Potentially Avoidable Hospitalizations
Potentially avoidable hospitalizations, by race/ethnicity, stratified by area income, 2013
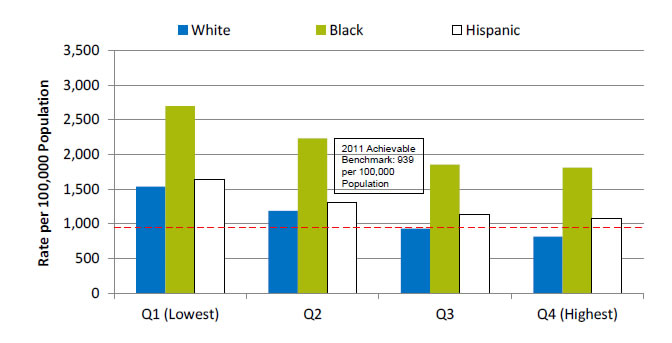
| Quartile | White | Black | Hispanic |
|---|---|---|---|
| Q1 (Lowest) | 1536.3 | 2695.9 | 1641.5 |
| Q2 | 1187.6 | 2230.4 | 1309 |
| Q3 | 930.3 | 1855 | 1131.4 |
| Q4 (Highest) | 815.2 | 1810.9 | 1085 |
2011 Achievable Benchmark: 939 per 100,000 Population.
Key: Q = quartile. based on the median income of a patient's ZIP Code of residence.
Source: Agency for Healthcare Research and Quality (AHRQ), Healthcare Cost and Utilization Project, State Inpatient Databases, 2013 quality and disparities analysis file, and AHRQ Quality Indicators, modified version 4.4.
Note: Rates are adjusted by age and gender using the total U.S. resident population for 2010 as the standard population.
- Groups With Disparities: In 2013, in all income groups, rates of potentially avoidable hospitalizations were higher for Blacks than for Whites. Rates for Whites in the lowest income quartile were lower than the rates for Blacks in the highest income quartile.
- Achievable Benchmark:
- In 2011, the top 4 State achievable benchmark for all potentially avoidable hospitalizations was 939 per 100,000 population. The States that contributed to the achievable benchmark are Hawaii, Oregon, Utah, and Washington.
- Whites in the two highest income quartiles have already achieved the benchmark. No other groups have achieved the benchmark.
Provider Ability To Share Medical Information Electronically
Patients who reported that it was very important to them that their doctors and other health care providers be able to share their medical information electronically, by race/ethnicity, 2008-2014
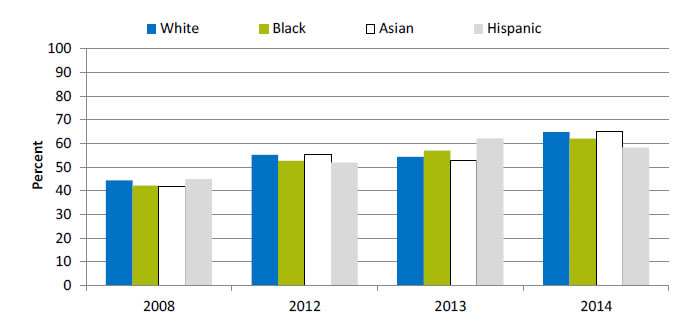
| Race | 2008 | 2012 | 2013 | 2014 |
|---|---|---|---|---|
| White | 44.4 | 55.2 | 54.3 | 64.8 |
| Black | 42.2 | 52.7 | 57 | 62.1 |
| Asian | 41.7 | 55.3 | 52.9 | 64.9 |
| Hispanic | 44.9 | 51.9 | 62.2 | 58.3 |
Source: Health Information National Trends Survey. Iterations included in this graph are HINTS 3, HINTS 4 Cycle 1, and HINTS 4 Cycle 2. Available at http://hints.cancer.gov/.
- Trends: From 2008 to 2014, the percentage of Black, White, Asian, and Hispanic patients who reported that it was very important that their doctors and other health care providers be able to share their medical information electronically increased significantly.
- Groups With Disparities: In 2014, there were no statistically significant differences between Blacks and Whites in the percentage who reported that it was very important that their doctors and other health care providers be able to share their medical information electronically.
Patient Electronic Access to Medical Information
Patients who reported that it was very important for them to be able get their own medical information electronically, 2008-2014
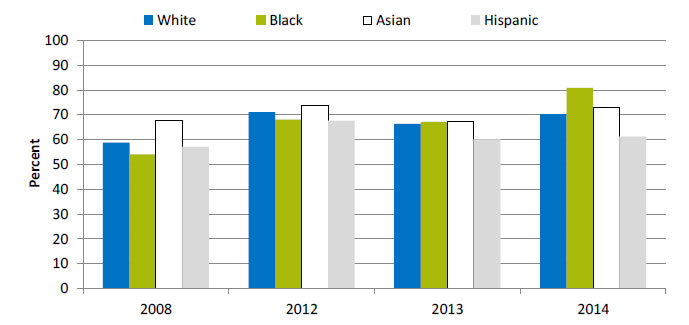
| Race | 2008 | 2012 | 2013 | 2014 |
|---|---|---|---|---|
| White | 58.8 | 71.1 | 66.4 | 70.3 |
| Black | 54.1 | 68.1 | 67.2 | 80.9 |
| Asian | 67.6 | 73.8 | 67.2 | 73 |
| Hispanic | 57.1 | 67.6 | 60.2 | 61.2 |
Source: Health Information National Trends Survey. Iterations included in this graph are HINTS 3, HINTS 4 Cycle 1, and HINTS 4 Cycle 2. Available at http://hints.cancer.gov/.
