Introduction to Daily Care Processes: Evidence Behind Spontaneous Awakening Trials, Spontaneous Breathing Trials, and Head of Bed Elevation: Facilitator Guide
AHRQ Safety Program for Mechanically Ventilated Patients
Slide 1: Introduction to Daily Care Processes: Evidence Behind Spontaneous Awakening Trials, Spontaneous Breathing Trials, and Head of Bed Elevation
Say:
In this module, you will be introduced to daily care processes. You will also learn about the evidence behind spontaneous awakening trials (SATs), spontaneous breathing trials (SBTs), and head of bed (HOB) elevation.
Slide 2: Learning Objectives
Say:
After this session, you will be able to identify how the use of SATs and SBTs can reduce the length of mechanical ventilation and the risk of ventilator-associated pneumonia (VAP), follow and perform the recommended SAT and SBT protocols when clinically indicated, understand the benefits of using HOB elevation techniques, and access the supporting resources for these daily care process measures.
Slide 3: SATs and SBTs
Say:
We will now discuss the efforts to reduce sedation practices using SATs and SBTs.
Slide 4: Complications of Sedation
Ask:
What complications arise from sedating patients?
Say:
Sedation suppresses respiratory drive, which prolongs ventilator dependence; impairs mobility; and increases the risk for delirium. Prolonged ventilation also carries an increased risk of potential complications such as pneumonia, atelectasis, acute respiratory distress syndrome, and deconditioning.
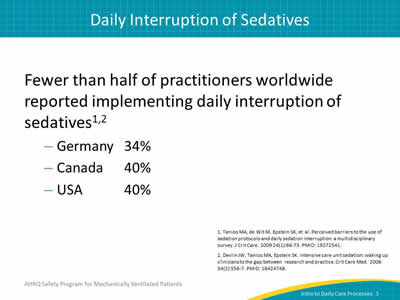
Slide 5: Daily Interruption of Sedatives
Say:
Less than half of practitioners worldwide have reported implementing daily interruption of sedatives with totals as low as 34 percent of practitioners in Germany, 40 percent of practitioners in Canada, and 40 percent of practitioners in the United States.
Slide 6: SAT & SBT Specific VAP Prevention Guidelines
Say:
The Centers for Disease Control and Prevention (CDC) does not specifically address SAT and SBT but supports sedation weaning.
The American Thoracic Society (ATS) recommends the use of daily interruption or lightening of sedation to avoid constant heavy sedation and to facilitate and accelerate weaning. However, it does not specifically address SBT.
Slide 7: SAT & SBT Specific VAP Prevention Guidelines
Say:
The Society for Healthcare Epidemiology of America (SHEA) recommends simultaneous use of daily SATs and the daily assessment of readiness wean through SBTs. It also recommends the management of ventilated patients with minimal sedation whenever possible, as well as the avoidance of benzodiazepines.
Slide 8: 2014 SHEA Compendium Update
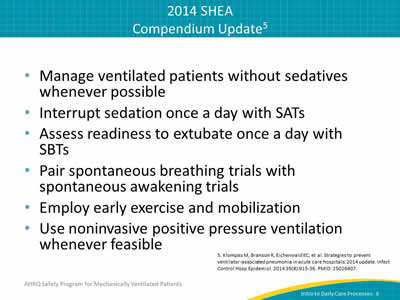
Say:
The 2014 SHEA Compendium Update suggests managing ventilated patients without sedatives whenever possible. Once a day, you should interrupt sedation with SATs as well as assess readiness to extubate with SBTs. The literature also suggests that pairing SATs and SBTs together results in better patient outcomes. Be sure to employ early exercise and mobilization for patients. Use non-invasive positive pressure ventilation whenever feasible as the primary strategy to reduce the need for putting a patient on mechanical ventilation.
Slide 9: SAT & SBT Protocol
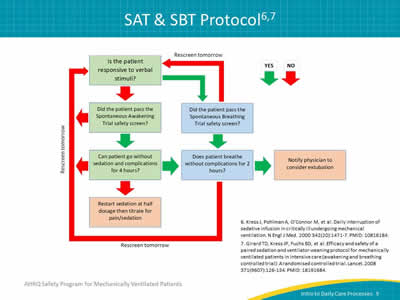
Say:
This chart uses a series of questions to assess patients for SATs and SBTs.
