- Most measures of Effective Treatment tracked in the QDR relate to priorities of the Heckler Report. Here, we illustrate effective treatment of conditions tracked in the QDR that were not priorities in the Heckler Report:
- Chronic kidney diseases.
- Musculoskeletal diseases.
- Respiratory diseases.
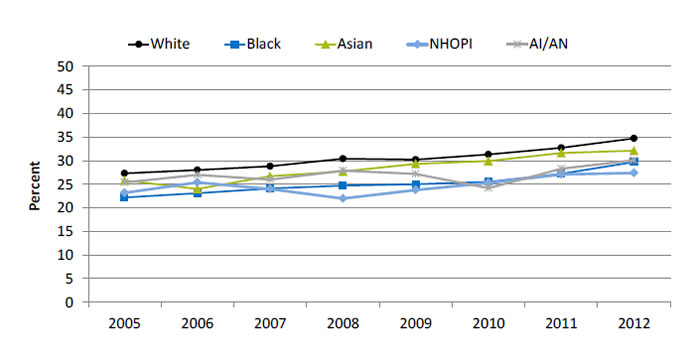
Nephrologist Visit Before Renal Replacement Therapy
Patients who saw a nephrologist at least 12 months prior to initiation of renal replacement therapy, by race 2005-2012
| Race | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 |
|---|---|---|---|---|---|---|---|---|
| White | 27.3 | 28.0 | 28.8 | 30.4 | 30.2 | 31.3 | 32.7 | 34.7 |
| Black | 22.2 | 23.1 | 24.1 | 24.7 | 25.0 | 25.5 | 27.2 | 29.7 |
| Asian | 25.8 | 24.0 | 26.7 | 27.7 | 29.3 | 29.9 | 31.6 | 32.1 |
| AI/AN | 25.4 | 27.0 | 26 | 27.9 | 27.2 | 24.2 | 28.3 | 30.1 |
| NHOPI | 23.2 | 25.4 | 24 | 22.0 | 23.8 | 25.3 | 27.1 | 27.4 |
Key: NHOPI = Native Hawaiian or Other Pacific Islander; AI/AN = American Indian or Alaska Native.
Source: U.S. Renal Data System, 2005-2012. http://www.usrds.org/2014/view/v2_02.aspx.
Note: This graph uses data from the newest version of the ESRD Medical Evidence CMS 2278 form. The cohorts include incident hemodialysis patients. Includes only patients for whom it is known whether they saw a nephrologist prior to initiation.
- Importance:
- Early referral to a nephrologist is important for patients with progressive chronic kidney disease who are approaching kidney failure.
- Patients who begin nephrology care more than a year before kidney failure are less likely to begin dialysis with a catheter, experience infections related to vascular access, or die during the months after dialysis initiation (USRDS, 2013).
- Groups With Disparities: From 2009 to 2012, the percentage of end stage renal disease (ESRD) patients who began nephrology care at least 12 months prior to initiation of renal replacement therapy was higher for White and Asian patients than for Black, Native Hawaiian and Other Pacific Islander, and American Indian and Alaska Native patients.
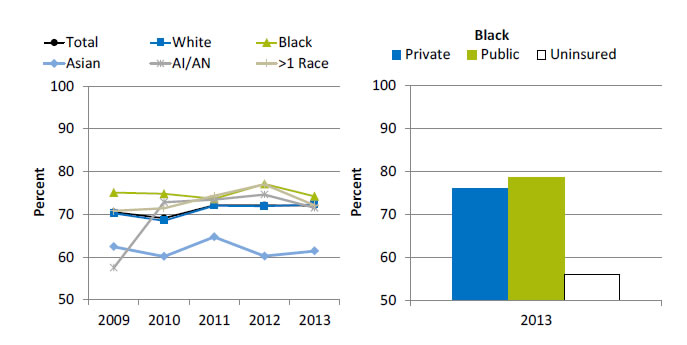
Doctor Visits for Chronic Joint Symptoms
Adults with chronic joint symptoms who have ever seen a doctor or other health professional for joint symptoms, by race, 2009-2013, and by insurance, Blacks, 2013
Left Chart:
| Race | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|
| Total | 70.5 | 69.1 | 72.1 | 72.1 | 72.0 |
| Black | 75.1 | 74.8 | 73.6 | 77.1 | 74.2 |
| White | 70.2 | 68.5 | 72.0 | 71.9 | 72.3 |
| AI/AN | 57.5 | 72.8 | 73.4 | 74.6 | 71.5 |
| Asian | 62.4 | 60.1 | 64.7 | 60.2 | 61.4 |
| >1 Race | 70.8 | 71.4 | 74.3 | 77.0 | 72.1 |
Right Chart (Insurance, Blacks, 2013):
- Private - 76.
