas MC, Vasilevskis EE, Olsen KM, et al. Effectiveness and safety of the awakening and breathing coordination, delirium monitoring/management, and early exercise/mobility bundle. Crit Care Med 2014 May;42(5):1024-36. PMID: 24394627.
12. Jackson JC, Santoro MJ, Ely TM, et al. Improving patient care through the prism of psychology: application of Maslow's hierarchy to sedation, delirium, and early mobility in the intensive care unit. J Crit Care 2014 Jun;29(3):438-44. PMID: 24636724.