Is the patient responsive to verbal stimuli? If yes, did the patient pass the SBT safety screen? If yes, does the patient breathe without complications for 2 hours? If yes, notify their physician to consider extubation.
If the patient didn’t pass the SBT safety screen or cannot breathe without complications for 2 hours, rescreen them the following day.
If the patient isn’t responsive to verbal stimuli, did the patient pass the SAT safety screen? If yes, can the patient tolerate being off sedation? If yes, does the patient breathe without complications for two hours? If yes, notify their physician to consider extubation.
If the patient didn’t pass the SAT safety screen or can’t breathe without complications for two hours, rescreen them the following day.
If the patient can’t go without sedation and complications for 4 hours, restart sedation at half dosage and then titrate for pain and sedation.
Slide 10: SAT Summary
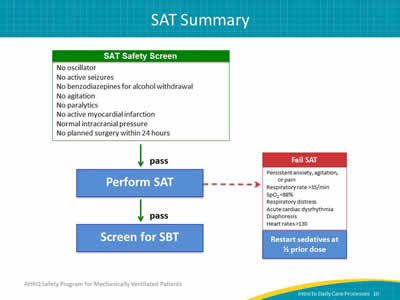
Ask:
How can we summarize this process?
Say:
Essentially, the patient undergoes the SAT safety screen. If they pass it, the SAT can be performed. The red arrow indicates the criteria for failing the SAT. If the patient passes the SAT, the SBT can be performed.
Slide 11: SAT Protocol
Say:
SATs are conducted to find the minimum amount of sedation necessary for a patient to be comfortable. SATs consist of two parts: a safety screen and a trial. The SAT safety screen checks for contraindications to performing the SAT trial. For patients who are not responsive to verbal stimuli, the SAT trial checks for contraindications to performing the SBT safety screen and SBT trial.
Slide 12: SAT Safety Screen Eligibility
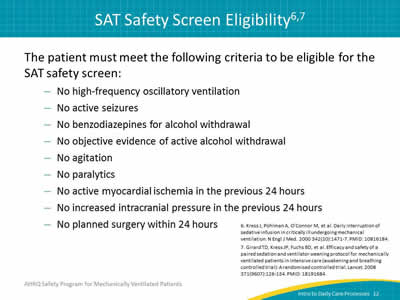
Ask:
What determines eligibility?
Say:
To be eligible for the SAT safety screen, the patient must not have been put on high-frequency oscillatory ventilation, must not experience active seizures, must not have been given benzodiazepines for alcohol withdrawal, must not have any objective evidence of active alcohol withdrawal, must not experience agitation, must not have been given paralytics, must not have had active myocardial ischemia in the previous 24 hours, must not have had any increased intracranial pressure in the previous 24 hours, and should not have any surgery planned within the next 24 hours.
Slide 13: Passing the SAT Safety Screen
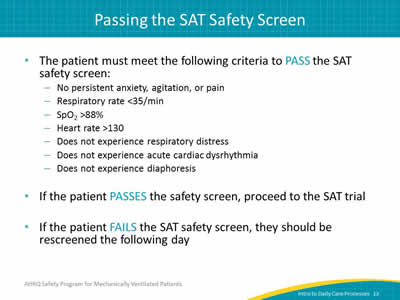
Say:
To pass the SAT safety screen, the patient must not demonstrate persistent anxiety, agitation, or pain, must have a respiratory rate of less than 35 breaths per minute, must have SpO2 that is greater than 88 percent, must have a heart rate greater than 130, must not experience any respiratory distress, must not experience acute cardiac dysrhythmia, and must not experience diaphoresis. If the patient passes the safety screen, proceed to the SAT trial. If the patient fails the SAT safety screen, they should be rescreened the following day.