- Trends: From 2008 to 2014, the percentage of Black patients who reported that it was very important to be able to get their medical information electronically increased from 54.1% to 80.9%; for Whites, the percentage increased from 58.8% to 70.3%.
- Groups With Disparities: In 2014, the percentage of patients who reported that it was very important to be able to get their medical information electronically was 80.9% for Blacks, 70.3% for Whites, 73.0% for Asians, and 61.2% for Hispanics.
Willingness To Exchange Medical Information Electronically
Patients who reported that they were very willing to exchange medical information with their health care provider electronically, by race/ethnicity, 2013
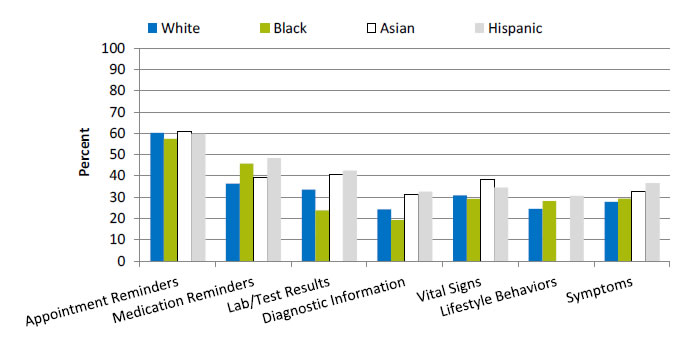
| Type of Information | White | Black | Asian | Hispanic |
|---|---|---|---|---|
| Appointment Reminders | 60.2 | 57.4 | 61 | 59.8 |
| Medication Reminders | 36.4 | 45.8 | 39.1 | 48.4 |
| Lab/Test Results | 33.5 | 23.8 | 40.8 | 42.4 |
| Diagnostic Information | 24.2 | 19.3 | 31.4 | 32.6 |
| Vital Signs | 30.9 | 29.2 | 38.5 | 34.4 |
| Lifestyle Behaviors | 24.6 | 28.1 | 30.6 | |
| Symptoms | 27.8 | 29.3 | 32.6 | 36.6 |
Source: Health Information National Trends Survey. Iterations included in this table are; HINTS 3, HINTS 4 Cycle 1, and HINTS 4 Cycle 2. Available at http://hints.cancer.gov/.
Note: Data for Asians for Lifestyle Behaviors were statistically unreliable.
- Groups With Disparities:
- The percentage of patients very willing to exchange appointment reminders electronically was higher for Whites (60.2%) and Asians (61.0%) than for Blacks (57.4%) and Hispanics (59.8%).
- The percentage of patients very willing to exchange medication reminders electronically was higher for Blacks (45.8%) and Hispanics (48.4%) than for Whites (36.4%) and Asians (39.1%).
- The percentage of patients very willing to exchange lab/test results electronically was lower for Blacks (23.8%) than for Whites (33.5%), Asians (40.8%), and Hispanics (42.4%).
- The percentage of patients very willing to exchange diagnostic information (e.g., medical illnesses) electronically was lower for Blacks (19.3%) than for Whites (24.2%), Asians (31.4%), and Hispanics (32.6%).
- The percentage of patients very willing to exchange vital signs (e.g., heart rate, blood pressure, glucose levels) electronically was lower for Blacks (29.2%) and Whites (30.9%) than for Asians (38.5%) and Hispanics (34.4%).
- The percentage of patients very willing to exchange lifestyle behaviors (e.g., physical activity, food intake, sleep patterns) electronically was higher for Blacks (28.1%) and Hispanics (30.6%) than for Whites (24.6%).
- The percentage of patients very willing to exchange symptoms (e.g., nausea, pain, dizziness) electronically was higher for Hispanics (36.6%) and Asians (32.6%) than for Blacks (29.3%) and Whites (27.8%).
AHRQ Health Care Innovations in Care Coordination
- Population: Low-income individuals with serious and persistent mental illness.
- Location: Atlanta, Georgia.
- Intervention: Case managers assist patients with severe mental illnesses in accessing needed preventive, primary, and specialty medical services. Between visits care managers monitor patients’ progress, provide additional support, and coordinate with primary care and mental health clinicians.
- Outcomes: Enhanced access to needed preventive primary care and specialty medical services, leading to improved physical and mental health. Also reduced cost of care.
Return to Contents
Return to National Quality Strategy Priorities



