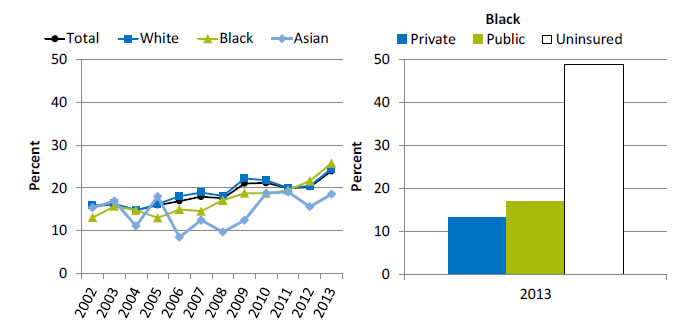
Lack of Usual Source of Care Due to Cost
People without a usual source of care who indicate a financial or insurance reason for not having a source of care, by race, 2002-2013, and by insurance, Blacks, 2013
Left Chart:
| Race | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | 15.6 | 16.3 | 14.8 | 16.0 | 17.0 | 18.0 | 17.6 | 21.1 | 21.2 | 19.9 | 20.2 | 24 |
| White | 15.9 | 16.3 | 14.7 | 16.3 | 18.1 | 19.0 | 18.1 | 22.2 | 21.8 | 20.0 | 20.5 | 24.5 |
| Black | 13.1 | 15.7 | 14.8 | 13.0 | 15.0 | 14.6 | 17.1 | 18.8 | 18.8 | 19.5 | 21.7 | 25.8 |
| Asian | 15.4 | 16.9 | 11.1 | 18.0 | 8.5 | 12.5 | 9.7 | 12.5 | 18.8 | 19.1 | 15.6 | 18.6 |
Right Chart (Insurance, Blacks, 2013):
- Private - 13.1.
- Public - 16.9.
- Uninsured - 48.8.
Source: Agency for Healthcare Research and Quality, Medical Expenditure Panel Survey, 2002-2012.
Denominator: Civilian noninstitutionalized population without a usual source of care.
Note: For this measure, lower rates are better.
- Importance: High-quality health care is facilitated by having a regular provider, but some Americans may not be able to afford one.
- Overall Rate: In 2013, 24% of people without a usual source of care indicated a financial or insurance reason for not having a source of care.
- Trends: The percentage worsened overall (15.6% to 24%) and among Blacks (13.1% to 25.8%) and Whites (15.9% to 24.5%).
- Groups With Disparities: In 2013, the percentage of people without a usual source of care who indicated a financial or insurance reason for not having a source of care was higher among uninsured Blacks (48.8%) compared with Blacks with private insurance (13.1%).
AHRQ Health Care Innovations in Reducing Costs
Methodist Le Bonheur Healthcare
- Location: Memphis, Tennessee.
- Intervention: The Congregational Health Network, a partnership between Methodist Le Bonheur Healthcare and 512 congregations in Memphis, supports the transition from hospital to home for church members. A hospital-employed navigator visits the patient to determine his or her needs and then works with a church-based volunteer liaison to arrange postdischarge services and facilitate the transition to the community.
- Outcomes: Reduced mortality, health care costs and charges, inpatient utilization, readmission rates, and time to readmission. Increased referrals to home health and hospice care and improved satisfaction with hospital care.
Return to Contents
Return to National Quality Strategy Priorities