Slide 14: Passing the SAT Trial
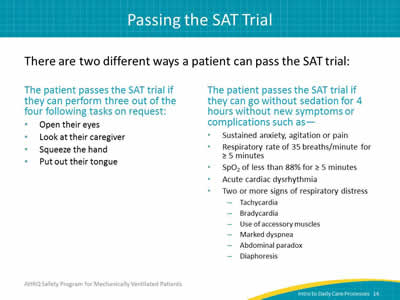
Say:
There are two different ways that a patient can pass the SAT trial. For instance, the patient will pass the SAT trial if they can perform three out of four tasks on request. These tasks include opening their eyes, looking at their caregiver, squeezing their caregiver’s hand, and putting out their tongue. The patient will also pass the SAT trial if they can go without sedation for 4 hours without new symptoms or complications such as sustained anxiety, any agitation or pain, a respiratory rate of 35 breaths per minute for 5 minutes or more, SpO2 of less than 88 percent for 5 minutes or more, and acute cardiac dysrhythmia. The patient must also not demonstrate any more than one of the signs of respiratory distress such as tachycardia, bradycardia, the use of accessory muscles, marked dyspnea, abdominal paradox, or diaphoresis.
Slide 15: Passing the SAT Trial
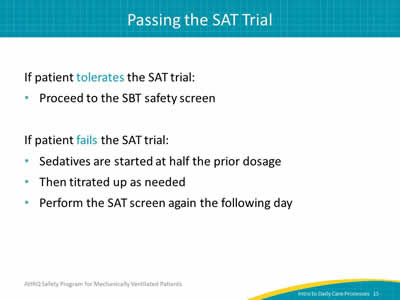
Say:
If the patient tolerates the SAT trial, they may proceed to the SBT safety screen. If the patient fails the SAT trial, sedatives are started at half the prior dosage and are then titrated up as needed. Perform the SAT screen on that patient again the following day.
Slide 16: SBT Safety Screen
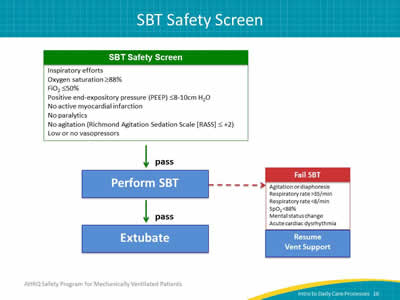
Say:
This slide should look very similar to the SAT summary. The patient undergoes the SBT safety screen. If they pass it, the SBT can be performed. The red arrow indicates the criteria for failing the SBT. If the patient passes the SBT, their physician should be informed so that the patient can be evaluated for extubation.
Slide 17: SBT Protocol
Say:
SBTs are conducted in an effort to remove patients from ventilator support. SBTs consist of two parts: a safety screen and a trial. The SBT safety screen checks for contraindications to performing the SBT trial. The SBT trial checks for contraindications to considering the extubation of the patient.
Slide 18: Passing the SBT Safety Screen
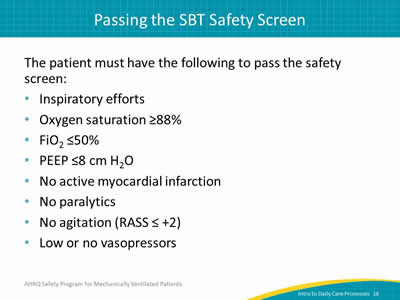
Say:
To pass the safety screen, the patient must demonstrate inspiratory efforts, must have an oxygen saturation of 88 percent or greater, must have FiO2 no greater than 50 percent, must have a PEEP value less than 8 to 10 centimeters of water, must not have an active myocardial infarction, must not be on paralytics, must not experience agitation which, according to RASS, is measured by a score of +2 or higher, and must be on low or no vasopressors.
Slide 19: Passing the SBT Trial
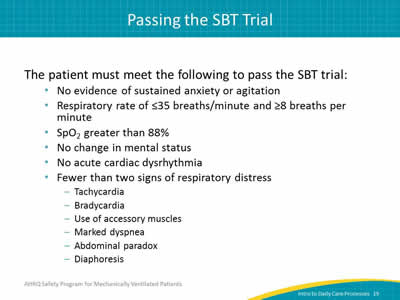
Say:
To pass the SBT trial, the patient must not demonstrate any evidence of sustained anxiety or agitation. The patient must also have a respiratory rate of less than 35 breaths per minute, and of at least 8 breaths per minute, and they must have sustained SpO2 greater than 88 percent. The patient must not experience any change in mental status, must not have acute cardiac dysrhythmia, and must not demonstrate any more than one of the signs of respiratory distress such as tachycardia, bradycardia, the use of accessory muscles, marked dyspnea, abdominal paradox, and diaphoresis.