- Public - 78.7.
- Uninsured - 55.9.
Key: AI/AN = American Indian or Alaska Native.
Source: Centers for Disease Control and Prevention, National Center for Health Statistics, National Health Interview Survey, 2009-2013.
Note: Racial groups refer to single race (e.g., White only).
- Overall: In 2013, 72% of adults with chronic joint symptoms reported seeing a doctor or other health professional for joint symptoms.
- Trends: There were no statistically significant improvements overall or among any racial group.
- Groups With Disparities:
- In 3 of 5 years, Blacks were more likely than Whites to report seeing a doctor or other health professional for joint symptoms.
- In 3 of 5 years, Asians were less likely than Whites to report seeing a doctor or other health professional for joint symptoms.
- In 2013, uninsured Blacks (55.9%) were less likely than privately insured Blacks (76%) to report seeing a doctor or other health professional for joint symptoms.
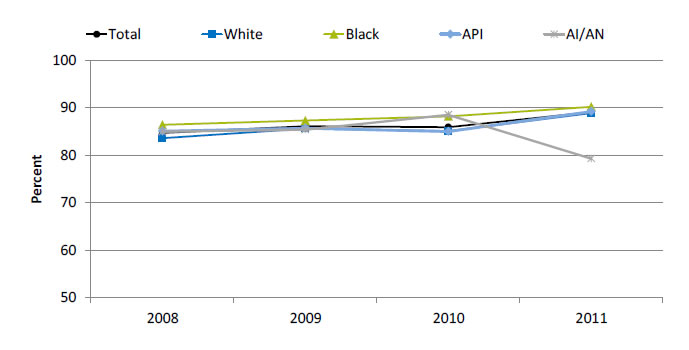
Completion of Tuberculosis Treatment
Patients with tuberculosis who completed a curative course of treatment within 1 year of initiation of treatment, by race, 2008-2011
| Race | 2008 | 2009 | 2010 | 2011 |
|---|---|---|---|---|
| Total | 84.7 | 86.1 | 85.9 | 89.1 |
| Black | 86.4 | 87.3 | 88.2 | 90.2 |
| White | 83.6 | 85.6 | 85.1 | 88.9 |
| API | 85.1 | 85.7 | 85.0 | 89.2 |
| AI/AN | 85.0 | 85.4 | 88.5 | 79.3 |
Key: API = Asian or Pacific Islander; AI/AN = American Indian or Alaska Native.
Source: Centers for Disease Control and Prevention, National Tuberculosis Surveillance System, 2008-2011.
Denominator: U.S. civilian noninstitutionalized population treated for tuberculosis.
- Overall: In 2011, 89.1% patients with tuberculosis completed a curative course of treatment within 1 year of initiation of treatment.
- Trends: From 2008 to 2011, there were improvements overall (84.7% to 89.1%) and among Blacks (86.4% to 90.2%) and Whites (83.6% to 88.9%) in the percentage of patients with tuberculosis who completed a curative course of treatment within 1 year of initiation of treatment.
- Groups With Disparities:
- In 2 of 4 years, Blacks were more likely than Whites to have completed a curative course of treatment within 1 year of initiation.
- In 2011, AI/ANs (79.3%) were less likely than Whites (88.9%) to have completed a curative course of treatment within 1 year of initiation.
AHRQ Health Care Innovations in Asthma Care
Blue Cross Blue Shield of Minnesota
- Population: Black and Latino children between 2 and 18.
- Location: Milwaukee, Wisconsin.
- Intervention: Parents of Black and Latino asthmatic children are paired with trained, culturally competent parent mentors to help them understand and care for their children’s asthma. Parent mentors conduct home visits, phone parents monthly, and meet monthly with groups of children and their families at community sites to educate and support.
- Outcomes: Improved parents’ ability to recognize when their child’s breathing problems could be controlled at home. Significantly reduced wheezing, asthma exacerbations, missed school and parent work days, and ED visits. Also led to significant cost savings for participants.
Return to Contents
Return to National Quality Strategy Priorities