Slide 20: Failing the SBT trial
Say:
If the patient fails the SBT trial, they should be re-ventilated immediately. They should be reassessed the following day. However, if the patient passes the SBT trial, notify their physician to consider performing extubation.
Slide 21: Perceived Barriers to Sedation Protocols and SATs
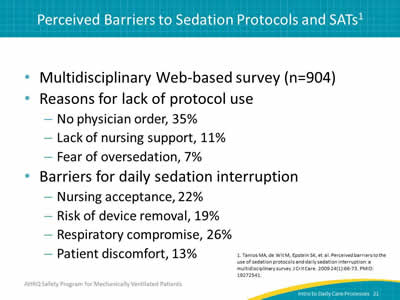
Say:
Despite the benefits of sedation protocols and SATs that we discussed earlier, a variety of perceived barriers contribute to their lack of use. A multidisciplinary Web-based survey of 904 clinicians reported several reasons for the lack of protocol use. Thirty-five percent of the respondents reported that lack of a physician order was a barrier, 11 percent reported lack of nursing support, and 7 percent reported a fear of over-sedation. This survey also reported several barriers for daily sedation interruption. 22 percent of respondents reported that lack of nursing acceptance was a barrier, 19 percent reported risk of device removal as a barrier, 26 percent reported concerns about respiratory comprise, and 13 percent reported patient discomfort as a barrier to use of daily sedation interruption.
Slide 22: Intensive Care Unit (ICU) Barriers to SATs
Ask:
What are some of the barriers to SATs?
Say:
ICU barriers include viewing SATs as unnecessary and considering light sedation as more appropriate and safer for patients. These barriers also include lack of physician orders, inadequate staff to undertake protocols, and staff remaining unconvinced that lowering sedation will benefit patients.
Slide 23: ICU Barriers to SATs
Say:
Nursing attitudes account for one-third of the variance in the number of patients who received sedatives. In this U.S. study, only 17.7 percent of respondents thought it was easier to care for an awake and alert patient receiving mechanical ventilation than to care for a similar patient who was more sedated.
Slide 24: Evidence for SATs and SBTs
Say:
We will now discuss the evidence and studies in support of SATs and SBTs.
Slide 25: Strøm et al.
![A protocol of no sedation for critically ill patients receiving mechanical ventilation: a randomised trial. 140 patients randomized to routine sedation versus no sedation: 70 prescribed routine sedation (propofol then midazolam). 70 prescribed no sedation (morphine boluses as needed). Patients with no sedation: Mean 4.2 (95% confidence interval [CI] 0.3 to 8.1) fewer days on ventilation. Shorter ICU stay (hazard ratio [HR] 1.86, 95% CI 1.1 to 3.2). Shorter hospital stay (HR 3.6, 95% CI 1.5 to 9.1). More agitated delirium (20% vs. 7%) but no difference in self-extubations. 1:1 nursing.](/sites/default/files/wysiwyg/professionals/quality-patient-safety/hais/tools/mvp/modules/technical/intro-dailycare/intro-dailycare-slide25.jpg)
Say:
First, let’s look at the concept of no sedation. A protocol of no sedation for critically ill patients receiving mechanical ventilation was tested in a randomized trial. In this trial, 140 patients were randomized and given either routine sedation or no sedation at all. Seventy were prescribed sedation, using propofol and then midazolam, while 70 were prescribed no sedation. For those not receiving sedation, morphine boluses were used as needed. The patients with no sedation spent a mean of 4.2 fewer days on mechanical ventilation and also decreased their time spent in the ICU as well as in the hospital. However, there was no change in mortality rates. Patients in the no sedation group did experience more agitated delirium but experienced no difference in the rate of self-extubations. This study shows that a patient on mechanical ventilation can be maintained without sedation.
Slide 26: Kress et al.
Say:
No sedation has not historically been standard of care in the United States, so more attention has been given to the interruption and minimization of sedation. This landmark study from Kress et al., published in 2000, evaluated daily sedative interruptions, later called SATs, for mechanically ventilated patients. Patients who underwent daily interruption of sedation had 2.4 more days off the ventilator and were almost twice as likely to be extubated than those in the control group. ICU length of stay was shorter by 3.5 days. There was also a decreased need for neurologic evaluations such as computed tomography (CT) scans in the intervention group.
Slide 27: Girard et al.
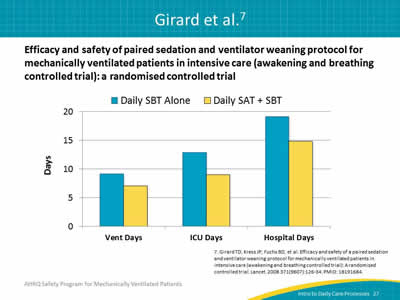
Say:
Later, another randomized trial, specifically the Awakening and Breathing Controlled trial, studied the efficacy and safety of paired sedation and ventilator weaning protocol for mechanically ventilated patients in intensive care. This bar graph shows that implementing daily SATs and SBTs in coordination decreased days of ventilation by 2 days, days spent in the ICU by 4 days, and days spent in the hospital by 4 days when compared with the daily implementation of SBTs alone. There was also a 14 percent absolute reduction in mortality at 1 year for patients who received the intervention. To maximize the patient’s chance of passing their SBT, perform the SBT without sedation so they are as awake as possible.
Slide 28: Wake Up and Breathe
Say:
We will now discuss the Wake Up and Breathe Collaborative.
Slide 29: CDC Prevention Epicenters' Wake Up and Breathe Collaborative
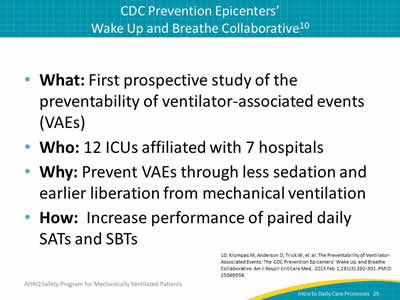
Ask:
What is the Wake Up and Breathe Collaborative?
Say:
The Wake Up and Breathe Collaborative performed the first prospective study of the preventability of ventilator-associated events (VAEs), which are defined by changes in patients' ventilator settings. This 19-month collaborative consisted of 12 ICUs, encompassing surgical, medical, and mixed units, and was affiliated with seven hospitals, including academic hospitals, a VA hospital, and community hospitals. Its purpose was to prevent VAEs through less sedation and earlier patient liberation from mechanical ventilation by increasing the performance of paired daily SATs and SBTs.
Slide 30: CDC Prevention Epicenters' Wake Up and Breathe Collaborative
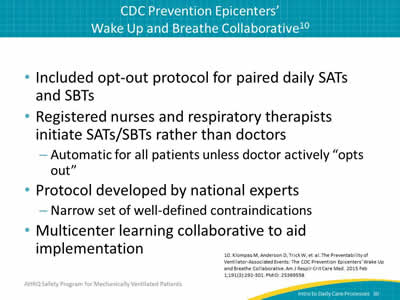
Say:
The Wake Up and Breathe Collaborative included an opt-out protocol for paired daily SATs and SBTs. Registered nurses and respiratory therapists would initiate the SATs and SBTs instead of doctors. This was done automatically for all patients unless the doctor actively "opted out" for a patient that they didn’t believe was suitable. This protocol was developed by national experts with a narrow set of well-defined contraindications. Ultimately, the Wake Up and Breathe Collaborative was a multicenter learning collaborative meant to aid implementation by influencing practice change, cultural change, and behavioral change.
Slide 31: CDC Prevention Epicenters' Wake Up and Breathe Collaborative
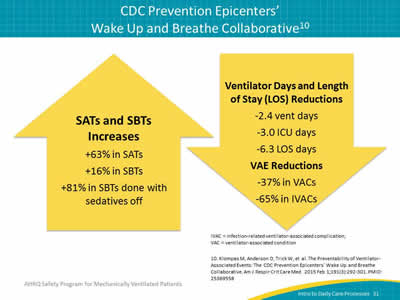
Say:
Here are the changes in performance rates of SATs and SBTs over time. This slide shows a 63 percent increase in SATs, a 16 percent increase in SBTs, and an 81 percent increase in SBTs performed with no sedation. These changes were associated with a 37 percent decrease in VAEs, 65 percent decrease in IVACs, a 2.4 day decrease in mechanical ventilation, a 3 day decrease in ICU length of stay, and a 6 day decrease in length of stay. This emphasizes that SATs and SBTs are effective in reducing VAE rates as well as the duration of mechanical ventilation and length of stay.
Sometimes, we may find it difficult to objectively determine whether we think a patient will pass an SBT. This difficulty may prevent us from attempting to perform the trial all together. And it brings to light the additional importance of the SAT—it allows the clinician to more accurately assess whether someone might pass the SBT. This embodies the larger mission of the Wake Up and Breathe Collaborative, which is to get people to challenge their assumptions. Let the patient tell you what they can tolerate in terms of minimal sedation, and what they can tolerate in terms of the need for mechanical ventilation.
Slide 32: Resources: SAT and SBT Fast Facts
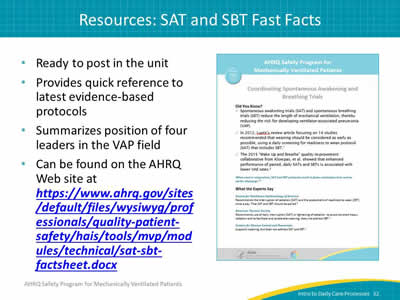
Say:
The AHRQ Safety Program for Mechanically Ventilated Patients provides many tangible resources you can use to educate and reinforce sedation protocols. An SAT and SBT "fast facts" guide is available on the AHRQ Web site here (Word File, 1.59 MB) and as shown on the slide, and is ready to be posted in your unit. It provides a quick reference to the latest evidence-based protocols as well as summarizes the position of four leaders in the VAP field.
Slide 33: Resources: SAT and SBT Literature Review
Say:
An SAT and SBT literature review is also available on the AHRQ Web site here (Word File, 1.6 MB) and as shown on the slide and is ready to be posted in your unit. It provides a quick reference to the latest evidence-based protocols as well as summarizes the position of four leaders in the VAP field.
Slide 34: HOB Elevation
Say:
We will now discuss HOB elevation.
Slide 35: HOB Elevation
Say:
HOB elevation to a semi-recumbent position, greater than 30 degrees, is associated with a decreased incidence of aspiration and VAP. A study showed that both the supine position and length of time the patient is kept in this position are potential risk factors for the aspiration of gastric contents.
Slide 36: HOB Elevation
Say:
Several successful strategies have been used to improve compliance with HOB elevation of at least 30 degrees. These include the use of a bed with a specific attachment that will show the angle at a glance, the use of a handheld protractor, and a determination of what mark on which bed can signify the correct angle for recline. HOB elevation data should be fed back to unit staff on a regular basis. You should involve everyone who cares for the patient, including family members, to ensure the HOB is maintained at the correct angle. The intervention is supported unanimously by all four leading guidelines, and newer publications in the field accept the head of bed as an effective, low cost, and low risk intervention.
Slide 37: HOB Specific VAP Prevention Guidelines
Say:
SHEA recommends the use of a semi-recumbent position, between 30 and 45 degrees, as a strategy to prevent aspiration.
ZAP the VAP: Ventilator Associated Pneumonia recommends the HOB elevation to be 45 degrees, as long as it’s not contraindicated.
Slide 38: HOB Specific VAP Prevention Guidelines
Say:
The CDC recommends that in the absence of medical contraindication(s), HOB elevation should be at an angle between 30 and 45 degrees for patients with a high risk for aspiration, such as a person receiving mechanically assisted ventilation.
ATS recommends that patients should be kept in a semi-recumbent position, between 30 and 45 degrees, rather than supine to prevent aspiration.
Slide 39: Resources: HOB Literature Review
Say:
The HOB literature review can be found on the AHRQ Web site here (Word File, 1.6 MB) and as shown on the slide and is ready to be posted in your unit. It provides a quick reference to the latest evidence-based protocols as well as summarizes the position of four leaders in the VAP field.
Slide 40: Questions?

Ask:
Are there any questions?
Slide 41: References
Slide 42: References